
Does Medicare pay for services performed by home health aide?
that Medicare covers, and how to get those benefits through Medicare. If you get your Medicare benefits through a Medicare health plan (not Original Medicare) check your plan’s membership materials, and contact the plan for details about how the plan provides your Medicare-covered home health benefits.
Is a home health aide a bad job?
Aug 30, 2019 · Medicare has several requirements to cover home health aide services and other home health care: Your doctor must write a formal treatment plan specifying the home health services you need and certifying that you need the services to improve or maintain your condition.
What makes a great home health aide?
In order to qualify for benefits, the following five requirements must be met, according to the Medicare Learning Network’s (MLN) pamphlet, “Medicare & Home Health Care.” 1. You’re under the care of a doctor, and you’re getting services under a plan of care established and reviewed regularly by a doctor.
What is the starting pay for a home health aide?
Home health aides through Medicare are approved for only up to 21 days. If you need longer-term care, then you may be eligible for a home health aide through your state via a Medicaid waiver, says Nicole Wolf, RN, manager of Clinical Health Services at Aetna®. Your hospital, doctor or insurance case manager can help you find out if you qualify.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
How many hours of home health aides can Medicare cover?
For example, the plan may choose to cover up to 50 hours per year of home health aide services, or 20 transportation trips per year.
How long does Medicare cover home health aides?
Medicare generally covers fewer than seven days a week of home health aide visits, and fewer than eight hours of care per visit.
How long does home health care take before Medicare benefits apply?
The home health care must follow a qualifying hospital stay of at least three days before your Medicare benefits apply. If you haven’t had a hospital stay, Medicare Part B might still cover home health care visits.
What is Medicare Advantage?
Medicare Advantage plans are offered by private insurance companies. They must provide the same coverage as Original Medicare at a minimum. Some many plans offer additional benefits to their members, including expanded coverage for home health care.
What does it mean to be homebound?
You must be certified by your doctor as homebound, which means you are unable to leave home without assistance or special transportation. Medicare may consider you homebound if leaving the house requires “considerable and taxing effort.”. Your doctor must monitor the services you receive at home.
Does Medicare cover home health?
If you need Medicare home health care after a hospitalization or due to a condition that keeps you homebound, Medicare might cover a home health aide. Here’s the information you need to know about Medicare coverage of home health services. A Medicare Advantage plan might cover some home health services.
Does Medicare Part B cover home care?
If you haven’t had a hospital stay, Medicare Part B might still cover home health care visits. Your doctor would need to recommend these visits as part of a formal, written treatment plan. Part B generally covers 80% of allowable charges for durable medical equipment and devices you need for your treatment at home. Your Part B deductible applies.
What does it mean to be homebound?
To be homebound means: You have trouble leaving your home without help (such as a cane, wheelchair, walker, crutches, special transportation or help from another person) because of an illness or injury, or leaving your home isn’t recommended because of your condition. 5. As part of your certification of eligibility, a doctor, ...
Do parents have rights to health care?
You also may be comforted by the fact that your parents have rights as far as their health care is concerned. These include having their property treated with respect; to be told, in advance what care they’ll be getting and when their plan of care is going to change; to participate in their care planning and treatment.
Do you need a therapist for your aging parents?
You are doing everything you can for your aging parents, but sometimes it comes to the point where that is not enough. After a hospitalization, or to simply maintain or slow the decline of their health, Mom or Dad may need skilled therapists and nurses. This new twist in caring for Mom and Dad raises many questions.
Does Medicare cover home aides?
Medicare also covers continuous health care but on a different level. It only covers a percentage of the cost. Unfortunately, home aides that help with housework, bathing, dressing and meal preparations are not covered by Medicare.
