Obtaining Conditional Payment Letter from Medicare
- Is your client a medicare recipient? In your initial meeting with your client ask them if they are a medicare recipient,...
- Initial Claim Call medicare personal injury department at 1-800-999-1118 to open the initial claim.
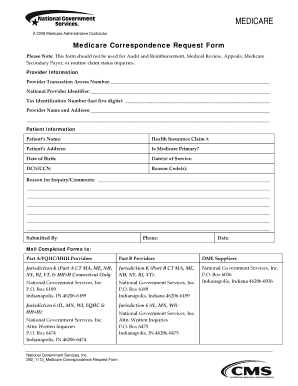
- Representation Fax a medicare representation letter and a signed medicare proof of representation...
How do you write a letter for payment received?
Tips for writing a letter for requesting payment
- Express gratitude for doing business with you
- Use courteous and sincere language
- Mention the urgency of the dues to be paid on time for account purposes
- Highlight details about the goods or services supplied
- Give details like reference numbers of the delivery
- Highlight the outstanding amount of money the customer has not paid
What is conditional payment?
• A conditional payment is a payment that Medicare makes. for services where another payer may be responsible. This. conditional payment is made so that the Medicare beneficiary won’t have to use their own money to pay the bill.
What term explains Medicare payments and denials?
Medicare denial code and Description A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service.
What is conditional billing?
ifyou are contractually obligated to accept an amount less than the total charges and higher than the payment received as your payment in full.
How to get conditional payment information?
How to remove CPL from Medicare?
What does BCRC do with conditional payment?
What is a CPL for Medicare?
How long does a CPN take to respond to a judgment?
When should a CPL be reported to the BCRC?
How long does it take to get a demand letter from a court?
See more
About this website
What is a conditional payment notice?
conditional payment is made so that the Medicare beneficiary won't have to use their own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is secured.
When would Medicare make a conditional payment to a beneficiary?
MSP provisions allow conditional payments in certain situations when the primary payer has not paid or is not expected to pay within 120 days after receipt of the claim for specific items and/or services. Medicare makes these payments “on condition” that it will be reimbursed if it is shown another payer is primary.
Do I have to pay back conditional payments?
If you continue to certify for benefits while we review, you may have to pay back any conditional payments you received if we later find you ineligible.
What is a Medicare demand letter?
When the most recent search is completed and related claims are identified, the recovery contractor will issue a demand letter advising the debtor of the amount of money owed to the Medicare program and how to resolve the debt by repayment. The demand letter also includes information on administrative appeal rights.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
What is conditional Medicare Part A?
The conditional enrollment process allows a person to apply for Premium-Part A but only get the coverage if the State approves the QMB application, whereby the State will pay the Part A premiums. If the State denies the QMB application, the person will not be enrolled in Premium-Part A.
What is notice of conditional payment pending review?
Conversation. Once a conditional payment has been processed, EDD will mail a Notice of Conditional Payment Pending Eligibility Review (DE 5400). If eligible, an Additional Instructions (DE 238) notice will be sent to inform you what weeks were found eligible for benefits.
How does Medicare calculate final demand?
Step number two: take the gross settlement amount and subtract the total procurement cost to determine Medicare's final lien demand.
What is a Medicare release?
General. A “consent to release” document is used by an individual or entity who does not represent the Medicare beneficiary but is requesting information regarding the beneficiary's conditional payment information.
How long does Medicare have to recoup payments?
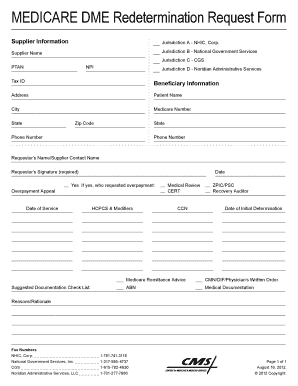
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
How do I get Medicare reimbursement?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is a Medicare overpayment?
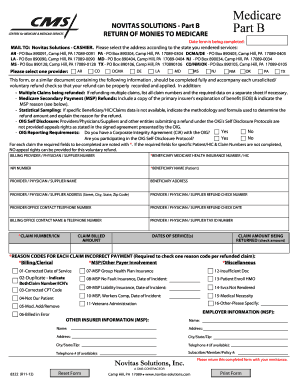
A Medicare overpayment is a payment that exceeds regulation and statute properly payable amounts. When Medicare identifies an overpayment, the amount becomes a debt you owe the Federal government. Federal law requires the Centers for Medicare & Medicaid Services (CMS) to recover all identified overpayments.
