
How to contact Medicare provider enrollment?
- enrolling, changing your address or opting out of the Medicare FFS program
- where to mail your application
- your National Provider Identifier (NPI) or Provider Transaction Access Number (PTAN)
- revalidation
Where to mail 855r application?
- SPOT
- Find Fee Schedules
- Search LCDs
- Provider Enrollment Enrollment Gateway Check Application Status Confirm a Revalidation Request Determine Your Application Type
- NCCI lookup
- Evaluation & Management E/M Interactive Worksheet Incident-to Tool
- Claims ADR Timeliness Calculator
What is CMS 855r?
Form CMS-855R is used by providers to reassign their right to bill the Medicare program and receive Medicare Part B payments to an eligible individual, clinic/group practice, or other health care organization. The individual or group to whom the benefits are reassigned then submits claims and receives payment on the provider’s behalf.
How to enroll in Medicare as a provider?
Use this guide if any of the following apply:
- You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify.
- You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
- You wish to provide services to beneficiaries but do not want to bill Medicare for your services. ...
What is CMS 855R?
Can a CMS 855R be used for employment?
About this website
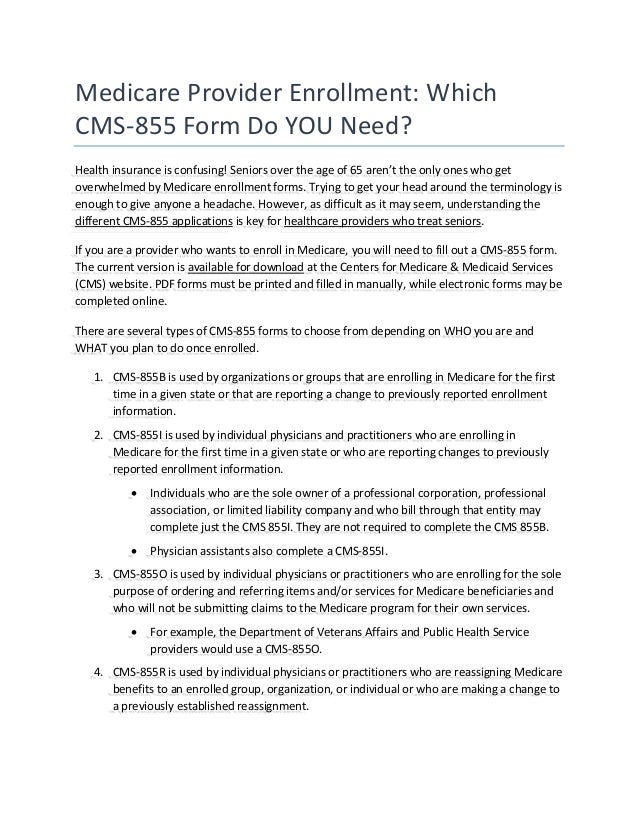
What is Medicare Form 855R?
Complete this application if you are reassigning your right to bill the Medicare program and receive Medicare payments for some or all of the services you render to Medicare beneficiaries, or are terminating a currently established reassignment of benefits.
What is Medicare third party reassignment?
A reassignment of benefits is a mechanism by which Medicare practitioners allow third parties to bill and receive payment for services that they rendered. Practitioners submit to Medicare contractors Form CMS-855I (855I) to enroll in Medicare and Form CMS-855R (855R) to reassign benefits.
How do I reassign my Medicare provider?
Providers and suppliers are able to submit their reassignment certifications either by signing section 6A and 6B of the paper CMS-855R application or, if completing the reassignment via Internet-based PECOS, by submitting signatures electronically or via downloaded paper certification statements (downloaded from www. ...
What forms are needed for Medicare revalidation?
How do I revalidate my Medicare file? You will need to submit a complete CMS-20134, CMS-855A, CMS-855B, or CMS-855I application, depending on your provider / supplier type. If you enrolled in more than one state in our jurisdiction, you are required to submit a separate application for each state.
Can Medicare patients choose to be self pay?
The Social Security Act states that participating providers must bill Medicare for covered services. The only time a participating-provider can accept "self-payments" is for a non-covered service. For Non-participating providers, the patient can pay and be charged up to 115% of the Medicare Fee Schedule.
What does accept assignment mean on CMS 1500?
If the provider accepts assignment, the Medicare payment will be made directly to the provider. Under this method, the provider agrees to accept the Medicare approved amount as full payment for covered services.
How do I fill out a CMS 855i form?
5:1213:56How to Complete the CMS 855I Form to Enroll Individual Reassigning All ...YouTubeStart of suggested clipEnd of suggested clipAnd social security number must match their social security record if you go by another name like aMoreAnd social security number must match their social security record if you go by another name like a professional name that does not match your legal name indicate that in the appropriate. Field.
Is Ptan the same as Medicare ID?
The Provider Transaction Access Number (PTAN) is your unique Medicare identification number. This number is assigned to providers once their enrollment has been approved.
How do I add a reassignment in Pecos?
0:367:08PECOS Reassignment through Individual Providers EnrollmentYouTubeStart of suggested clipEnd of suggested clipState select view manage reassignments on the reassignment. Report screen click manage reassignmentsMoreState select view manage reassignments on the reassignment. Report screen click manage reassignments. Select add a new reassignment.
How often is Medicare revalidation required?
every 5 yearsAll providers and suppliers are required to revalidate their enrollment information every 5 years and every 3 years for DMEPOS suppliers. CMS also reserves the right to request off-cycle revalidations.
