These will reject with Claim Adjustment Reason Code (CARC) 16 and Remittance Advice Code (RARC) N245. If your claim rejects, you must submit a new claim with the correct MSP type. Report the MSP Insurance Type Code in Loop/Segment 2000B/SBR05 of the electronic claim.
Full Answer
What does denial code 24 mean?
24: Denial Code 24 described as "Charges are covered by a capitation agreement/ managed care plan". 1) Get Claim Denial date? 2) Verify, is the beneficiary enrolled in Medicare Advantage plan and get insurance name, id#, conctact#, mailing address? 3) Claim number and Calreference number Note: Submit the claim to correct payor: 26
What does denial code 97 mean on claim form?
Note: If its valid diagnosis and procedure code, then you have rights to appeal with supporting documentation. Denial code - 97 described when "The benefit for this service is included in the payment or allowance for another service/procedure that has already been adjudicated". 1) Claim denial date?
What is the remark code for Medicare n425?
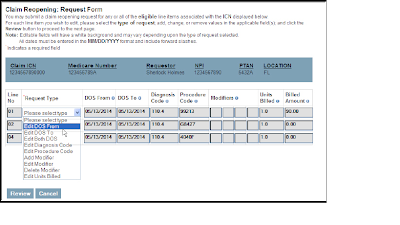
Remark Code: N425 Statutorily excluded. Common Reasons for Denial Non-covered charge(s). Medicare does not pay for this service/equipment/drug. Next Step If billed incorrectly (such as inadvertently omitting a required modifier), request a reopening. Utilize the Noridian Modifier Lookup Toolto ensure proper modifiers are included on claim
How do I review the reason or remark code for denial?
Select the Reason or Remark code link below to review supplier solutions to the denial and/or how to avoid the same denial in the future. The Washington Publishing Company publishes the CMS -approved Reason Codes and Remark Codes .

What does denial code N245 mean?
Effective for claims processed on or after April 27, 2017, failure to supply the correct MSP type will result in a return unprocessable claim (RUC) denial with claim adjustment reason code (CARC) code 16 and remittance advice remark code (RARC) N245.
What is Medicare denial code Co 22?
In circumstances where there is more than one potential payer, not submitting claims to the proper payer will lead to denial reason code CO-22, indicating this care may be covered by another payer, per COB.
Why do Medicare claims get denied?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
What does N130 denial mean?
This service/equipment/drug is not covered under the patient's current benefit plan. Remark Code: N130.
What is reason 22 code?
Reason Code: 22. This care may be covered by another payer percoordination of benefits. Remark Codes: MA 04. Secondary payment cannot be considered without theidentity of or payment information from the primary payer. The information waseither not reported or was illegible.
What is a Co 24?
CO 24 – charges are covered under a capitation agreement/managed care plan: This reason code is used when the patient is enrolled in a Medicare Advantage (MA) plan or covered under a capitation agreement. This claim should be submitted to the patient's MA plan.
How do I fight Medicare denial?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
Can you resubmit a rejected Medicare claim?
Claims rejected as unprocessable cannot be appealed and instead must be resubmitted with the corrected information. The rejected claim will appear on the remittance advice with a remittance advice code of MA130, along with an additional remark code identifying what must be corrected before resubmitting the claim.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is denial Co 29?
Insurance will deny the claim with denial code CO 29 – the time limit for filing has expired, whenever the claims submitted after the time frame. The time limit is calculated from the date service provided.
What does N706 remark mean?
N706. 4D. DENIED - DOCUMENTATION DOES NOT JUSTIFY PROC/MODIFIER BILLED.
What does PR 119 mean?
Denial code and Reason CO -119 Benefit maximum for this time period or occurrence has been reached. Check Benefit Information through website/Calls. If NO – Call the carrier and send the claim to reprocess. PR – 119 Benefit maximum for this time period or occurrence has been reached.