CMS Conditional Payment Information | Guidance Portal
Under Medicare Secondary Payer law (42 U.S.C. § 1395y(b)), Medicare does not pay for items or services to the extent that payment has been, or may reasonably be expected to be, made through a no-fault or liability insurer or through a workers' compensation entity. Medicare may make a conditional payment when there is evidence that the primary plan does not pay promptly conditioned upon ...
Conditional Payments - CMS
Conditional Payments January 10, 2021. Page 4 of 27 . Slide 4 - of 26 - Case Recovery
Conditional Payment Letters and Conditional Payment Notices
• An initial Conditional Payment Letter (CPL) does NOT need to be requested. A CPL will be generated automatically within 65 days of the issuance of the "Rights and Responsibilities
Request a Mailed Copy of the Conditional Payment Letter
For BCRC cases, when you select the Request a mailed copy of the conditional payment letter action, the MSPRP will send the conditional payment letter to each authorized individual/entity associated to the case (i.e., the beneficiary and each individual/entity with a Verified Proof of Representation or Consent to Release on file for the case).
42 CFR Part 424 - CONDITIONS FOR MEDICARE PAYMENT | CFR | US Law | LII ...
Subpart A - General Provisions (§§ 424.1 - 424.7) Subpart B - Certification and Plan Requirements (§§ 424.10 - 424.27) Subpart C - Claims for Payment (§§ 424.30 - 424.44)
Medicare Secondary Payer (MSP): Condition, Occurrence, Value, and ...
February 12, 2013 – Revised 10.01.15. Medicare Secondary Payer (MSP): Condition, Occurrence, Value, and Patient Relationship, and Remarks Field Codes. This article includes tables of some of the most common Condition, Occurrence, Value, Patient Relationship, and Remarks Field Codes associated with MSP claims.
Initial Claim
Initial Claim Call medicare personal injury department at 1-800-999-1118 to open the initial claim.
Conditional Payment Letter
Conditional Payment Letter In 65 days you should receive a "conditional payment letter" which the insurance company will require in order to properly resolve your claim.
When will Medicare determine if a conditional payment is being claimed?
Once Medicare has information concerning a potential recovery situation, it will identify the conditional payments paid by Medicare that are being claimed and/or released with respect to the accident, illness, or other incident from the date of incident through the date of settlement, judgment, award, or other payment.
How long does it take to get a conditional payment letter?
Sixty-five days after the Rights and Responsibilities letter is sent, the Conditional Payment letter will be sent to all authorized parties on the case.
Why are conditional payments called conditional payments?
These payments are referred to as conditional payments because the money must be repaid to Medicare when a settlement, judgment, award, or other payment is secured.
What is the sum of the amounts included in the conditional payment amount column?
The sum of the amounts included in the conditional payment amount column is the Total Conditional Payments Amount.
What is a payment summary form?
The Payment Summary form lists all of the claims that are included in the Current Conditional Payment Amount.
Can a debtor submit a redetermination request on the MSPRP?
To automate the redetermination process, the debtor and their authorized representatives can submit a redetermination request (first level appeal) on the MSPRP for BCRC or CRC cases.
Can authorized users request an update to the conditional payment amount?
For CRC cases, authorized users may request an update to the conditional payment amount.
What is a CPL letter?
This letter identifies Medicare's current conditional payment amount (as noted in the Current Conditional Payment Amount on the Case Information page) The CPL will include a Payment Summary Form that lists claims paid by Medicare that are being claimed and/or released with respect to the accident, illness, injury, or other incident. For more information on the conditional payment amount see the Request an update to the conditional payment amount help page.
How to contact MSPRP for BCRC?
Phone: (855) 798-2627. For BCRC cases, when you select the Request a mailed copy of the conditional payment letter action, the MSPRP will send the conditional payment letter to each authorized individual/entity associated to the case (i.e., the beneficiary and each individual/entity with a Verified Proof of Representation or Consent ...
Can you request a copy of a CPL?
This option allows you to request a mailed copy of the Condition al Payment Letter (CPL) for either a Benefits Coordination & Recovery Center (BCRC) or Commercial Repayment Center (CRC) case.
Does a conditional payment letter update?
Note: The Request a mailed copy of the conditional payment letter action will not update the Current Conditional Payment Amount prior to the letter being generated. However, claims are retrieved daily, so the Conditional Payment Amount displayed on the Case Information page will be up to date as of the previous day.
