Let’s get started
- Step one: Request participation. You can do this by choosing a link below. ...
- Step two: Review your contract
- Step three: Complete credentialing. We’ll get your credentialing application from the Council for Affordable Quality Healthcare’s ProView® (CAQH)* to begin the credentialing process.
Full Answer
How to credential a provider with Medicare?
- Obtain DMEPOS accreditation from a CMS-approved organization
- Enroll in the Medicare program as a DMEPOS Supplier
- Post a surety bond to the National Supplier Clearinghouse (NSC)
How long does it take to get approved for Medicare?
The process should take 21 to 30 days for getting approved, and then people can enjoy the services. The person getting the benefits of Medicare part B should have to pay the monthly premium. The monthly premium would not be the same for everyone.
How to become Medicare Certified Provider?
- Public agency is an agency operated by a State or local government. Examples include State-operated HHAs and county hospitals. ...
- Nonprofit agency is a private (i.e., nongovernmental) agency exempt from Federal income taxation under §501 of the Internal Revenue Code of 1954. ...
- Proprietary agency is a private, profit-making agency or profit-making hospital.
What are the requirements for Medicare certification?
- The date the plan of care being sent for certification becomes effective (the initial evaluation date is acceptable)
- Diagnoses
- Long term treatment goals
- Type, amount, duration and frequency of therapy services
- Signature, date and professional identity of the therapist who established the plan

What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
How long does it take for Medicare to approve a provider?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
Is accreditation mandatory for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider's or supplier's ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.
How do providers bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
How long is the credentialing process?
90 to 120 daysA standard credentialing process takes from 90 to 120 days based on the guidelines. In some cases, the process may be completed within 90 days and sometimes, it can take more than 120 days. Keeping in mind, the complexities in medical credentialing, it is best to hire experts in the field.
Does Medicare pay non-participating providers?
Non-participating providers haven't signed an agreement to accept assignment for all Medicare-covered services, but they can still choose to accept assignment for individual services. These providers are called "non-participating."
What does CMS certification mean?
The CMS Certification number (CCN) replaces the term Medicare Provider Number, Medicare Identification Number or OSCAR Number. The CCN is used to verify Medicare/Medicaid certification for survey and certification, assessment-related activities and communications. The RO assigns the CCN and maintains adequate controls.
What is the difference between Medicare and Joint Commission?
CMS has been designated as the organization responsible for certification of hospitals, deeming them certified and meeting established standards. The Joint Commission sets its standards and establishes elements of performance based on the CMS standards.
What is a CMS designation?
CMS Designation. About the Compensation Management Specialist (CMS) designation. The Compensation Management Specialist (CMS) designation is rooted in the principles of human resources, compensation design and administration, and executive compensation.
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
Does Medicare pay more than billed charges?
Consequently, the billed charges (the prices that a provider sets for its services) generally do not affect the current Medicare prospective payment amounts. Billed charges generally exceed the amount that Medicare pays the provider.
Complete The Medicare Enrollment Application
Once a psychologist has an NPI, the next step is to complete the Medicare Enrollment Application. Complete the application through Medicares online enrollment system known as the Provider Enrollment, Chain, and Ownership System . Although PECOS is designed to be paperless, providers can print a copy of the application for their records.
Can Interns Be Credentialed
I am post-Masters but I do not have my license yet. Can I be credentialed?
Discover A Simple Efficient Credential Tracking Solution In Smartsheet
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team and adapt as those needs change.
License For Use Of Dental Procedure Codes Fourth Edition
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED I ACCEPT, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
Pecos For Medicare Applications
We highly recommend utilizing PECOS for all Medicare applications. This is primarily due to the timeline associated with PECOS applications vs those completed on paper.
How Does Provider Credentialing Work
Provider credentialing is the process of establishing that medical providers have proper qualifications to perform their jobs. This requires contacting a range of organizations, including medical schools, licensing boards, and other entities, to verify that the providers have the correct licenses and certificates.
Put The New Physician On The Speaking Circuit
If you cant fill the physicians schedule due to credentialing, get the physician out to meet other physicians and the community.
Medicare basics
Start here. Learn the parts of Medicare, how it works, and what it costs.
Sign up
First, you’ll sign up for Parts A and B. Find out when and how to sign up, and when coverage starts.
What is Medicare credentialing?
Medicare approves a variety of individual practitioners, agencies and facilities to provide high-quality care to Medicare recipients. Medicare credentialing standards vary depending on the type of services you are providing.
