What are the five levels for appealing a Medicare claim?
What are the steps taken when appealing a Medicare claim?
- If you have Original Medicare, start by looking at your "Medicare Summary Notice" (MSN). ...
- Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. ...
- Or, send a written request to company that handles claims for Medicare to the address on the MSN.
What should I say in a Medicare appeal?
- your name and address.
- your Medicare number (as shown on your Medicare card)
- the items you want Medicare to pay for and the date you received the service or item.
- the name of your representative if someone is helping you manage your claim.
How do I write a Medicare appeal letter?
How successful are Medicare appeals?
Can providers appeal denied Medicare claims?
How do I correct a Medicare billing error?
What is a Medicare reconsideration?
What is the first level of the Medicare appeals process?
How do I appeal a Medicare Part B premium?
How do I write an appeal letter?
- Review the appeal process if possible.
- Determine the mailing address of the recipient.
- Explain what occurred.
- Describe why it's unfair/unjust.
- Outline your desired outcome.
- If you haven't heard back in one week, follow-up.
- Appeal letter format.
How do I write a letter of appeal for a denied claim?
- Patient name, policy number, and policy holder name.
- Accurate contact information for patient and policy holder.
- Date of denial letter, specifics on what was denied, and cited reason for denial.
- Doctor or medical provider's name and contact information.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
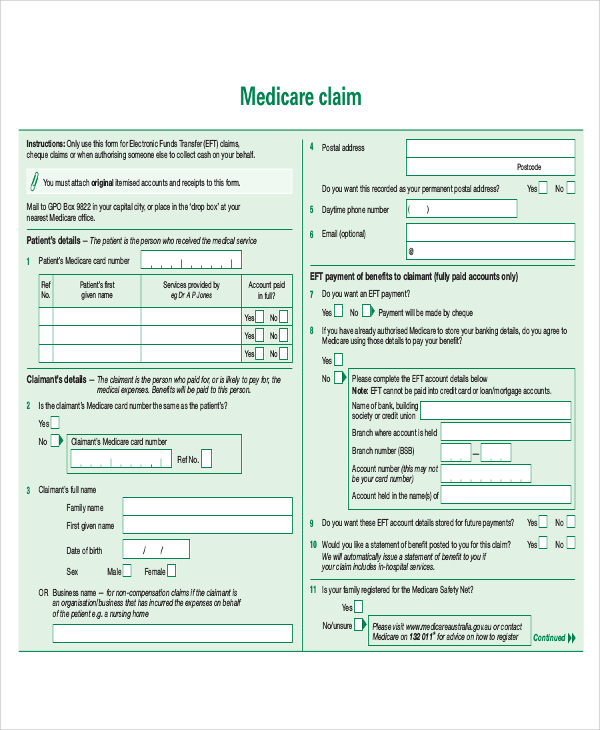
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
How long does it take to appeal a denied Medicare claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim.
What happens if you disagree with a Medicare decision?
If you disagree with a decision about one of your Medicare claims, you have the right to challenge that decision and file an appeal. Situations in which you can appeal include: Denials for health care services, supplies or prescriptions that you have already received. For example: During a medical visit your doctor conducts a test.
How to report Medicare not paying?
If you still have questions about a claim you think Medicare should not have paid, report your concerns to the Medicare at 1-800-MEDICARE. Make copies for your records of everything you are submitting. Send the MSN and any additional information to the address listed at the bottom on the last page of your MSN.
What to do if Medicare decision is not in your favor?
If that decision is not in your favor, you can proceed up the appeals levels to an administrative law judge, the Medicare Appeals Council and federal court.
What is the second level of Medicare appeal?
If your concerns aren’t resolved to your satisfaction at this level, you can file an appeal form with Medicare to advance your request to the second “reconsideration” level in which an independent review organization, referred to as the “qualified independent contractor,” assesses your appeal.
Why does Medicare reject my doctor's recommendation?
For example: Your Medicare Part D drug plan rejects your doctor’s recommendation that you receive a discount on an expensive medication because the available lower-cost drugs are not effective for your condition.
How to appeal a Medicare benefit?