How to get conditional payment information?
You can obtain the current conditional payment amount and copies of CPLs from the BCRC or from the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627. To obtain conditional payment information from the MSPRP, see the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below. If a settlement, judgment, award, or other payment occurs, it should be reported to the BCRC as soon as possible so the BCRC can identify any new, related claims that have been paid since the last time the CPL was issued.
How to remove CPL from Medicare?
If the beneficiary or his or her attorney or other representative believes any claims included on the CPL or CPN should be removed from Medicare's conditional payment amount , documentation supporting that position must be sent to the BCRC. The documentation provided should establish that the claims are not related to what was claimed or were released by the beneficiary. This process can be handled via mail, fax, or the MSPRP. See the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below for additional details. The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
What is a CPL for Medicare?
A CPL provides information on items or services that Medicare paid conditionally and the BCRC has identified as being related to the pending claim. For cases where Medicare is pursuing recovery from the beneficiary, a CPL is automatically sent to the beneficiary within 65 days of issuance of the Rights and Responsibilities letter (a copy of the Rights and Responsibilities letter can be obtained by clicking the Medicare's Recovery Process link). All entities that have a verified Proof of Representation or Consent to Release authorization on file with the BCRC for the case will receive a copy of the CPL. Please refer to the Proof of Representation and Consent to Release page for more information on these topics. The CPL includes a Payment Summary Form that lists all items or services the BCRC has identified as being related to the pending claim. The letter includes the interim total conditional payment amount and explains how to dispute any unrelated claims. The total conditional payment amount is considered interim as Medicare might make additional payments while the beneficiary’s claim is pending.
How long does it take to get a demand letter from a court?
If a response is received within 30 calendar days, the correspondence will be reviewed, and a demand letter will be issued. If a response is not received in 30 calendar days, a demand letter will automatically be issued requesting repayment on all conditional payments related to the case without a proportionate reduction for fees or costs.
Does Medicare pay for a secondary plan?
Under Medicare Secondary Payer law (42 U.S.C. § 1395y(b)), Medicare does not pay for items or services to the extent that payment has been, or may reasonably be expected to be, made through a no -fault or liability insurer or through a workers' compensation entity. Medicare may make a conditional payment when there is evidence that the primary plan does not pay promptly conditioned upon reimbursement when the primary plan does pay. The Benefits Coordination & Recovery Center (BCRC) is responsible for recovering conditional payments when there is a settlement, judgment, award, or other payment made to the Medicare beneficiary. When the BCRC has information concerning a potential recovery situation, it will identify the affected claims and begin recovery activities. Beneficiaries and their attorney(s) should recognize the obligation to reimburse Medicare during any settlement negotiations.
Can you get Medicare demand amount prior to settlement?
If the beneficiary is settling a liability case, he or she may be eligible to obtain Medicare's demand amount prior to settlement or to pay Medicare a flat percentage of the total settlement. Click the Demand Calculation Options link to determine if the beneficiary's case meets the required guidelines.
Does Medicare send recovery letters to beneficiaries?
The beneficiary does not need to take any action on this correspondence. However, if Medicare is pursuing recovery from the beneficiary, the BCRC will send recovery correspondence to the beneficiary.
How many days before the anticipated date of settlement for Medicare?
The process begins when the beneficiary, their attorney, or another representative (SLRS), provides the required notice of pending liability insurance settlement to the appropriate Medicare contractor at least one hundred twenty (120) days before the anticipated date of settlement.
Does Medicare use synergy?
Fortunately, Medicare has recently released a tool which is very useful in avoiding such situations. Synergy regularly utilizes this tool to achieve exceptional results in cases for clients which have enrolled in this process prior to settlement.
Can an insurer request an eCPL?
Insurers, recovery agents who were submitted on the insurers' Tax Identification Number (TIN) reference file, and insurer representatives with a verified Recovery Agent Authorization, who log in using multi-factor authentic ation, can also request an eCPL for insurer-debtor cases only.
Does a request for conditional payment update?
The Request an electronic conditional payment letter with Current Conditional Payment Amount action will not update the Current Conditional Payment Amount prior to the letter being generated. However, claims are retrieved daily, so the Conditional Payment Amount displayed on the Case Information page will be up to date as of the previous day.
Can you request an electronic conditional payment letter?
