You need a provider number to claim, bill, refer or request Medicare services. You must be registered with the Australian Health Practitioner Regulation Agency (Ahpra) or an approved registration body to apply for one.
- Step 1: Get an NPI.
- Step 2: Complete the Medicare Enrollment Application. Enroll using PECOS,i the online Medicare enrollment system. ...
- Step 3: Work with Your MAC.
How to verify Medicare eligibility?
- Provider Registration
- Verify Eligibility
- CoverRx
- Managed Care Organizations
- Medicare/Medicaid Crossover Claims
- Miscellaneous Provider Forms
- Pharmacy
- Report Provider Fraud
- Current P.O. Box List
- Electronic Data Interchange
What are the elegibility criteria of Medicare?
The updated Medicare recommendation is also an important step forward in addressing racial disparities associated with lung cancer, as the expanded criteria includes more individuals from Brown and Black communities.
Where to check Medicare eligibility?
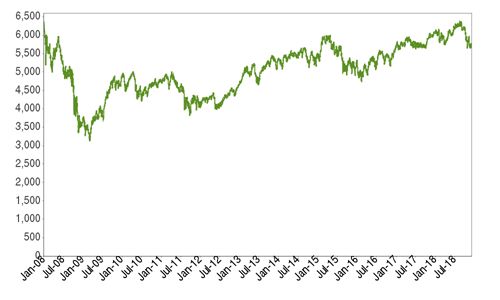
Stop Googling for information and check out Benzinga Pro. You will never again be left in the dark on when a stock moves. You’ll have what you need to act in real-time — before the crowd.
What are the requirements to receive Medicare?
- Scope of Coverage. Rural health clinics/federally qualified health centers. ...
- Covered Personnel. The IFR requires vaccinations for staff who routinely perform care for patients and clients inside and outside of the facility, such as home health, home infusion therapy, hospice, ...
- Definition of Full Vaccination. ...
- Exemptions. ...
How do you become eligible for Medicare?
The best way to check eligibility and enroll in Medicare online is to use the Social Security or Medicare websites. They are government portals for signing up for Medicare, and they offer free information about eligibility.
Which of the following are steps to becoming a Medicare provider?
Applying to become a Medicare providerStep 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ... Step 2: Complete the Medicare Enrollment Application. ... Step 3: Select a Specialty Designation.
How long does it take for Medicare to approve a provider?
A limited sample of 500 Medicare provider enrollment applications processed by nCred with various Medicare intermediaries around the country reveals an average time to completion of 41 days. That average consist of the time that an application is submitted to a carrier until the time the carrier notifies of completion.
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.
Is Pecos enrollment mandatory?
It is a database where physicians register with the Centers for Medicare and Medicare Services (CMS). CMS developed PECOS as a result of the Patient Protection and Affordable Care Act. The regulation requires all physicians who order or refer home healthcare services or supplies to be enrolled in Medicare.
Does Medicare require board certification?
Perhaps more convincingly, the CMS does not require board certification for provider enrollment in the Medicare program, which covers over 55 million elderly, disabled, and otherwise vulnerable Americans.
How long is the credentialing process?
90 to 120 daysA standard credentialing process takes from 90 to 120 days based on the guidelines. In some cases, the process may be completed within 90 days and sometimes, it can take more than 120 days. Keeping in mind, the complexities in medical credentialing, it is best to hire experts in the field.
How long does it take to get credentialed with Caqh?
HSCSN will only accept CAQH applications. How long does the credentialing process take? On average, complete applications are processed within 60 days.
What is Pecos?
PECOS is the online Medicare enrollment management system which allows you to: Enroll as a Medicare provider or supplier. Revalidate (renew) your enrollment. Withdraw from the Medicare program. Review and update your information.
What is the process of credentialing?
Credentialing is a formal process that utilizes an established series of guidelines to ensure that patients receive the highest level of care from healthcare professionals who have undergone the most stringent scrutiny regarding their ability to practice medicine.
What are the steps involved in the credentialing process?
6 Key Steps In Provider CredentialingThe Importance of Credentialing.#1 Identify the Required Documents.#2 Prioritize Insurers.#3 Check for Accurate Information.#4 Completing the CAQH.#5 Wait for Verification.#6 Following Up.#7 Recertification.More items...
How often does a provider need to be credentialed?
every three yearsHealthcare providers need to be re-credentialed at least every three years. Some healthcare facilities or insurance companies perform recredentialing even more often.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months. ( Note: If you have Lou Gehrig's disease, your Medicare benefits begin the first month you get disability benefits.)
When did Medicare start providing prescription drugs?
Since January 1, 2006, everyone with Medicare, regardless of income, health status, or prescription drug usage has had access to prescription drug coverage. For more information, you may wish to visit the Prescription Drug Coverage site.
Medicare basics
Start here. Learn the parts of Medicare, how it works, and what it costs.
Sign up
First, you’ll sign up for Parts A and B. Find out when and how to sign up, and when coverage starts.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
Can BCRC provide beneficiary entitlement data?
Information regarding beneficiary entitlement data. Current regulations do not allow the BCRC to provide entitlement data to the provider. Insurer information. The BCRC is permitted to state whether Medicare is primary or secondary, but cannot provide the name of the other insurer.
How long before Medicare card is sent out?
We’ll mail you a welcome package with your Medicare card 3 months before your Medicare coverage starts.
How long after you sign up for Part A do you have to sign up for Part B?
You get Part A automatically. If you want Part B, you need to sign up for it. If you don’t sign up for Part B within 3 months after your Part A starts, you might have to wait to sign up and pay a monthly late enrollment penalty.
How long do you have to sign up for Part A?
You get Part A automatically. If you want Part B, you need to sign up for it. If you don’t sign up for Part B within 3 months of turning 65, you might have to wait to sign up and pay a monthly late enrollment penalty.
How to contact railroad retirement board?
If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
What is personal care?
Custodial or personal care (like bathing, dressing, or using the bathroom), when this is the only care you need
Does Medicare change home health benefits?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process. For more information, call us at 1-800-MEDICARE.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
Does Medicare cover home health services in Florida?
This helps you and the home health agency know earlier in the process if Medicare is likely to cover the services. Medicare will review the information and cover the services if the services are medically necessary and meet Medicare requirements.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.