Write down the specific service or benefit you are appealing and the reason you believe the benefit or service should be approved, either on the notice or on a separate piece of paper. Use the “Redetermination Request Form” available at cms.gov, or call 800-MEDICARE (800-633-4227) to have a form sent to you..
How many levels of appeals are there for Medicare?
The process of filing a Medicare appeal depends on what type of plan you have. But the appeal process generally has five levels. So, if your original appeal is denied, you will likely have additional opportunities to make your case.
What to do if Medicare denies your request?
If the drug plan denies your request, you or your designated representative can file a formal appeal by phone or mail.
How to file a grievance with Medicare?
If your Medicare Prescription drug plan doesn't respond to your request, you can file a grievance by calling 800-MEDICARE (800-633-4227) . Continued. If you need help filing an appeal, get in touch with your state's State Health Insurance Assistance Program (SHIP). Your local SHIP can help you whether your appeal is for Original Medicare, ...
What to do if your insurance denies your appeal?
If the insurer denies your appeal, you may request a review by an independent group affiliated with Medicare. Your plan is required to provide you information on how to file an independent review of the plan’s denial. If you think that your Medicare Advantage program's refusal is jeopardizing your health, ask for a "fast decision.".
How often do you get a Medicare summary notice?
Whenever Medicare approves (or denies) payment, called an “initial determination,” you'll get a record of it on the "Medicare Summary Notice" you receive every three months in the mail. To file a Medicare appeal or a “redetermination,” here's what you do:
What is Medicare Advantage?
With Medicare Advantage plans, you're dealing not only with Medicare, but with the rules set by the private insurance company that runs your program. So, you start by working through your insurer, which should have provided you instructions on how to file an appeal.
How to appeal a Medicare claim?
The appeals process starts with your Medicare Summary Notice or MSN–the document you get in the mail every three months. MSN explains the status of your recent healthcare claims. If Medicare denies a claim, you can file an appeal. You can file an appeal by submitting a Redetermination Request form to the company on the last page of your MSN. You can also write a letter to appeal Medicare’s decision.
What happens if you appeal a Medicare claim?
If your appeal is approved, Medicare or your plan will pay the Medicare-allowed amount of the claim. You don’t need to do anything further.
How to check on Medicare appeal?
Call Medicare to check on the status of your appeal and have your reconsideration number ready .
How long does it take for Medicare to redetermine?
You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN.
What happens if Medicare denies coverage?
If Medicare denies coverage for a healthcare service, item, or medication, you have a right to appeal. You can also appeal if a hospital or skilled nursing facility discharge you before you are ready. You have this right whether your claim relates to Part A, Part B, a prescription plan, or Medicare Advantage.
What is the level 3 appeal hearing?
Appeal Hearing before the Office of Medicare Hearings. At this level, an administrative law judge hears your claim. At the hearing, you can present facts and testimony. After reviewing all the information, the judge will make a new decision on your request. Your claim must be for at least a specific dollar amount ($170 in 2021) to be eligible for a Level 3 appeal.
How many levels of appeals are there for Medicare?
The full Medicare appeals process has five levels. At the end of each step, you’ll receive a notice explaining the procedure for appealing to the next level.
How to contact Medicare by phone?
If you have questions about appointing a representative, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048.
What is a Medicare representative?
Your name, address, phone number, and Medicare Number. A statement appointing someone as your representative. The name, address, and phone number of your representative. The professional status of your representative (like a doctor) or their relationship to you. A statement authorizing the release of your personal and identifiable health ...
What is MAC in Medicare?
Send the representative form or written request with your appeal to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare ), or your Medicare health plan. If you have questions about appointing ...
Who can be your representative?
Your representative can be a family member, friend, advocate, attorney, doctor or someone else who will act on your behalf.
Do you keep a copy of everything you send to Medicare?
Keep a copy of everything you send to Medicare as part of your appeal.
How long does it take to appeal Medicare?
2How do I appeal if I have Original Medicare? You can submit additional information or evidence to the MAC after filing the redetermination request, but it may take longer than 60 days for the MAC to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days to make a decision for each submission.
How to appoint a representative for an appeal?
