You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit.
How long do you have to submit a claim to Medicare?
Medicare Part A and B claims are submitted directly to Medicare by the healthcare provider (such as a doctor, hospital, or lab). Medicare then takes approximately 30 days to process and settle each claim. However, if there are queries or issues with the claim, the process can be a lot longer.
How do providers submit claims to Medicare?
- Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. ...
- View the Electronic Filing Instructions
- Palmetto GBA Interactive CMS-1500 Claim Form Instructions — This resource can also be helpful to providers who submit electronic claims. ...
How long does Medicaid have to file a claim?
The administrator of the Medicaid estate recovery program must present a claim for estate recovery to the person responsible for the estate within 90 days after the date on which the Medicaid estate recovery notice form is received or one year after the decedent's death, whichever is later.
How do I submit a claim to Medicare?
Generally, you’ll need to submit these items:
- The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB])
- The itemized bill from your doctor, supplier, or other health care provider
- A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the ...
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
How are hospitals reimbursed by Medicare?
Hospitals are reimbursed for the care they provide Medicare patients by the Centers for Medicare and Medicaid Services (CMS) using a system of payment known as the inpatient prospective payment system (IPPS).
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Where do I send Medicare claims?
Medicare All state claim address and phone number list, if any modification please comment it....Medicare claim address, phone numbers, payor id – revised list.StateArizonaIVR #1-877-908-8431Claim mailing addressMedicare Part B P.O. Box 6704 Fargo, ND 58108-6704Appeal addressMedicare Part B PO Box 6704 Fargo, ND 58108-6704Online resourcewww.noridianmedicare.com22 more columns
What does Medicare cover in hospital?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.
How Long Does Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
Can Medicare claims be done online?
If you can't claim at the doctor's office, you can submit a Medicare claim online using either: your Medicare online account through myGov. the Express Plus Medicare mobile app.
How long does a Medicare claim take?
It can take us up to 7 days to process your claim. When you've submitted your claim, you can select: Download claim summary to view a PDF of the claim you just made. Make another claim.
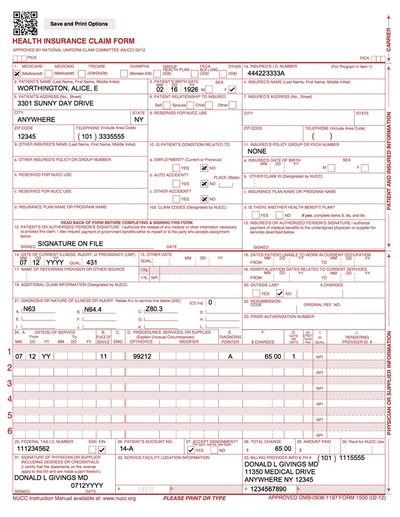
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
How do I write to Medicare?
If you're enrolled in Medicaid, contact your State or local Medicaid office....If you want Medicare information in an accessible format, you can:Call 1-800-MEDICARE (1-800-633-4227). ... Email us at [email protected] us a fax at 1-844-530-3676.More items...•
Does Medicare accept secondary paper claims?
Currently, Medicare does not accept electronically filed claims when there is more than one payer primary to Medicare. Claims that involve more than one primary payer to Medicare must be submitted on the 1500 paper claim form, with all appropriate attachments.
How do I submit a 1500 claim to Medicare?
CMS-1500 should be submitted with the appropriate resubmission code (value of 7) in Box 22 of the paper claim with the original claim number of the corrected claim. Include a copy of the original Explanation of Payment (EOP) with the original claim number for which the corrected claim is being submitted.
How does Medicare reimburse for inpatient hospital stays?
Inpatient hospitals (acute care): Medicare pays hospitals per beneficiary discharge, using the Inpatient Prospective Payment System. The base rate for each discharge corresponds to one of over 700 different categories of diagnoses—called Diagnosis Related Groups (DRGs)—that are further adjusted for patient severity.
What is Medicare DRG reimbursement?
Diagnosis-Related Group Reimbursement. Diagnosis-related group reimbursement (DRG) is a reimbursement system for inpatient charges from facilities. This system assigns payment levels to each DRG based on the average cost of treating all TRICARE beneficiaries in a given DRG.
How has DRG changed hospital reimbursement?
The introduction of DRGs shifted payment from a “cost plus profit” structure to a fixed case rate structure. Under a case rate reimbursement, the hospital is not paid more for a patient with a longer length of stay, or with days in higher intensity units, or receiving more services.