The ability to request an electronic conditional payment letter is available to beneficiaries for either BCRC or CRC cases. This option is also visible and active for authorized beneficiary representatives who have a POR signed by the beneficiary in verified status and who log in using multi-factor authentication. Insurers and their authorized representatives who have a verified Recovery Agent Authorization, who log in using multi-factor authentication, can also request an eCPL for insurer-debtor cases only.
Who can request an electronic version of a conditional payment letter?
The ability to request an electronic version of the conditional payment letter is only available to beneficiaries and authorized beneficiary representatives who have a verified POR signed by the beneficiary and who have logged into the MSPRP using multi-factor authentication.
How long does it take to get a conditional payment letter?
and have initiated the Final Conditional Payment process. You will be mailed an Updated Conditional Payment Letter within 7-12 business days. This letter will include a list of claims currently associated to your case,
How to request a copy of a Notice of Anticipated Settlement?
To request a mailed copy of the Notice of Anticipated Settlement Letter, select the Request a mailed copy of the conditional payment letter action on the Case Information page for the applicable Case ID and click [Continue].
How long does it take to dispute a CP claim?
Disputes submitted on the MSPRP for Final CP cases are addressed within 11 business days. To view/dispute claims, click View/Dispute Claims Listing on the Case Information page. Click [Continue]. Once this action is selected, the MSPRP retrieves all of the claim information that is included in the Current Conditional Payment Amount and displays that information on the Claims Listing page. See the Disputing a Claim- Beneficiary CBT for more information on disputing claims.
What is the final CP process?
All Final CP actions must be completed on the MSPRP. The Final CP process is only available for liability cases and workers’ compensation cases. This process can be initiated by the identified debtor, or their authorized representative. Note: When an insurer debtor initiates the Final CP process, this action closes the insurer case and transitions the debt to the beneficiary.
What happens if you have not requested the final CP amount?
current Final Conditional Payment Status is Active), you will receive a Notice of Anticipated Settlement Letter.
How long does it take to get a final CP?
3. Request your Final CP Amount within 120 calendar days from the date that you initiated the process. Note: You must settle your case within three (3) business days of requesting the Final CP Amount.
How to get conditional payment information?
You can obtain the current conditional payment amount and copies of CPLs from the BCRC or from the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627. To obtain conditional payment information from the MSPRP, see the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below. If a settlement, judgment, award, or other payment occurs, it should be reported to the BCRC as soon as possible so the BCRC can identify any new, related claims that have been paid since the last time the CPL was issued.
How to remove CPL from Medicare?
If the beneficiary or his or her attorney or other representative believes any claims included on the CPL or CPN should be removed from Medicare's conditional payment amount , documentation supporting that position must be sent to the BCRC. The documentation provided should establish that the claims are not related to what was claimed or were released by the beneficiary. This process can be handled via mail, fax, or the MSPRP. See the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below for additional details. The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
What does BCRC do with conditional payment?
The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
What is a CPL for Medicare?
A CPL provides information on items or services that Medicare paid conditionally and the BCRC has identified as being related to the pending claim. For cases where Medicare is pursuing recovery from the beneficiary, a CPL is automatically sent to the beneficiary within 65 days of issuance of the Rights and Responsibilities letter (a copy of the Rights and Responsibilities letter can be obtained by clicking the Medicare's Recovery Process link). All entities that have a verified Proof of Representation or Consent to Release authorization on file with the BCRC for the case will receive a copy of the CPL. Please refer to the Proof of Representation and Consent to Release page for more information on these topics. The CPL includes a Payment Summary Form that lists all items or services the BCRC has identified as being related to the pending claim. The letter includes the interim total conditional payment amount and explains how to dispute any unrelated claims. The total conditional payment amount is considered interim as Medicare might make additional payments while the beneficiary’s claim is pending.
How long does a CPN take to respond to a judgment?
After the CPN has been issued, the recipient is allowed 30 days to respond.
When should a CPL be reported to the BCRC?
If a settlement, judgment, award, or other payment occurs, it should be reported to the BCRC as soon as possible so the BCRC can identify any new, related claims that have been paid since the last time the CPL was issued. For more information about the CPL, refer to the document titled Conditional Payment Letters (Beneficiary).
How long does it take to get a demand letter from a court?
If a response is received within 30 calendar days, the correspondence will be reviewed, and a demand letter will be issued. If a response is not received in 30 calendar days, a demand letter will automatically be issued requesting repayment on all conditional payments related to the case without a proportionate reduction for fees or costs.