Insurance claims can be submitted through a medical claims management system or a direct data entry system. Minnesota State Statute, section 62J.536, requires all health care providers to submit claims, including secondary claims, electronically using a standard format.
Full Answer
Where can I find more information about Medicare in Minnesota?
If you need more information, the Minnesota Board on Aging's annual Minnesota-focused Medicare guide, Health Care Choices for Minnesotans on Medicare can help.
How do I file a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I get Medicare to give my personal health information?
You need to fill out an " Authorization to Disclose Personal Health Information " if you want someone to be able to call 1-800-MEDICARE on your behalf or you want Medicare to give your personal information to someone other than you. Get this form in Spanish. Find out who to call about Medicare options, claims and more.
When do I need to file a Medicare claim?
When do I need to file a claim? Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How do I submit a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I submit Medicare Part B?
Contact Social Security to sign up for Part B:Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). ... Call 1-800-772-1213. ... Contact your local Social Security office.If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
What documentation is required for Medicare?
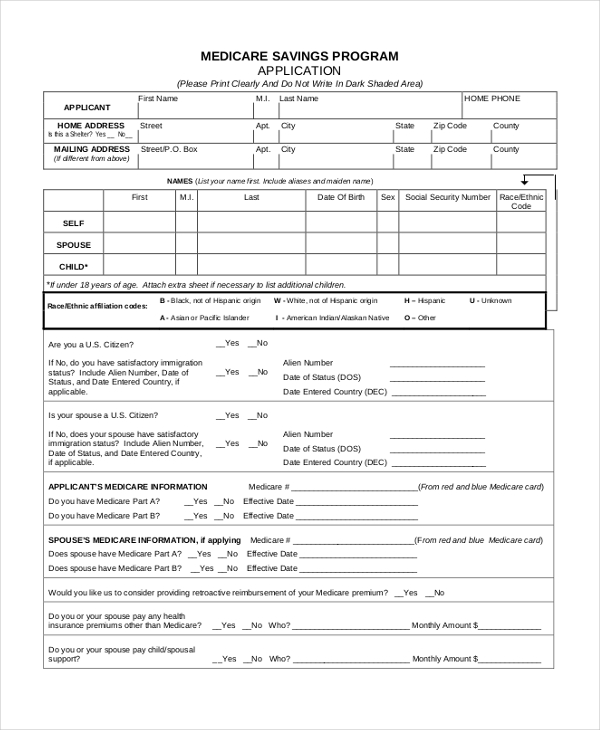
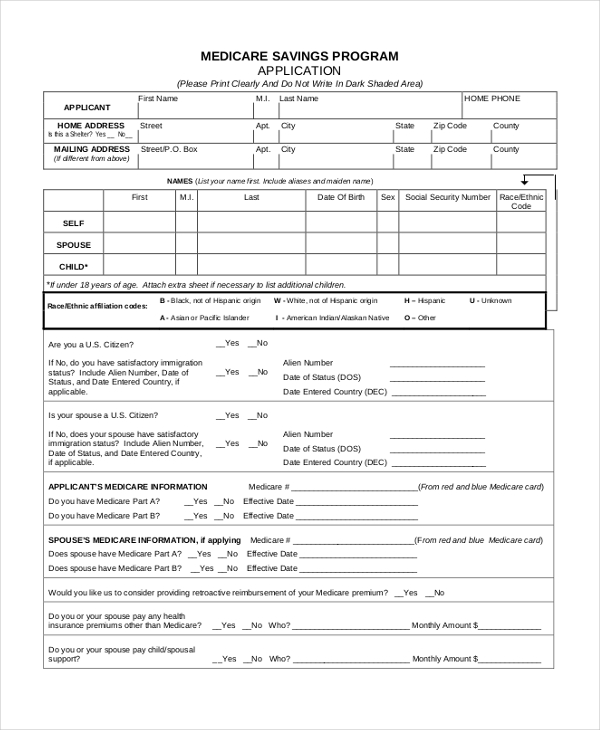
Applying for Medicare: What Documents Do I Need? You'll need to prove that you're eligible to enroll in Medicare. You might need to submit documents that verify your age, citizenship, military service, and work history. Social Security can help you get copies of any documents you no longer have.
What are the 3 requirements for Medicare?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
How long does it take for Medicare Part B to be approved?
Yes. You automatically get Part A and Part B after you get disability benefits from Social Security or certain disability benefits from the RRB for 24 months. If you're automatically enrolled, you'll get your Medicare card in the mail 3 months before your 65th birthday or your 25th month of disability.
How do I file medical necessity?
Documentation of medical necessity should do the following:Identify a specific medical reason or focus for the visit (e.g., worsening or new symptoms)Document the rationale for ordering tests or referrals.More items...•
When should you apply for Medicare?
Generally, we advise people to file for Medicare benefits 3 months before age 65. Remember, Medicare benefits can begin no earlier than age 65.
How should documentation of time be entered into the medical record in 2021?
2021 Time CalculationThe total time of time spent should include face-to-face and non-face-to-face time working for that specific patient.Only includes the time spent by the physician or QHP, not the clinical staff.All time must be on the date of service, NOT the day before or the day after.More items...•
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
How much does Medicare cost at age 62?
