
If you know the name of the form you need, you can search for the document on Medicare.gov or the Centers for Medicare & Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
Full Answer
What is the best Medicare Part D plan?
The best medicare Part D plan for diabetes, cancer or other ongoing illnesses will have coverage during the gap as well as either a low or no deductible. If you have diabetes, look for a plan that is participating in the new Insulin Savings program that launched in 2021.
What drugs are covered on Medicare Part D?
- Tier 1: Preferred generic drugs
- Tier 2: Generic drugs
- Tier 3: Preferred brand drugs and select insulin drugs
- Tier 4: Non-preferred drugs
- Tier 5: Specialty drugs
How to find out if you have Medicare Part D?
How to Find the Best Medicare Part D Drug Plan
- Enter All Your Meds. Start by adding all the medications you take into the Medicare.gov tool, including the dosages, quantity, and frequency.
- Consider the Doughnut Hole
- Get Free Help. In Medicare Part D, that is what you fall into when your annual drug costs (not including premiums) reach $4,430.
What drugs are covered in Part D?
- Oral cancer drugs: Medicare helps pay for some oral cancer drugs you take by mouth if the same drug is available in injectable form or the drug is a prodrug ...
- Oral anti-nausea drugs: Medicare helps pay for oral anti-nausea drugs used as part of an anti-cancer chemotherapeutic regimen if they’re administered before, at, or within 48 hours of chemotherapy or ...
- Self-administered drugs in hospital outpatient settings: Medicare may pay for some self-administered drugs, like drugs given through an IV. ...
Does Part D show on Medicare card?
Primarily, the prescription plan uses the Medicare ID number in record keeping; by checking the Medicare ID number the Part D plan will show on system records. Often, beneficiaries can use the Part D benefits before they receive a member card by simply using their Medicare ID.
How do I prove I have Medicare Part D?
Proof can include your Medicaid card and an award letter from the Social Security Administration (SSA), or your yellow auto-enrollment letter from Medicare.
Can Medicare Part D notices be sent electronically?
CMS allows employers to send Medicare Part D notices electronically and has stated that employers who follow the general electronic disclosure rules set by the U.S. Department of Labor (DOL) for other group health plan information will be deemed to have met their Medicare Part D Notice obligations.
How do you find out what drugs are covered by Medicare?
Get information about specific drug plans and health plans with drug coverage in your area by visiting Medicare.gov/plan-compare or by calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
When did Medicare Part D become mandatory?
The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.
How do you find Evidence of coverage?
Your evidence of coverage (EOC) or Certificate of insurance (COI)Go to the Benefits and coverage plan resources page to view and download your EOC/COI (not available to all members).Contact your Human Resource department for a copy if you have health care through your company.More items...
Who should receive the Medicare Part D notice?
Notice must be provided to all Medicare Part D eligible individuals who are covered by or apply for the employer's drug coverage (active employees, retirees and covered spouses). Medicare Part D eligible individuals are those covered by Medicare because of age (65 and older), disability or end-stage renal disease.
What is a Medicare Part D notice?
Medicare Part D notices must be provided to all Medicare Part D eligible individuals who are covered under or who apply for the plan's prescription drug coverage. The Medicare Part D notice is utilized to inform individuals about the plan's prescription drug coverage status for the next calendar year.
What is the deadline for Part D?
Enrollment Periods This period is from October 15 through December 7 each year. Coverage begins the following January 1. For people who are new to Medicare, the Initial Enrollment Period (IEP) for Part D is 7 months long.
What are two options for Medicare consumers to get Part D prescription drug coverage assuming they meet all eligibility requirements )? Select 2?
There is no other way a Medicare consumer could get Part D prescription drug coverage. They could enroll in a Medicare Supplement Insurance Plan. They could enroll in a Medicare Advantage Plan or other Medicare health plan that includes prescription drug coverage.
Are all Part D formularies the same?
Each Medicare Part D plan has its own unique formulary, meaning that it has its own unique list of drugs the plan covers. Medicare formularies are used to help provide Medicare beneficiaries with affordable and effective medications.
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
How to enroll in Medicare?
Enroll on the Medicare Plan Finder or on the plan's website. Complete a paper enrollment form. Call the plan. Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. When you join a Medicare drug plan, you'll give your Medicare Number and the date your Part A and/or Part B coverage started.
What are the different types of Medicare plans?
You can only join a separate Medicare drug plan without losing your current health coverage when you’re in a: 1 Private Fee-for-Service Plan 2 Medical Savings Account Plan 3 Cost Plan 4 Certain employer-sponsored Medicare health plans
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What happens if you don't get prescription drug coverage?