How to become in network for Medicare?
The general steps for being considered in-network for Medicare patients are as follows: Obtain a National Provider Identifier (NPI) by applying on the National Plan and Provider Enumeration System Website. Complete a Medicare enrollment application ...
How often do you need to resubmit Medicare enrollment application?
Once you meet Medicare credentialing standards and have been approved as a provider, you need to keep up your credentials. Every three years, you will need to resubmit the Medicare enrollment application CMS-855I.
How long does it take for Medicare to bill?
Once you submit all of your paperwork, expect it to take two to three months for your application to be reviewed and either accepted or denied. Once you are an approved Medicare provider, you will be able to bill retroactively for all services provided during the waiting period.
How long does it take to get a psychologist's license?
Once you submit all of your paperwork, expect it to take two to three months for your application to be reviewed and either accepted or denied.
Can Medicare claim be rejected?
Medicare claims can involve a lot of time and effort, including time required to resubmit claims, and finding the right claims procedures for your specialty can involve trial and error. Some people hire outside services to help simplify this process, as they already have a wealth of experience about the fastest way to have claims approved without rejections.
Does Medicare require a license?
Medicare will require you to meet all of the credentialing and licensing requirements of your field. As such, be prepared to provide the following documentation as part of the application process:
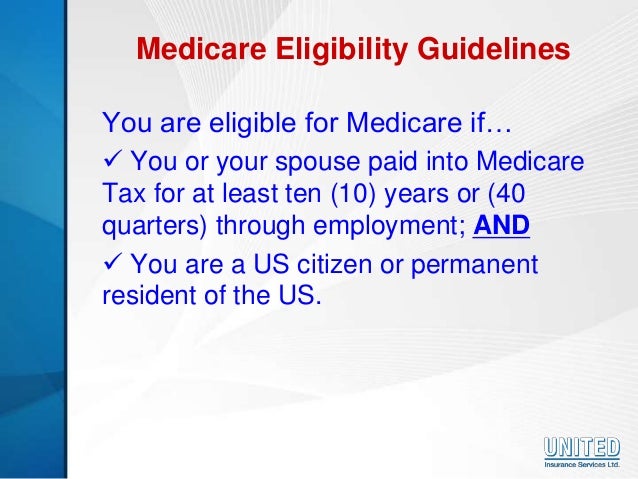
When do you get Medicare if you have Social Security?
If you already get benefits from Social Security or the Railroad Retirement Board, you are automatically entitled to Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) starting the first day of the month you turn age 65. You will not need to do anything to enroll.
What is the Medicare eligibility tool?
The Medicare.gov Web site also has a tool to help you determine if you are eligibile for Medicare and when you can enroll. It is called the Medicare Eligibility Tool.
What is a medical credential?
Insurance Credentialing: Also known informally as “getting on insurance panels,” this term refers to a health insurance company verifying a physician’s credentials. Every health insurance company checks the credentials of a physician before it includes the doctor as an in-network provider.
What Is Provider Credentialing in Healthcare?
Provider credentialing in healthcare is the process by which medical organizations verify the credentials of healthcare providers to ensure they have the required licenses, certifications, and skills to properly care for patients.
What is healthcare provider credentialing?
Healthcare provider credentialing involves many parties and moving parts. Your doctor — and other healthcare providers — all need to prove they have the education, training, and skills required to properly care for patients. At the same time, healthcare oversight organizations monitor the work of medical providers to evaluate, among other matters, reports of improper care. All of this reporting and monitoring must be continually checked, both by healthcare facilities that employ providers and by health insurance companies that want to issue an approved provider lists.
How to get information from a healthcare provider?
A healthcare facility or health insurance plan asks the provider for information on his or her background, licenses, education, etc. The provider may submit the information in a questionnaire through email or through software.
Which entity regulates or provides standards for credentialing of providers?
Entities That Regulate or Provide Standards for Credentialing of Providers. The federal Centers for Medicare & Medicaid Services (CMS) and the Joint Commision on Accreditation of Healthcare Organizations both require that healthcare providers be credentialed.
How often do you need to be re-credentialed?
Healthcare providers need to be re-credentialed at least every three years. Some healthcare facilities or insurance companies perform recredentialing even more often.
How long does it take to get a physician credentialed?
Under the most efficient circumstances, a physician can be credentialed to work at a hospital or credentialed and approved to be in-network for a health insurance company in 30 days. More often, the process takes 60 to 90 days. And on occasion — especially with insurance companies — it can take six months or more.