Reaching age 62 can affect your spouse's Medicare premiums He can still receive Medicare Part A, but he will have to pay a monthly premium for it. In 2020, the Medicare Part A premium can be as high as $458 per month.
What is Medicare insurance?
Medicare. Medicare is a national health insurance program in the United States, begun in 1966 under the Social Security Administration and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans age 65 and older, persons with disability status as determined by ...
Who regulates Medicare Supplement and Medicare Supplement?
The Minnesota Department of Commerce and the federal government both regulate Medicare Cost and Medicare Supplement and Select insurance plans. The federal government is responsible for the oversight of Medicare Advantage and Part D plans.
How long does it take to enroll in Medicare?
There is a seven-month period when you can first enroll in Medicare. It’s called the Initial Enrollment Period (IEP) and it happens three months before the month you turn age 65, the month of your 65th birthday and the three months after.
When will Medicare premiums be deducted?
Paying Medicare Premiums. If you get Social Security benefits, your Medicare Part B premium will automatically be deducted from your check, beginning one month before Medicare starts. If you do not get a Social Security check, you will receive a premium bill. There are four ways to pay:
How long does it take to get Social Security Disability?
If you are disabled and under age 65, there is a seven-month period surrounding the 25th month you begin receiving Social Security Disability payments. Enrollment time frames are different for people who become eligible because of end-stage renal disease or Lou Gehrig’s Disease (ALS).
How old do you have to be to get medical assistance in Minnesota?
Applying for Medical Assistance (MA) and MinnesotaCare. This information is for families with children as well as adults who do not have children under age 19 living with them, are under age 65 and do not have a disability. If you are only applying for coverage for a person who is 65 or older, please see the page on how to apply if you are a senior.
How to contact a navigator in Minnesota?
By calling 855-366-7873. Contacting a navigator in your area. Go to the MNsure website or call 855-366-7873 for a list of navigators. At your county or tribal office or the MinnesotaCare office. Learn more about how county workers or MNsure navigators can help.
Does the date you submit your insurance application affect your coverage?
Yes, the date you submit your application online or we get your paper application affects when your coverage can start. Coverage may start: The first day of the month you submit your application online or we get your paper application.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you didn't get your prescription yet?
If you didn't get the prescription yet, you or your prescriber can ask for an expedited (fast) request. Your request will be expedited if your plan determines, or your prescriber tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
How long do you have to return Minnesota health insurance renewal?
You have 45 days from the date printed on your renewal to return your form. You could lose your health care coverage for one or more months if you return your form after the 45 days. Be sure to follow the instructions on the notice. Renewing MinnesotaCare eligibility for January 2020.
How often do you have to renew your medical insurance in Minnesota?
If you have Medical Assistance (MA) or MinnesotaCare coverage, the Department of Human Services (DHS) must redetermine your eligibility once a year to see whether you are still eligible for health care coverage. This process is called a renewal.
When will MinnesotaCare renew?
Renewing MinnesotaCare eligibility for January 2020. All MinnesotaCare members must verify that they remain eligible for MinnesotaCare by the end of the year. You will receive a notice from DHS explaining what you need to do to renew your eligibility. You do not need to do anything until you get this notice.
How long does it take for Medicare to process a claim?
A claim that with charge and adjustments out of balance will suspend for review and are considered complex claims that may take up to 90 days to process. Submit claims for services that are never covered by Medicare directly to MHCP. You do not need a denial from Medicare.
How long after TPL claim to bill MHCP?
Do not bill MHCP earlier than 90 days after the initial attempt.
What is MHCP payment?
MHCP payment is the difference between the Medicare payment and the MHCP calculated allowable where the difference is greater than zero. If the difference is less than or equal to zero, the MHCP payment will be zero.
How long does MHCP suspend a claim?
If you do not report all adjustment codes and amounts on the claim or line level to balance the claim or line, MHCP may suspend the claim for up to 90 days or deny the claim or line. MHCP uses HIPAA-compliant claims adjustment reason code 129 and remittance advice reason code M04.
What is Medicare and other insurance?
Medicare is administered by the Centers for Medicare & Medicaid Services (CMS) and is the federal health insurance program for people 65 years old and older and certain people with disabilities. Other insurance, or third party liability (TPL), refers to health, ...
What happens if a member requests a billing statement?
If a member requests a billing statement, the statement must clearly state that it is not a bill and payment has been made or could be made by MHCP. Providers must report the request in writing to the Benefit Recovery Section.
Is Medicare a primary payer for MHCP?
Medicare. Medicare is primary to MHCP. Services covered by Medicare must be provided by a Medicare-enrolled provider and billed to Medicare first. Bill any balance after Medicare payment to other TPL payers.
When Do I Need to File A Claim?
How Do I File A Claim?
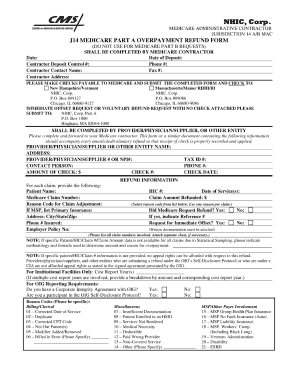
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them an...