
To check the status of Medicare Part A (Hospital Insurance) or Medicare Part B (Medical Insurance) claims: Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it.
Full Answer
How can I check if my health insurance is active?
The database linked to the platform will assist in:
- Assessing performance.
- Ensure seamless flow of digital information.
- Automate the healthcare system
- Give members the convenience of carrying only one card.
- Keep medical records for the patient, all in one place - This will help in making effective medical decisions by keeping accurate clinical records & ensuring quick access to them.
How to check if a provider is enrolled in Medicare?
Check Provider Enrollment Application Status. This inquiry tool can be used to check on the status of your application. How to Search. To perform a search please enter into a field below either a valid Case Number/Web Tracking ID (Option 1) or a valid National Provider Identifier (NPI) and last five digits of the Tax Identification Number (TIN ...
How to confirm Medicare coverage?
We rate the statement Mostly False. Centers for Medicare & Medicaid Services, "Four in Ten New Consumers Spend $10 or Less Per Month for HealthCare.Gov Coverage Following Implementation of American Rescue Plan Tax Credits," June 14, 2021 Centers for ...
How much is taken out of your check for Medicare?
You as the employer must pay 6.2% with no limit. The Medicare withholding rate is gross pay times 1.45 %, with a possible additional 0.9% for highly-paid employees. Your portion as an employer is also 1.45% with no limit, but you don’t have to pay the additional 0.9% For a total of 7.65% withheld, based on the employee’s gross pay.

How do I check the status of my Medicare provider?
Providers with additional questions about checking the status of their claims should call the Telephone Service Center (TSC) at 1-800-541-5555.
How do you check if your Medicare is active online?
If you applied for Medicare online, you can check the status of your application through your Medicare or Social Security account. You can also visit the Check Enrollment page on Medicare.gov and find information about your enrollment status by entering your: ZIP code. Medicare number.
How do I find out if a patient has Medicare?
The best way to check eligibility and enroll in Medicare online is to use the Social Security or Medicare websites. They are government portals for signing up for Medicare, and they offer free information about eligibility.
How do I check if a provider is enrolled in Pecos?
To determine if you have a current enrollment record in the PECOS, you can do the following:Utilize the national file of Medicare physicians and non-physician practitioners who are eligible to order / refer and have current enrollment records in the PECOS. ... Utilize Internet-based PECOS.More items...•
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
Why would my Medicare be inactive?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
How do I find out if my Medicare is noridian eligible?
0:237:54To begin an eligibility inquiry select eligibility from the top navigation bar or select startMoreTo begin an eligibility inquiry select eligibility from the top navigation bar or select start inquiry. First select the tax id mpi. And ptan and program from the drop down menus.
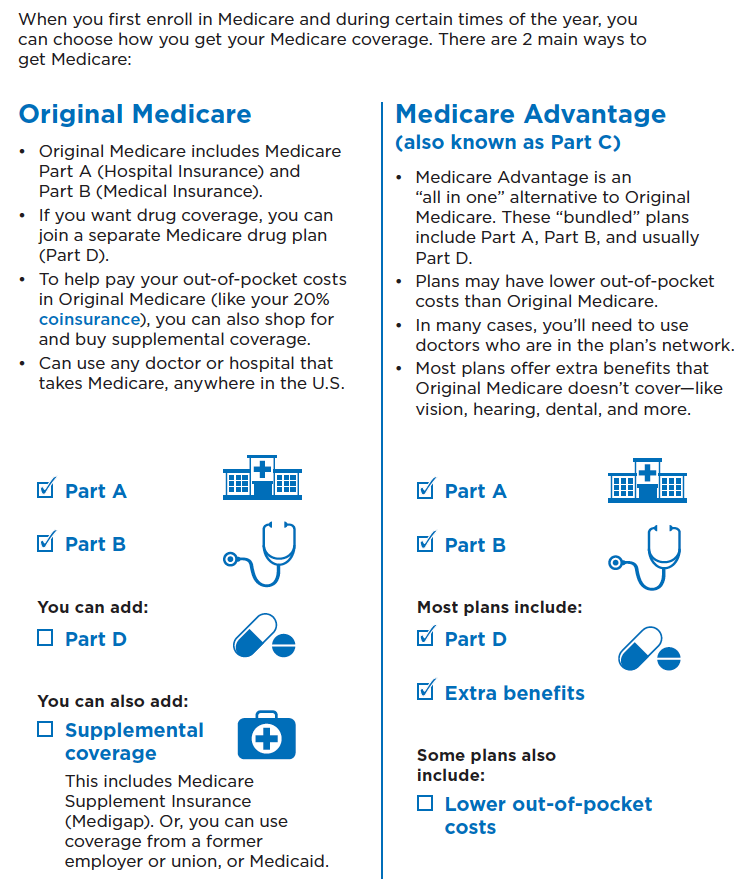
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
How do I find my Medicare item number?
You can find the item number on the account or receipt. It's a set of numbers and can be up to 8 numbers long. Enter the: Item number.
Is NPI the same as Medicare provider number?
Yes, you must have an NPI to do business with any health insurance company including Medicare. But, your NPI is NOT your Medicare provider number. You may obtain an NPI through NPPES by applying online, click here to go to their website. It's a quick and simple process.
What is the Pecos database?
The Provider Enrollment, Chain and Ownership System (PECOS) is a database of physicians or non-physician practitioner who are enrolled with Medicare. It allows registered users to securely and electronically submit and manage Medicare enrollment information.
Is Pecos ID same as Medicare number?
The following walk-thru explains how a user can find their Medicare ID number in PECOS. Medicare numbers are also known as the CCN, P-Tan, Oscar, Provider number, or Medicare ID.
Add your favorite providers
Keep a list of all your favorite providers – Select the button above to find and compare providers. Then, select the heart icon next to any of the providers to add them to your list of favorites.
Not sure what type of provider you need?
Use our provider search tool to find quality data, services offered, and other information for these type of providers:
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
Can BCRC provide beneficiary entitlement data?
Information regarding beneficiary entitlement data. Current regulations do not allow the BCRC to provide entitlement data to the provider. Insurer information. The BCRC is permitted to state whether Medicare is primary or secondary, but cannot provide the name of the other insurer.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
Can you get Medicare for electronic health records?
It is possible that you may not be able to receive incentive payments from Medicare for meaningful use of certified electronic health records. These incentive payments are authorized by the American Recovery and Reinvestment Act of 2009. More information on this initiative, also known as HITECH, is available at ...
Do you need an enrollment record for PECOS?
You need an approved enrollment record in PECOS to continue to refer or order items or services for your Medicare patients. If you do not have a current and active Medicare enrollment record, it is imperative that you take the necessary action to establish your enrollment record as soon as possible.
Coordination of Benefits Overview
Information Gathering
Provider Requests and Questions Regarding Claims Payment
Medicare Secondary Payer Records in CMS's Database
Termination and Deletion of MSP Records in CMS's Database
Contacting The BCRC
Contacting The Medicare Claims Office
- Contact your local Medicare Claims Office to: 1. Answer your questions regarding Medicare claim or service denials and adjustments. 2. Answer your questions concerning how to bill for payment. 3. Process claims for primary or secondary payment. 4. Accept the return of inappropriate Medicare payment.
Coba Trading Partner Contact Information
mln Matters Articles - Provider Education