If you decide not to get it when you’re first eligible, and you don’t have other creditable prescription drug coverage (like drug coverage from an employer or union) or get Extra Help, you’ll likely pay a late enrollment penalty if you join a plan later.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Do you have to have Part A and Part B to get Medicare?
You get all of your Part A, Part B, and drug coverage, through these plans. Remember, you must have Part A and Part B to join a Medicare Advantage Plan , and not all of these plans offer drug coverage. Visit Medicare.gov/plan-compare to get specific Medicare drug plan and Medicare Advantage Plan costs, and call the plans you’re interested in ...
Does Medicare change drug coverage?
The drug coverage you already have may change because of Medicare drug coverage, so consider all your coverage options. If you have (or are eligible for) other types of drug coverage, read all the materials you get from your insurer or plan provider.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
What are some examples of documents you can send to Medicare?
Examples of documents you can send your plan include: A purple notice from Medicare that says you automatically qualify for Extra Help. A yellow or green automatic enrollment notice from Medicare. An Extra Help "Notice of Award" from Social Security. An orange notice from Medicare that says your copayment amount will change next year.
What is a copy of a medicaid card?
A copy of your Medicaid card (if you have one). A copy of a state document that shows you have Medicaid. A print-out from a state electronic enrollment file that shows you have Medicaid. A screen print from your state's Medicaid systems that shows you have Medicaid.
How much does a prescription cost for 2021?
Make sure you pay no more than the LIS drug coverage cost limit. In 2021, prescription costs are no more than $3.70 for each generic/$9.20 for each brand-name covered drug for those enrolled in the program. Contact Medicare so we can get confirmation that you qualify, if it's available.
How long does it take to get a prescription for a syringe?
Your request can take anywhere from several days to up to 2 weeks to process, depending on the circumstances. Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Be sure to tell your plan how many days of medication you have left.
What is an orange notice from Medicare?
An orange notice from Medicare that says your copayment amount will change next year. If you have. Supplemental Security Income (Ssi) A monthly benefit paid by Social Security to people with limited income and resources who are disabled, blind, or age 65 or older.
How long does Medicaid pay for stay?
Or, a copy of a state document showing Medicaid paid for your stay for at least a month. A print-out from your state’s Medicaid system showing you lived in the institution for at least a month. A document from your state that shows you have Medicaid and are getting home- and community-based services.
How to get a fax number for a Medicare plan?
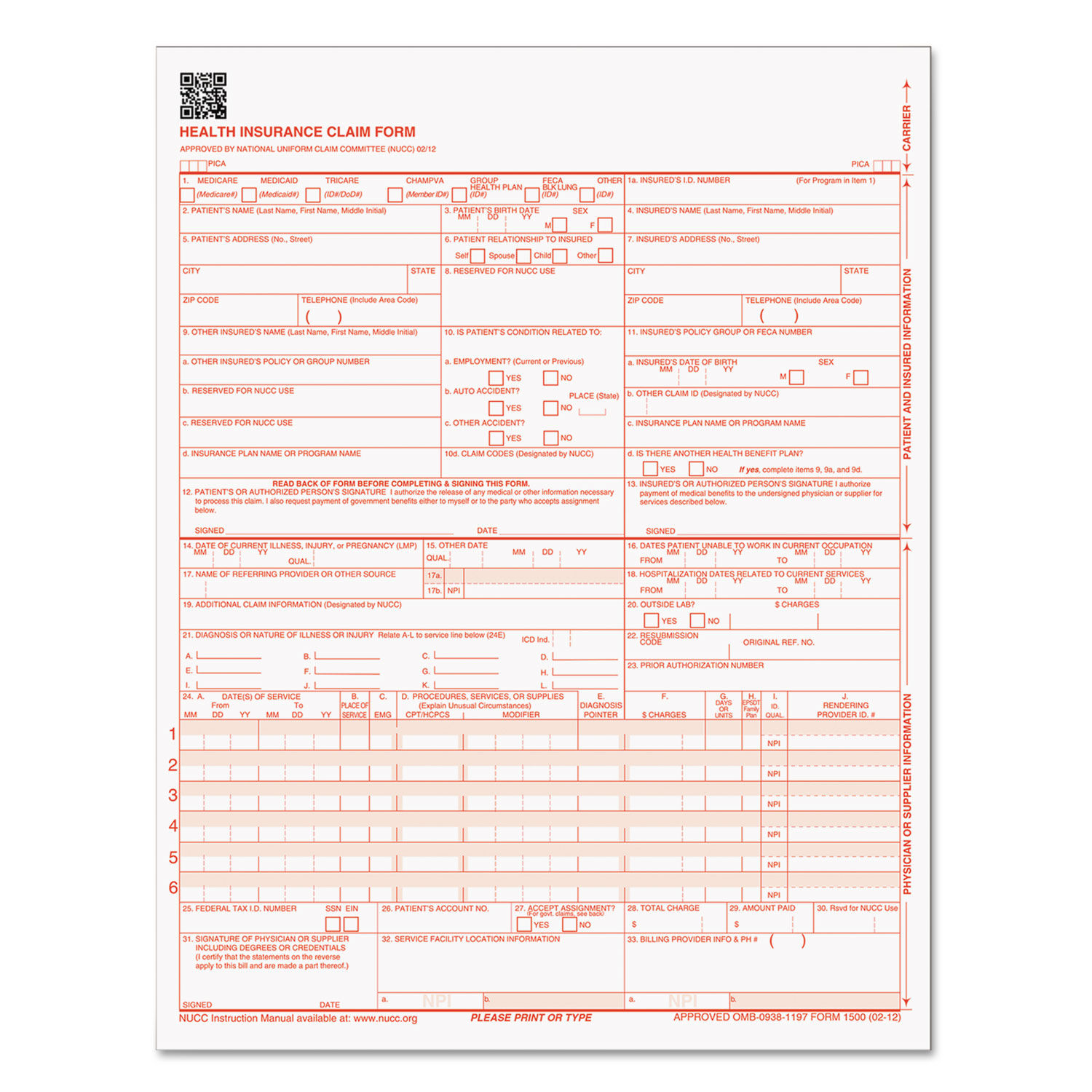
Step 1 – Enter the name, phone number, and fax number of the member’s plan. Step 2 – In the “Patient Information” section, provide the patient’s name, ID number, address, phone number, gender, and date of birth.
What is a prior authorization form for Medicare?
Medicare Prior (Rx) Authorization Form. Medicare members who have prescription drug coverage (Part D) will be covered for almost all their medication costs. Original Medicare members most likely have chosen to join a Medicare Prescription Drug Plan (PDP) for an additional premium.
