How do I file a Medicare appeal?
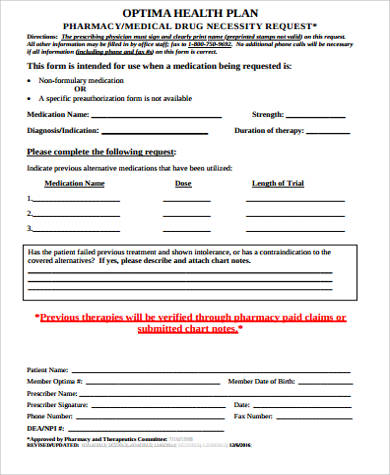
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
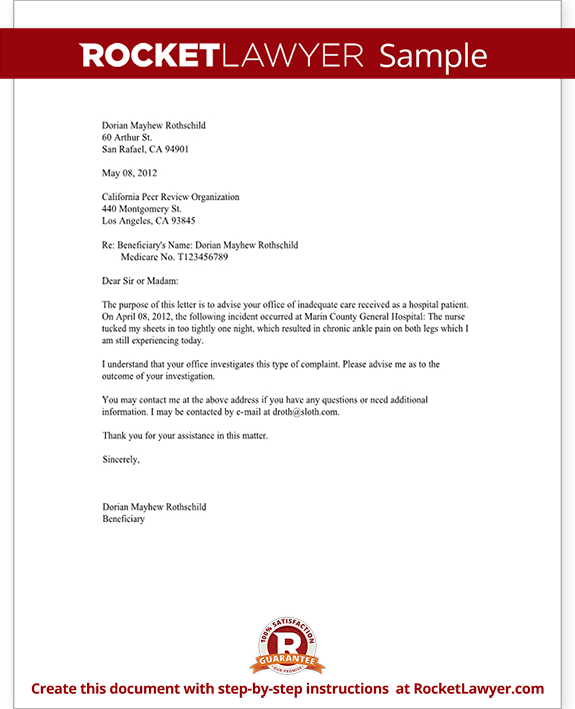
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Who pays if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
What is the first level of appeal in the Medicare program?
redeterminationAppeal the claims decision. The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
What are Medicare appeals?
If you disagree with a Medicare coverage or payment decision, you can appeal the decision. This is called a redetermination. Medicare contracts with the MACs to review your appeal request and make a decision.
How long does Maximus take to review an appeal?
Workers Compensation Appeals With the introduction of IMR, disputes are resolved in 2 weeks on average - down from nearly 12 months under the cumbersome court system it replaced.
How do you write a successful appeal letter?
Follow these steps to write an effective appeal letter.Step 1: Use a Professional Tone. ... Step 2: Explain the Situation or Event. ... Step 3: Demonstrate Why It's Wrong or Unjust. ... Step 4: Request a Specific Action. ... Step 5: Proofread the Letter Carefully. ... Step 6: Get a Second Opinion.
How do you write an appeal statement?
Content and ToneOpening Statement. The first sentence or two should state the purpose of the letter clearly. ... Be Factual. Include factual detail but avoid dramatizing the situation. ... Be Specific. ... Documentation. ... Stick to the Point. ... Do Not Try to Manipulate the Reader. ... How to Talk About Feelings. ... Be Brief.More items...
How do I appeal Medicare underpayment?
You can appeal an underpayment by timely submitting a request for a redetermination appeal to your regional contractor (e.g. Palmetto-GBA for California).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
What is a QIC?
QIC is an independent contractor that didn’t take part in the level 1 decision. The QIC will review your request for a reconsideration and will make a decision.
Can you request a fast reconsideration?
If you disagree with the plan’s redetermination, you, your representative, or your doctor or other prescriber can request a standard or expedited (fast) reconsideration by an IRE. You can’t request a fast reconsideration if it’s an appeal about payment for a drug you already got.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
What is a denial of a request?
Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition. Denials of a request you and your doctor have made to change the price you pay for a prescription drug. For example: Your Medicare Part D drug plan rejects ...
How to request a plan exception?
Requests for plan exceptions can be made by phone or in writing if you are asking for a prescription drug you haven’t yet received. If you are asking to be reimbursed for the price of drugs you have already bought, you must make your request in writing.
Can you appeal a Part D plan?
If your life or health could be at risk by having to wait for a medication approval from your plan, you or your doctor can request an expedited appeal by phone. If you disagree with your Part D plan’s decision, you can file a formal appeal.
Can you appeal a Medicare Advantage plan?
Medicare Advantage plans, which are administered by private insurance companies, are required by Medicare to have an appeals process by which you can get a redetermination if your plan denies you a service or benefit you think should be covered. If you disagree with the decision, you can request an independent review.
How long does Medicare cover SNF?
It will cover up to 100 days in a SNF, with the goal being that the beneficiary can then resume normal self-care. Medicare Advantage plans follow these same rules. It appeared Joe was refusing to try to get well, so the carrier actually did have grounds to deny the claim.
What happened to the man who fell on his back?
The fall had caused him to break his arm and bruise his back. Upon admittance to the hospital, he was diagnosed with low blood pressure, low oxygen and a severe and debilitating UTI. This infection, coupled with the pain medication he was given, had left him feeling weak, foggy and confused.
Does Medicare pay for skilled nursing facilities?
The Medicare Advantage carrier then denied payment for the Skilled Nursing Facility (SNF). Their denial stated that Joe had “refused to participate” in therapy that would begin his rehabilitation. Medicare generally does not provide skilled nursing facility care for beneficiaries who are not expected to recover.
Can Medicare be denied?
You’ve helped someone through something that potentially could have been costly for them. Medicare bills sometimes get denied, especially when you are on a Medicare Advantage plan. Read on to see how we handed this particular denial.
What happens if your appeal is denied?
If your appeal is denied, you can make additional appeals. While your first appeal is decided by the same organization that processed the original claim, other appeals are heard by third parties involved in the initial decision. There are five levels of appeals.
How many claims does Medicare process?
Medicare processes more than a billion claims every year, and there will inevitably be mistakes and oversights. Knowing your Medicare rights and protections can help you navigate the health program more easily.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
What is a Medicare representative?
Your name, address, phone number, and Medicare Number. A statement appointing someone as your representative. The name, address, and phone number of your representative. The professional status of your representative (like a doctor) or their relationship to you. A statement authorizing the release of your personal and identifiable health ...
What is MAC in Medicare?
Send the representative form or written request with your appeal to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare ), or your Medicare health plan. If you have questions about appointing ...
What's New
December 2019: The Parts C and D Enrollee Grievance, Organization/Coverage Determinations and Appeals Guidance has been updated to include recent regulatory changes and will be effective January 1, 2020. Questions related to the guidance or appeals policy may be submitted to the Division of Appeals Policy at https://appeals.lmi.org.
Overview
Medicare health plans, which include Medicare Advantage (MA) plans (such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans) Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance, organization determination, and appeals processing under the MA regulations found at 42 CFR Part 422, Subpart M.
Web Based Training Course Available for Part C
The course covers requirements for Part C organization determinations, appeals, and grievances. Complete details can be accessed on the "Training" page, using the link on the left navigation menu on this page.
How to request reconsideration of Social Security?
A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772.1213) as well as by writing to SSA .
What are the life changing events?
There are 7 qualifying life-changing events: 1 Death of spouse 2 Marriage 3 Divorce or annulment 4 Work reduction 5 Work stoppage 6 Loss of income from income producing property 7 Loss or reduction of certain kinds of pension income
What is a work stoppage?
Work stoppage. Loss of income from income producing property. Loss or reduction of certain kinds of pension income. Events that result in the loss of dividend income or affect a beneficiary's expenses, but do not affect the beneficiary's modified adjusted gross income are not considered qualifying life-changing events.