Your representative can be a family member, friend, advocate, attorney, doctor, or someone else to act on your behalf. You can appoint your representative in one of these ways: ■ Fill out an “Appointment of Representative” form (CMS Form number 1696). To get a copy, visit CMS.gov/cmsforms/downloads/cms1696.pdf, or call 1-800-MEDICARE and ask for a copy. Words in red are defined on pages 55–58.
How to file for reconsideration of Medicare?
The address is listed in the QIC’s reconsideration notice. You or your representative can file a request for a hearing in one of these ways: 1. Fill out a “Request for Administrative Law Judge (ALJ) Hearing or Review of Dismissal” form (OMHA-100), which is included with the “Medicare Reconsideration Notice.” You can also get a copy by visiting hhs.gov/about/agencies/omha/filing- an-appeal/forms/index.html, or calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. 2. Submit a written request that must include: • Your name, address, phone number, and Medicare Number. If you’ve appointed a representative, include the name, address, and phone number of your representative. • The appeal number included on the “Medicare Reconsideration Notice,” if any. • The dates of service for the items or services you’re appealing. See your MSN or “Medicare Reconsideration Notice” for this information. • An explanation of why you disagree with the reconsideration decision being appealed. • Any information that may help your case. If you can’t include this information with your request, include a statement explaining what you plan to submit and when you’ll submit it. Words in red are defined on pages 55–58.
How to appeal a QIC decision?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator. A hearing before an ALJ allows you to present your appeal to a new person who will independently review your appeal and listen to your testimony before making a new and impartial decision. An ALJ hearing is usually held by phone or video-teleconference, but can be held in person if the ALJ finds that you have a good reason. You can ask OMHA to make a decision without holding a hearing (based only on the information that’s in your appeal record). If you do this, either an ALJ or an attorney adjudicator will review the information in your appeal record and issue a decision. The ALJ or attorney adjudicator may also issue a decision without holding a hearing if, for example, information in your appeal record supports a decision that’s fully in your favor. To get a hearing or review by OMHA, the amount of your case must meet a minimum dollar amount. For 2020, the required amount is $170. The required amount for 2021 is $180. The “Medicare Reconsideration Notice” may include a statement that tells you if your case is estimated to meet the minimum dollar amount. However, it’s up to the ALJ to make the final decision. You may be able to combine claims to meet the minimum dollar amount.
How to request a Medicare reconsideration?
The QIC’s address is listed on the “Medicare Redetermination Notice.” You can request a reconsideration in one of these ways: 1. Fill out a “Medicare Reconsideration Request” form (CMS Form number 20033), which is included with the “Medicare Redetermination Notice.” You can also get a copy by visiting CMS.gov/cmsforms/downloads/cms20033.pdf, or calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
What is level 1 Medicare?
Level 1: Redetermination by the Medicare Administrative Contractor (MAC)
How many levels of appeals are there?
The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council) Level 5: Judicial Review by a Federal District Court If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get a decision letter with instructions on how to move to the next level of appeal.
How to appeal a health insurance claim?
Here are 4 tips to help you get started: 1 Get help: If you want help filing an appeal, contact your State Health Insurance Assistance Program (SHIP) or appoint a representative. Your representative could be a family member, friend, advocate, attorney, doctor, or someone else who will act on your behalf. 2 Gather information: Ask your doctor, other health care providers, or supplier for any information that may help your case. 3 Keep copies: Be sure to keep a copy of everything you send to your plan as part of your appeal. 4 Start the process: Follow the directions in your plan’s initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. See what information to include in your written request.
How long do you have to file a denial of health insurance?
Start the process: Follow the directions in your plan’s initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. See what information to include in your written request.
Does Medicare Advantage cover diabetics?
If you have a Medicare Advantage Plan, you know it covers a lot of items and services, like prescription drugs, diabetic test supplies, cardiovascular screenings, and hospital visits. But, what should you do if your plan won’t cost an item or service you need?
Can you ask Medicare Advantage to pay for services?
You have the right to ask your Medicare Advantage Plan to provide or pay for items or services you think should be covered, provided, or continued. To resolve these differences with your plan, learn how to file an appeal.
Can you disagree with a Medicare decision?
Once you start the appeals process, you can disagree with the decision made at any level of the process and can generally go to next level. Learn more about appeals in a Medicare Advantage Plan.