How long does it take for a health insurance plan to respond?
Call your plan or check on their website to look up the proper mailing address or fax number. Plans must respond within 72 hours of receiving your request form. If the physician feels the request is an emergency situation, an expedited review of 24 hours should take place.
Appointment of Representative Form CMS-1696
If an enrollee would like to appoint a person to file a grievance, request a coverage determination, or request an appeal on his or her behalf, the enrollee and the person accepting the appointment must fill out this form (or a written equivalent) and submit it with the request. (See the link in " Related Links " section).
Request for a Medicare Prescription Drug Coverage Determination
An enrollee, an enrollee's representative, or an enrollee's prescriber may use this model form to request a coverage determination, including an exception, from a plan sponsor.
Request for a Medicare Prescription Drug Redetermination
An enrollee, an enrollee's representative, or an enrollee's prescriber may use this model form to request a redetermination (appeal) from a plan sponsor.
Request for Reconsideration of Medicare Prescription Drug Denial
An enrollee or an enrollee's representative may use this model form to request a reconsideration with the Independent Review Entity. You may download this form by clicking on the link in the " Downloads " section below.
What do you need to know before enrolling in a Part D plan?
The most important preparation you can do before finding a Part D plan is recording information about your medications.
How does dosage affect Part D?
Your dosage can affect your final cost or enact certain plan restrictions depending on the Part D plan. The frequency of the medication. The number of pills you take also affects the cost, so double check how often you take your medication and write it down. Once you have these recorded, you’ll be able to compare plans, apples-to-apples.
When is the best time to sign up for Part D?
If you don’t have creditable drug coverage or health insurance from a current employer, the best time to sign up for Part D is during your 7-month initial enrollment period (IEP) to avoid penalties. Under your IEP, you have a 7-month window that opens 3 months before you turn 65 and closes at the end of the 3rd month following your birthday month.
Is Medicare Part D a good program?
Although Medicare is not without its faults, one thing is clear: Medicare Part D has been a successful program. With nearly 70% of all beneficiaries enrolled in Part D, this optional add-on to Original Medicare is a popular way to lower drug costs. 1. But before diving into the deep end of Part D plans, you’ll want to perform due diligence ...
What is an applicant in Medicare?
Applicant is a non-governmental legal entity that intends to enter into a Medicare Prescription Drug Plan contract with CMS. (For applicants applying for a new PDP contract.) Applicant is a legal entity that intends to enter into a Medicare Prescription Drug Plan addendum to its contract with CMS.
When was Medicare established?
The Medicare Prescription Drug Benefit program was established by section 101 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), as amended, and is codified in sections 1860D-1 through 1860D-43 of the Social Security Act (the Act).
