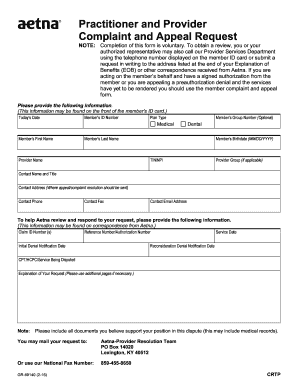
The following tips can help you fill in Medicare Reconsideration Form easily and quickly:
- Open the template in our feature-rich online editor by clicking Get form.
- Complete the requested fields that are yellow-colored.
- Press the arrow with the inscription Next to jump from field to field.
- Go to the e-autograph solution to e-sign the form.
- Add the relevant date.
Full Answer
How to do Medicare redetermination request?
- Circle the item (s) and/or services you disagree with on the MSN.
- Explain in writing why you disagree with the decision or write it on a separate piece of paper, along with your Medicare number, and attach it to the MSN.
- Include your name, phone number, and Medicare Number on the MSN.
How to file a request for reconsideration?
- Modifies the findings of fact and decision;
- Sets aside the findings of fact and decision and directs that an additional evidentiary hearing be conducted, or;
- Affirms the findings of fact and decision.
How to file for reimbursement from Medicare?
When filling out the form, you must choose the service type then provide the following information:
- Itemized Bill
- The provider or supplier’s National Provider Identifier (NPI) If known
- Description of Illness or Injury
- Date of Service
- Place of Service
- The doctor’s or supplier’s name and address
- Description of each surgical or medical service or supply furnished
- Charge for each service
How to appeal a Medicare decision?
To increase your chance of success, you may want to try the following tips:
- Read denial letters carefully. ...
- Ask your healthcare providers for help preparing your appeal. ...
- If you need help, consider appointing a representative. ...
- Know that you can hire legal representation. ...
- If you are mailing documents, send them via certified mail. ...
- Never send Medicare your only copy of a document. ...
- Keep a record of all interactions. ...
How do I write a Medicare reconsideration letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
What should I say in a Medicare appeal?
Explain in writing on your MSN why you disagree with the initial determination, or write it on a separate piece of paper along with your Medicare Number and attach it to your MSN. Include your name, phone number, and Medicare Number on your MSN. Include any other information you have about your appeal with your MSN.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
How long does Medicare have to respond to an appeal for reconsideration?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days.
How do I win a Medicare appeal?
Appeals with the best chances of winning are those where something was miscoded by a doctor or hospital, or where there is clear evidence that a doctor advised something and the patient followed that advice and then Medicare didn't agree with the doctor's recommendation.
How often are Medicare appeals successful?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
How do you write a redetermination letter?
How to Write an Appeal Letter in 6 Simple StepsReview the appeal process if possible.Determine the mailing address of the recipient.Explain what occurred.Describe why it's unfair/unjust.Outline your desired outcome.If you haven't heard back in one week, follow-up.
What is the Medicare redetermination process?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination. A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
Can providers appeal denied Medicare claims?
The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
How many steps are there in the Medicare appeal process?
The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan.
When benefits in a Medicare policy are denied a patient has the right to appeal to quizlet?
Judicial Review. The final level of appeal for Medicare is to request a Judicial Review in Federal District Court. The threshold for review in federal district court in 2016 is $1,460.00 and is calculated each year and may change.
How do I appeal my Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.
How to appeal a Medicare reconsideration?
Include this information in your written reconsideration request: 1 Your name, address, and the Medicare number on your Medicare card [JPG]. 2 The items or services for which you're requesting a reconsideration, the dates of service, and the reason (s) why you're appealing. 3 If you've appointed a representative, include the name of your representative and proof of representation.
What to include in appeal for reconsideration?
If you've appointed a representative, include the name of your representative and proof of representation. Include any other information that may help your case.
How long does it take for a health insurance company to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days. You'll get a fast request if your plan determines, or your doctor tells your plan, that waiting for a standard service decision may seriously jeopardize your: Life. Health.
What level is an appeal sent to?
If the plan decides against you (fully or partially), your appeal is automatically sent to level 2.
How to fill out and sign MAXIMUS online?
Get your online template and fill it in using progressive features. Enjoy smart fillable fields and interactivity. Follow the simple instructions below:
Accredited Business
Guarantees that a business meets BBB accreditation standards in the US and Canada.
How to request a Medicare reconsideration?
There are 2 ways to submit a reconsideration request. 1 Fill out a " Medicare Reconsideration Request Form." [PDF, 180 KB] 2 Submit a written request to the QIC that includes:#N#Your name and Medicare Number#N#The specific item (s) or service (s) for which you're requesting a reconsideration and the specific date (s) of service. See MSN or your redetermination notice for this information.#N#The name of the company that made the redetermination (the company that handles claims for Medicare). or the redetermination notice for this information.#N#An explanation of why you disagree with the redetermination decision.#N#If you've appointed a representative, include the name of your representative.
What is a redetermination notice?
or the redetermination notice for this information. An explanation of why you disagree with the redetermination decision. If you've appointed a representative, include the name of your representative. No matter how you choose to request ...
How long does it take for a QIC to make a decision?
In most cases, the QIC will send you a written response called a "Medicare Reconsideration Notice" about 60 days after the QIC gets your appeal request.
What is a redetermination in Medicare?
A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
How long does it take for a MAC to send a decision?
Generally, the MAC will send its decision (either in a letter, an RA, and/or an MSN) to all parties within 60 days of receipt of the request for redetermination. The decision will contain detailed information on further appeals rights, where applicable.
Can a MAC dismiss a request for redetermination?
A MAC may dismiss a request for a redetermination for various reasons, some of which may be: If the party (or appointed representative) requests to withdraw the appeal. The party fails to file the request within the appropriate timeframe and did not show (or the MAC did not determine) good cause for late filing.
How long does it take for Medicare to be reconsidered?
You'll generally get a decision from the MAC (either in a letter or an MSN) called a "Medicare Redetermination Notice" within 60 days after they get your request. If you disagree with this decision, you have 180 days after you get the notice to request a reconsideration by a Qualified Independent Contractor (QIC).
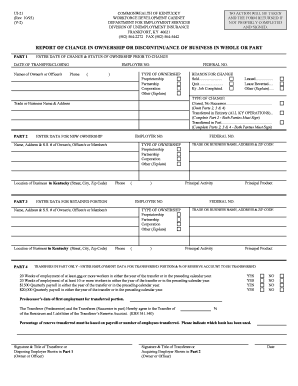
What is a redetermination request?
The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service. An explanation of why you don't agree with the initial determination. If you've appointed a representative, include the name of your representative.
How long does it take for Medicare to make a decision?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days ...
How long does it take to appeal a Medicare payment?
The MSN contains information about your appeal rights. You'll get a MSN in the mail every 3 months, and you must file your appeal within 120 days of the date you get the MSN.
What information do you put on your MSN?
Include your name, phone number, and Medicare Number on the MSN. Include any other information you have about your appeal with the MSN. Ask your doctor, other health care provider, or supplier for any information that may help your case.
How to appeal a disability claim denied for medical reasons?
If you do not wish to appeal a medical decision online, you can use the Form SSA-561, Request for Reconsideration.
What to do if you disagree with a non medical decision?
If You Disagree With A Non-Medical Decision. You may request an appeal online for a "non-medical" decision. If you do not wish to appeal a "non-medical" decision online, you can use the Form SSA-561, Request for Reconsideration. Some examples of "non-medical" decisions are: you were denied another type of benefit, such as retirement or spouse's;