What is a Medicare claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hos...
Who files Medicare claims?
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nur...
When do I need to file Medicare claim?
Original Medicare has both participating and non-participating providers. Participating providers accept Medicare’s reimbursement plus your coinsur...
How long do I have to file a claim?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for w...
What should I do if my provider doesn’t file my claim?
Before receiving care, ask your provider’s office whether they will submit your bill to Original Medicare. While they aren’t required to do so, som...
Are claim filing requirements different if I have Medicare Advantage or Medigap?
If you have Medicare Advantage, providers in the plan’s network have to bill your insurer for your care. As mentioned above, you may have to submit...
What if I’ve already paid for my care?
You may have already paid in full for your care when you filed your claim. Be sure to note that you’ve paid on your submission, so Medicare or your...
Do I need to file Part D claims?
Medicare Part D plans contract with pharmacies where you can fill your prescriptions. Both preferred and non-preferred pharmacies can bill your Par...
How do I check on my claim to make sure it was processed?
Original Medicare beneficiaries should receive an MSN every three months detailing their recent Medicare claims. Medicare Advantage and Part D enro...
How should I ensure my claims are also filed with Medicaid?
Many Medicare beneficiaries also qualify for Medicaid due to having limited incomes and resources. Medicaid pays for Medicare co-pays, deductibles...
How to file a claim for Medicare?
How to File a Medicare Claim Yourself. If you need to file your own Medicare claim, you’ll need to fill out a Patient Request for Medical Payment Form, the 1490S. Make sure it’s filed no later than 1 full calendar year after the date of service. Medicare can’t pay its share if the submission doesn’t happen within 12 months.
Who Submits Medicare Claims?
For the most part, your doctor will submit claims to Medicare. But, in some instances, like foreign travel or doctors that don’t accept the coverage, you’ll file the claim. If you receive an Advance Beneficiary Notice of Noncoverage and decide to proceed, it’s best to request your doctor submit the claim to Medicare before billing you.
How Are Medicare Claims Processed?
Then, Medicare will take about 30 days to process the claim. When it comes to Part A services, Medicare will pay the hospital directly.
What Does Medicare Adjustment Mean?
Adjustment claims will be submitted when changing the information on a previous claim is necessary. The change made must impact the processing of the original bill for the change to take place.
What to do if Medicare is denied?
If your Medicare claim is denied, you’ll want to file an appeal.
What is a claim number?
A claim number helps Medicare track your claim. This number is most likely your social security number with a letter after it.
How to check Medicare claim status?
You can easily check the status of Medicare claims by visiting MyMedicare.gov; all you need to do is log into your account. Most claims are sent in within 24 hours of processing.
How to file an original Medicare claim?
You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice ...
Who files Medicare claims?
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nursing facility (SNF) or hospice care. When it comes to outpatient care, some providers will not file claims. This can happen if you have Original Medicare and see a non-participating provider, or if you have Medicare Advantage and visit an out-of-network doctor.
What is a Medicare claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hospital. If you have a Medicare Advantage or Part D plan, your insurer will process claims on Medicare’s behalf.
How long do I have to file a claim?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
What should I do if my provider doesn’t file my claim?
Before receiving care, ask your provider’s office whether they will submit your bill to Original Medicare. While they aren’t required to do so, some non-participating providers will still file your claims with Medicare.
What if I’ve already paid for my care?
You may have already paid in full for your care when you filed your claim. Be sure to note that you’ve paid on your submission, so Medicare or your insurer reimburses you rather than your provider. Keep copies of everything you submit.
Do I need to file Part D claims?
If you have to fill medications at a pharmacy outside your plan’s network because of an emergency, you may be able to receive partial reimbursement by submitting your receipt and supporting documentation to your Part D insurer. Contact your insurer for instructions if you need to file an out-of-network claim.
Who fills out the Medicare claims?
Generally, the doctor or other healthcare professional will fill in the forms to make the claim with Medicare for reimbursement. This article looks at the Medicare claims procedure, and why and when a person might need to file a claim. It then details those circumstances, the process, and any time limitations.
How long does it take for Medicare to process a patient request?
After a person submits the form, Medicare may take up to 60 days to process ...
How long does it take to get medicare on a ship?
territorial waters. To meet the criteria, the vessel needs to either be in a U.S. port or have left the U .S. port less than 6 hours previously or will be in the U.S. port within 6 hours.