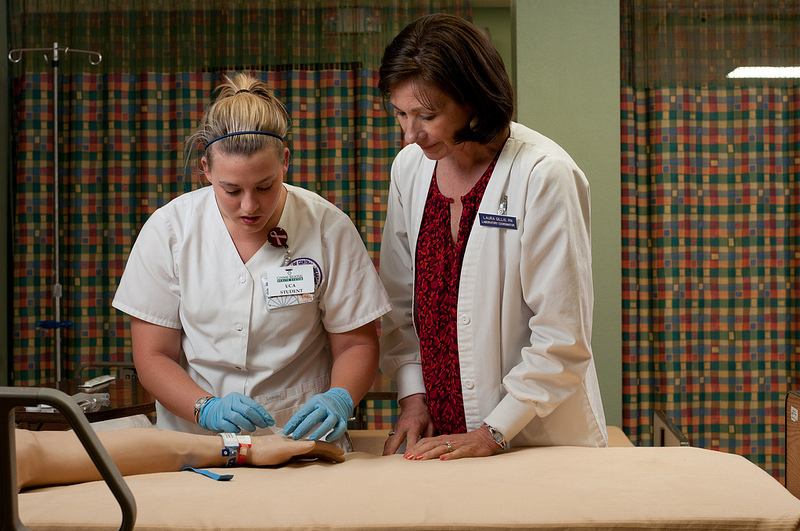
What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
What education do you need to be a home health aide?
According to the U.S. Bureau of Labor Statistics, the typical educational level for a home health aide is a high school diploma or equivalent. Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
Is long term care insurance part of Medicare?
Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare . These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
How to start home health care?
Starting home health care 1 If you are in the hospital: A hospital social worker or discharge planner should arrange for a Medicare-certified home health agency (HHA) to visit you and assess your condition. If you qualify, you should receive home health care after being discharged. 2 If you are at home or leaving a SNF: Speak to your doctor about your home health needs and ask for a list of Medicare-certified HHAs. You, your doctor, or a caregiver should be able to call an HHA directly and ask them to visit your home and assess your condition.#N#You should also be able to find local HHAs through your hospital discharge planning office, 1-800-MEDICARE, or the Eldercare Locator.
How often should a HHA recertify a home health plan?
Your doctor must certify that you qualify for Medicare’s home health benefit, sign off on the plan of care, and recertify the plan every 60 days.
How to find an HHA?
You should also be able to find local HHAs through your hospital discharge planning office, 1-800-MEDICARE, or the Eldercare Locator.
What is a HHA in hospital?
If you are in the hospital: A hospital social worker or discharge planner should arrange for a Medicare-certified home health agency (HHA) to visit you and assess your condition. If you qualify, you should receive home health care after being discharged.
What are the eligibility requirements for Medicaid home care?
Eligibility Requirements for Medicaid Home Care. In order to be eligible for Medicaid, and hence, in-home care, there are eligibility requirements that must be met. In addition to being a resident in the state in which one applies, there are also financial and functional needs that must be met.
How much income can I have on Medicaid in 2021?
As a general rule of thumb, in 2021, 300% of SSI is used as the income limit. This means that an individual cannot have more than $2,382 / month in income. There is also an asset limit, which in most cases, is $2,000.
What is HCBS waiver?
HCBS Medicaid Waivers. Home and Community Based Services Medicaid wa ivers, also known as Section 1915 (c) waivers, are another way in which Medicaid offers in-home services and supports to promote independent living of elderly persons.
What is regular state medicaid?
With regular state Medicaid, also referred to as original Medicaid and classic Medicaid, the federal government requires that states make home health benefits available to those in need.
Do you need HCBS for nursing home?
On the other hand, for HCBS Medicaid waivers, a level of care consistent to that which is provided in a nursing home is generally required.
Can Medicaid recipients direct their own care?
Many states allow Medicaid recipients to direct their own in-home care. This model of receiving services is called consumer directed care, participant directed care, cash and counseling, and self-directed care, and often allows care recipients to hire relatives as paid caregivers. Some states even allow spouses to be hired, ...
Does Medicaid pay for nursing home care?
Yes, Medicaid will pay for in-home care, and does so in one form or another, in all 50 states. Traditionally, Medicaid has, and still continues to, pay for nursing home care for persons who demonstrate a functional and financial need. However, in-home care provides an alternative for seniors who require assistance to remain living at home, ...
