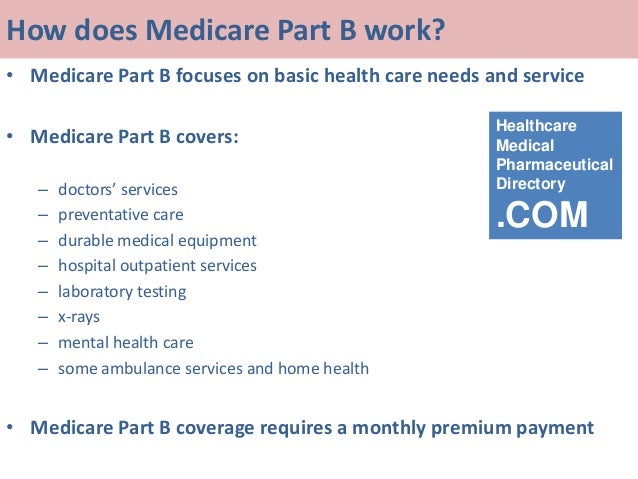
If your physician feels it is medically necessary to perform more often, obtain an advance beneficiary notice (ABN) and submit 92250 with modifier -GA for Medicare Part B. The patient will likely be financially responsible for the test. You can find Medicare Part B policies at aao.org/lcds.
Full Answer
How much does Medicare pay for a CPT 92250?
Jan 26, 2016 · ANSWER: In the Medicare Physician Fee Schedule Database (MPFSDB), fundus photography (CPT code 92250) is designated as a Bilateral Indicator 2 code, which means that payment is already based upon it being performed bilaterally. Therefore, CPT modifier 50 should not be submitted with CPT code 92250. When CPT code 92250 is performed bilaterally, simply …
Is code 92250 a stand-alone service?
General Guidelines for Claims submitted to Part A or Part B MAC: Procedure codes may be subject to National Correct Coding Initiative (NCCI) edits or OPPS packaging edits. ... CPT codes 92250 and 92228 describe services that are performed bilaterally. ... (See CMS Publication 100-04, Medicare Claims Processing Manual, Chapter 25, Section 75 for ...
Can I use CPT code 92250 for fundus photography?
Medicare claim address, phone numbers, payor id – revised list; Medicare Fee for Office Visit CPT Codes – CPT Code 99213, 99214, 99203; ... Fundus photography (CPT code 92250) and scanning ophthalmic computerized diagnostic imaging (CPT code 92133 or 92134) are generally mutually exclusive of one another in that a provider would use one ...
What is ophthalmologic code 92250?
Jun 12, 2020 · 92250 is subject to Medicare's Multiple Procedure Payment Reduction (MPPR). According to Medicare's National Correct Coding Initiative (NCCI), 92250 is bundled with ICG (92240) and mutually exclusive with scanning computerized ophthalmic diagnostic imaging of the posterior segment (92133 or 92134). Click to see full answer.
Does Medicare cover CPT code 92250?
A Yes. According to Medicare's National Correct Coding Initiative (NCCI), 92250 is bundled with ICG (92240) and mutually exclusive with scanning computerized ophthalmic diagnostic imaging of the posterior segment (92133 or 92134).
Does CPT 92250 require a modifier?
2. CPT codes 92250 and 92228 are global services, which include a professional and a technical component. The components should be reported with modifiers 26 or TC as appropriate, if the entire global service is not performed.Jun 1, 2012
Is CPT 92250 a bilateral code?
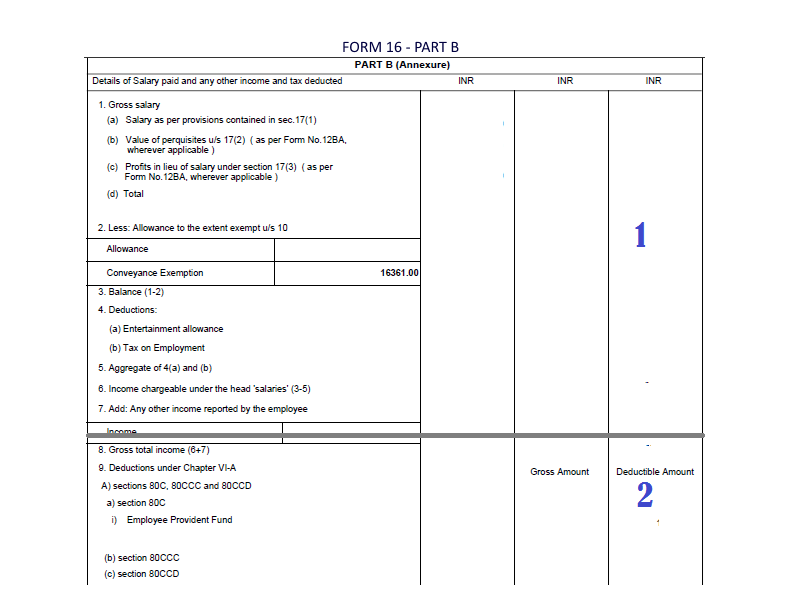
CPT 92250 is defined as bilateral, so reimbursement is for both eyes. The 2020 national Medicare Physician Fee Schedule allowable is $45.83. Of this amount, $23.82 is assigned to the technical component and $22.01 is the value of the professional component (ie, interpretation).Feb 1, 2020
How Much Does Medicare pay for 92250?
Q What is the reimbursement for 92250? A CPT 92250 is defined as bilateral so reimbursement is for both eyes. The 2019 national Medicare Physician Fee Schedule participating allowable is $51.54, including $29.19 for the technical component and $22.34 for the professional component (i.e., interpretation).