Can a supplier submit a DME claim?
If a person gets covered durable medical equipment (DME), including prosthetics and orthotics, then the supplier will usually put in the claim for services to Medicare. In some cases, the supplier may not submit the claim, which means the person may have to make a claim for the D ME.
Do foreign hospitals have to file a Medicare claim?
and require care for a medical emergency, but the foreign hospital is closer than the hospital in the U.S. Foreign hospitals do not have to file a Medicare claim, so it may be up to the person to do so.
Does Medicare pay for out of state?
Usually, Medicare does not pay for services when a person is out of the U.S., which includes anywhere other than the 50 states, the District of Columbia, the U.S. Virgin Islands, American Samoa, Guam, the Northern Mariana Islands, and Puerto Rico.
Does Medicare cover diabetic test strips?
Typically, the Medicare-participating provider, such as a person’s doctor, fills in the forms and files the reimbursement request. Medicare does not process claims for Part B drugs or diabetic test strips.
Complaints about the quality of your care
Contact your Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) for complaints about the quality of care you got from a Medicare provider.
note
For questions about a specific service you got, look at your Medicare Summary Notice (MSN) or log into your secure Medicare account . You can file an appeal if you disagree with a coverage or payment decision made by one of these:
How to submit Medicare claims electronically?
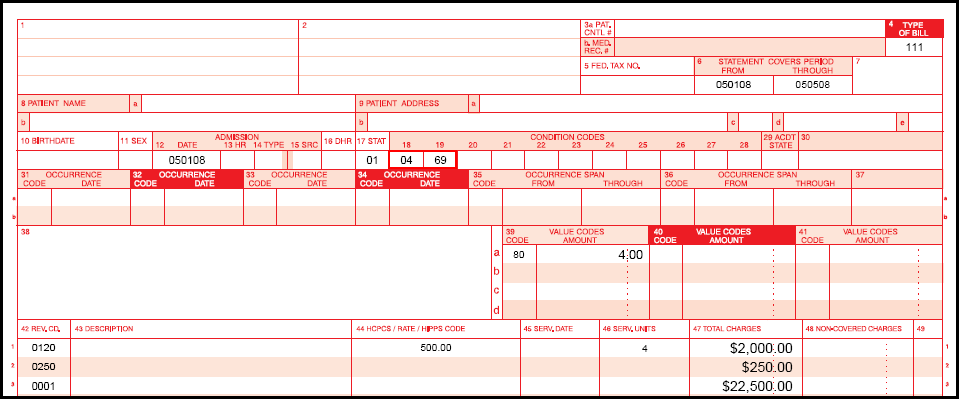
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & certification category area of this web site and the EDI Enrollment page in this section of the web site. Providers that bill institutional claims are also permitted to submit claims electronically via direct data entry (DDE) screens.
What chapter is Medicare claim processing manual?
For more information please contact your local MAC or refer to the Medicare Claims Processing Manual (IOM Pub.100-04), Chapter 24.
What is 10.4 in Medicare?
10.4 - Payment of Nonphysician Services for Inpatients
What is 70.1 in medical billing?
70.1 - Providers Using All-Inclusive Rates for Inpatient Part A Charges
What is CAH 30.1.1?
30.1.1 - Payment for Inpatient Services Furnished by a CAH
What is Medicare 20.1.2.7?
20.1.2.7 - Procedure for Medicare contractors to Perform and Record Outlier Reconciliation Adjustments
What is 90.4.2 billing?
90.4.2 - Billing for Liver Transplant and Acquisition Services
What's the difference between a complaint and an appeal?
A complaint is about the quality of care you got or are getting. For example, you can file a complaint if you have a problem calling the plan, or you're unhappy with how a staff person at the plan treated you.
Need help filing a complaint?
Contact your State Health Insurance Assistance Program (SHIP) for free personalized help.
note
For questions about a specific service you got, look at your Medicare Summary Notice (MSN) or log into your secure Medicare account . You can file an appeal if you disagree with a coverage or payment decision made by one of these:
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Is GHP a disability?
Disability and Employer GHP: Individual is disabled, is covered by a GHP through his or her own current employment (or through a family member’s current employment) AND the employer has 100 or more employees (or at least one employer is a multi-employer group that employs 100 or more individuals) GHP pays Primary, Medicare pays secondary.