What is Medicare recertification?
The recertification statement must contain an adequate written record of the reasons for the continued need for extended care services, the estimated period of time required for the patient to remain in the facility, and any plans, where appropriate, for home care.
What is the revalidation process?
Revalidation is an evaluation of your fitness to practise. This process: supports doctors in regularly reflecting on how they can develop or improve their practice. gives patients confidence doctors are up to date with their practice. promotes improved quality of care by driving improvements in clinical governance.
REASSIGNMENT OF MEDICARE BENEFITS HTTPS://PECOS.CMS.HHS
ADDITIONAL INFORMATION. When establishing a new reassignment, Section 6A must be signed by the individual practitioner . and. Section 6B must be signed by a delegated or authorized official of the organization/group.
PECOS 101 - CMS
PECOS 101 MARCH 2019 Sandhya Mathur, CMS Business Systems Lead, Division of Enrollment Systems. Anthony Peterson, Noridian. Supervisor Operations, Part B Provider Enrollment
Medicare enrollment instructions: Individual reassigning benefits
Where to mail paper enrollment forms and supporting documentation. Paper enrollment forms and supporting documentation, supporting documentation for PECOS web submitted applications, and other enrollment forms (e.g., CMS-460) must be sent through the U.S. mail to the addresses below. Note: For PECOS w eb applications, the CMS-588 must be e-signed or uploaded as a supporting document.
Help - Frequently Asked Questions (FAQs)
centers for medicare & medicaid services 7500 security boulevard baltimore, md 21244
Welcome to the Medicare Provider Enrollment, Chain, and Ownership ...
CMS.gov/Providers - Section of the CMS.gov website that is designed to provide Medicare enrollment information for providers, physicians, non-physician practitioners, and other suppliers.; Revalidation Notice Sent List - Check to see if you have been sent a notice to revalidate your information on file with Medicare.; Enrollment Checklists - Review checklists of information needed to complete ...
Provider Transaction Access Number (PTAN) - JE Part B
A PTAN is a Medicare-only number issued to providers by Medicare Administrative Contractors (MACs) upon enrollment to Medicare. MACs issue an approval/notification letter, including PTAN information, when an enrollment is approved.
Section 2
Did you provide the requested information for the supplier to whom benefits are being reassigned, or reassignment is being terminated?
Section 4
Did you indicate the Primary Practice Location that the individual practitioner will render services most of the time?
Section 5
Did you complete section 5 (on page 3), with the contact person information?
Your application contact information
The following chart describes when and how First Coast Service Options will contact providers based on the contact information provided in your enrollment application.
What is CMS 855R?
The CMS-855R application is used by individual physicians and non-physician practitioners (hereafter collectively referred to as “individual practitioners”) who want to reassign their right to receive Medicare payments to another eligible individual or entity (i.e., sole proprietorship/clinic/group practice/other health care organization); Medicare eligible professionals may also reassign their benefits to a critical access hospital (CAH) that bills Method II in order to participate in the Electronic Health Records (EHR) Incentive Program for Eligible Professionals (EPs). In addition, the CMS-855R is used to terminate a currently established reassignment of benefits.
Can a CMS 855R be used for employment?
The CMS-855R shall not be used to report employment arrangements of physician assistants. Employment arrangements for physician assistants must be reported on the CMS-855I application. In addition, a CMS-855R application is not required to be submitted with a CMS-855B for an independent diagnostic testing facility (IDTF) that employs or contracts with interpreting physicians.
What is CMS 855R?
CMS-855R is to be used for Reassignment of Medicare Benefits -- Complete this application if you are reassigning your right to bill the Medicare program and receive Medicare payments, or are terminating a reassignment of benefits.
Who uses CMS 855O?
CMS-855O is to be used by Eligible Ordering and Referring Physicians and Non-physician Practitioners -- CMS requires certain physicians and non-physician practitioners to register in the Medicare program for the sole purpose of ordering or referring items or services for Medicare beneficiaries.
What is enrollment application assistance tool?
The enrollment application assistance tool removes the guesswork for providers trying to figure out which enrollment form to use, whether they are submitting an initial enrollment, a change of information, revalidation or even terminating their Medicare enrollment.
Who completes CMS 460?
The CMS-460 may only be completed by new physicians, practitioners, and suppliers looking to become participating providers during initial enrollment and during annual participation open enrollment. Learn more about the purpose of the Medicare Participating Physician or Supplier Agreement (CMS-460).
What is CMS 855R?
The CMS-855R application is used by individual physicians and non-physician practitioners (hereafter collectively referred to as “individual practitioners”) who want to reassign their right to receive Medicare payments to another eligible individual or entity (i.e., sole proprietorship/clinic/group practice/other health care organization); Medicare eligible professionals may also reassign their benefits to a critical access hospital (CAH) that bills Method II in order to participate in the Electronic Health Records (EHR) Incentive Program for Eligible Professionals (EPs). In addition, the CMS-855R is used to terminate a currently established reassignment of benefits.
Can a CMS 855R be used for employment?
The CMS-855R shall not be used to report employment arrangements of physician assistants. Employment arrangements for physician assistants must be reported on the CMS-855I application. In addition, a CMS-855R application is not required to be submitted with a CMS-855B for an independent diagnostic testing facility (IDTF) that employs or contracts with interpreting physicians.