What does CPT code 92250 mean?
fundus photographsCode 92250 describes the taking of fundus photographs, that is, photographs of the posterior segment of the inner aspect of the eye, to document alterations in the optic nerve head, retinal vessels, and retinal epithelium. It can be used to document baseline retinal findings and track disease progression.
Can 92250 and 92225 be billed together?
The NCCI edits bundle 92250 with 92134 so 92250 is not billed; 92225 is not bundled with 92250 or 92134 although there are limitations in many coverage policies. The physician's claim will read as shown in Figure 1.Mar 1, 2018
Can 92250 and 92133 be billed together?
Coding Implications Fundus photography with interpretation and report—92250—and either 92133 or 92134 cannot be performed on the same date of service on the same patient.Sep 15, 2017
Is corneal topography covered by Medicare?
Corneal topography will be non-covered if performed pre- or post-operatively in relation to a non-covered procedure, i.e., radial keratotomy. As published in the CMS IOM Publication 100-08, Medicare Program Integrity Manual, Chapter 13, Section 13.5.
Can you bill fundus photo and visual field same day?
The Correct Coding Initiative (CCI) does not have any bundles limiting the use of either CPT codes 92002-92014 or CPT codes 99201-99215 with the fundus photography code, so you can bill both your exam and 92250 on the same day and get paid.May 2, 2018
Does Medicare cover optical coherence tomography?
Q: Does Medicare cover SCODI of the posterior segment with Topcon's 3D OCT-1 Maestro2? A: Yes. Scanning computerized ophthalmic diagnostic imaging of the posterior segment (SCODI-P) is covered by Medicare subject to the limitations in its payment policies; other third party payers generally agree.
Is CPT 92134 covered by Medicare?
Claims for SCODI services (CPT codes 92133 and 92134) are payable under Medicare Part B in the following places of service: The global service is payable in the office (11), nursing facility (32- for Medicare patient not in a Part A stay) and independent clinic (49).
How often can 92134 be billed?
4 times per year92134 is allowed more often – typically up to 4 times per year – or once per month in patients with retinal conditions undergoing active intravitreal drug treatment.Jan 1, 2017
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Language quoted from Centers for Medicare and Medicaid Services (CMS), National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is E08.3521?
E08.3521 Diabetes mellitus due to underlying condition with proliferative diabetic retinopathy with traction retinal detachment involving the macula, right eye. E08.3522 Diabetes mellitus due to underlying condition with proliferative diabetic retinopathy with traction retinal detachment involving the macula, left eye.
Why do we need fundus photography?
Fundus photography may be necessary to establish the extent of retinal edema in moderate non-proliferative diabetic retinopathy. In four to six months, the baseline photograph can be compared to the clinical appearance ...
Why are fundus photographs necessary?
In order to document a disease process , plan its treatment or follow the progress of a disease, fundus photographs may be necessary. Fundus photographs are not medically necessary simply to document the existence of a condition. However, photographs may be medically necessary to establish a baseline to judge later whether a disease is progressive.
Why do contractors specify bill types?
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service . Absence of a Bill Type does not guarantee that the policy does not apply to that Bill Type.
What does "furnished" mean?
Furnished in a setting appropriate to the patient’s medical needs and condition. Ordered and furnished by qualified personnel. One that meets, but does not exceed, the patient’s medical need. At least as beneficial as an existing and available medically appropriate alternative.
What does "appropriate" mean in medical terms?
Appropriate, including the duration and frequency that is considered appropriate for the service, in terms of whether it is: Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member.
Is fundus photography considered medically reasonable?
• Fundus photography is considered medically reasonable and necessary when it is furnished by a qualified optometrist or ophthalmologist in the course of the evaluation and management of a retin al disorder or another condition that has affected the retina as outlined above.
What is fundus photography?
In 2013, a Medicare Part B contractor further confused the situation by stating that fundus photography uses a special camera to photograph structures behind the lens of the eye , including vitreous, retina, choroid and optic nerve.
Is red free color coded separately?
An analogous service provided by a doctor of optometry, obtaining red-free images at the time of color photography, is not coded separately. To summarize, as stated several times over the past few months, ophthalmic technology is evolving more quickly than CPT can keep up.
What is an ABN waiver?
Ask the patient to assume financial responsibility for the charge. A financial waiver can take several forms. An Advance Beneficiary Notice of Noncoverage (ABN) is required for services where Part B Medicare coverage is ambiguous or doubtful, and may be useful where a service is never covered.
What is general supervision in Medicare?
General supervision means the procedure is furnished under the physician’s overall direction and control , but the physician’s presence is not required during the performance of the procedure. Other payers generally agree.
Is Medicare 92250 a multiple procedure?
92250 is subject to Medicare’s Multiple Procedure Payment Reduction (MPPR). This reduces the allowable for the technical component of the lesser-valued test when more than one test is performed on the same day.
Does Medicare cover ophthalmic imaging?
A Ophthalmic imaging is covered by Medicare subject to the limitations in its payment policies ; other third party payers generally agree. Medicare covers fundus photography if the patient presents with a complaint that leads you to perform this test or as an adjunct to management and treatment of a known disease.
Is a diagnostic test reimbursed by Medicare?
In general, this and all diagnostic tests are reimbursed when medically indicated. Clear documentation of the reason for testing is always required. Too-frequent testing can garner unwanted attention from Medicare and other third party payers.

When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…