The supplier of the orthotic must be enrolled in Medicare and accept Medicare assignment. Individuals enrolled in Medicare Part B who are eligible for an orthotic device will pay 20 percent of the Medicare-approved cost, and the Part B deductible will apply.
Full Answer
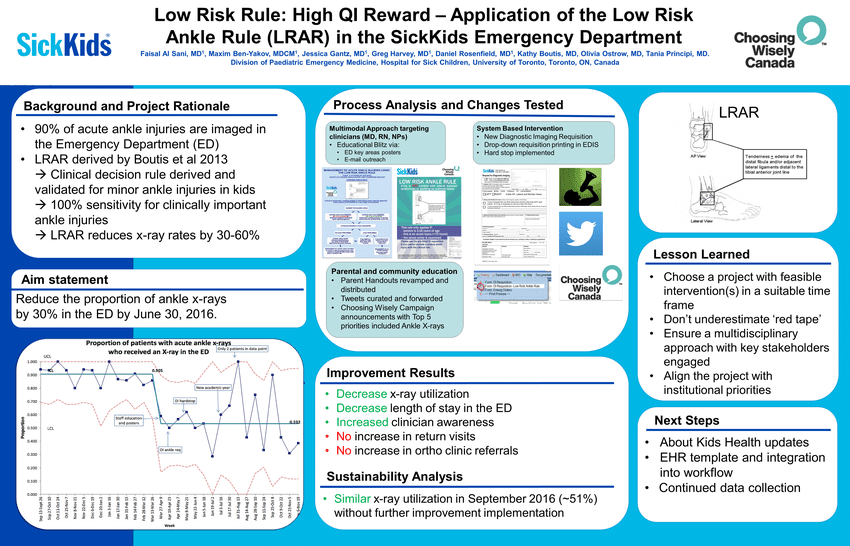
Does Medicare cover ankle braces?
Yes, Medicare will help cover the costs of ankle braces. Beneficiaries pay only 20% of the cost for ankle braces with Part B. Benefits may include ankle braces, straps, guards, stays, stabilizers, and even heel cushions. Acute and chronic ankle or foot pain is a common, everyday use for these devices.
Does Medicare cover orthopedic shoes?
Medicare covers orthopedic shoes if they’re a necessary part of a leg brace. You pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare will only cover these items if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
How much does Medicare pay for orthotics?
Medicare assignment. Individuals enrolled in Medicare Part B who are eligible for an orthotic device will pay 20 percent of the Medicare-approved cost, and the Part B deductible will apply. In 2019, the yearly Part B deductible is $185.00.
Does Medicare cover wheelchairs and walkers?
Medicare Part B (Medical Insurance) covers power-operated vehicles (scooters), walkers, and wheelchairs as durable medical equipment (DME). Medicare helps cover DME if: • The doctor treating your condition submits a written order stating that you have a medical need for a wheelchair or scooter for use in your home.

Are artificial limbs covered by Medicare?
Yes, Medicare will cover a prosthetic leg. Part B will cover the cost of the surgery if it's done in an outpatient setting. If it's done in an inpatient setting, then Part A will cover it. You must get your prosthetic leg from a supplier that participates in Medicare.
Are foot orthotics covered by Medicare?
Does Medicare Cover Orthotics? Orthotics are devices used to treat injured muscles and joints. Medicare will typically cover 80 percent of the costs for orthotic devices under Medicare Part B if they are deemed medically necessary by a doctor.
How do you qualify for a prosthetic leg?
You have difficulty walking without assistance. You need crutches, a cane, a wheelchair, or another assistive device to walk. You have difficulty managing public transportation on your own or driving. You face other limitations because of your amputation, despite your use of a prosthetic limb.
Does Medicare pay for podiatry?
Medicare Part B covers podiatry services for medically necessary treatment of foot injuries, diseases, or other medical conditions affecting the foot, ankle, or lower leg.
Does Medicare Part B cover custom orthotics?
Medicare Part B pays for 80 percent of the approved cost of either custom-made or pre-made orthotic devices. Of course, this is only possible if your health care provider feels it is medically necessary. Medicare categorizes orthotics under the durable medical equipment (DME) benefit.
Why are orthotics not covered by insurance?
Accommodative, digital, or supportive orthotics are flexible or semi-rigid devices and are used to ease foot pain. Since they do not correct the condition, they are considered comfort and convenience items and are excluded from coverage.
How can I get a free prosthetic leg?
Amputee Blade Runners is a nonprofit organization that helps provide free running prosthetics for amputees. Running prosthetics are not covered by insurance and are considered “not medically necessary,” so this organization helps amputees keep an active lifestyle.
What is the average cost of a prosthetic leg?
The cost for a prosthetic leg is usually less than $10,000 for a basic leg and upwards of $70,000 or more for a computerized leg that you control via muscle movement. That cost is just for one leg, so if you want another one to use for other purposes, you will likely need to pay for the additional prosthetic.
Can you wear a prosthetic leg all day?
Overdoing it and not following the schedule and instructions from your prosthetist can result in pain and possible injury. Once you have completed the wearing schedule, you can wear the prosthesis all day, but never at night while sleeping. Will I need a wheelchair or crutches?
What does Medicare considered routine foot care?
Routine foot care includes: Cutting or removing corns and calluses. Trimming, cutting, or clipping nails. Hygienic or other preventive maintenance, like cleaning and soaking your feet.
Does Medicare pay for podiatrist to cut toenails?
NonCovered Foot Care The cutting of toenails in a healthy person or when they are not painful is not a payable service by Medicare. The cutting of corns and calluses in a healthy person is not a payable service by Medicare. Legally, your podiatrist cannot try to obtain Medicare payment for noncovered foot care.
Do podiatrists cut toenails?
While you may be able to care for your toenails at home, you can also schedule a visit with the podiatrists at Certified Foot and Ankle Specialists to trim your toenails properly. It is during this visit that many overlooked preventive measures are performed.
What are the orthotics for DME?
Medicare lists the following devices as orthotics under the heading of DME: Bracing for ankle, foot, knee, back, neck, spine, hand, wrist, elbow. Orthopedic shoes as a necessary part of a leg brace. Prosthetic devices like artificial limbs. Medicare recipients must meet all the following prerequisites for eligibility:
What is the Medicare Part B deductible?
In 2019, the yearly Part B deductible is $185.00.
Does Medicare cover orthotics?
Medicare Coverage for Orthotic Devices. Medicare Part B pays for 80 percent of the approved cost of either custom-made or pre-made orthotic devices. Of course, this is only possible if your health care provider feels it is medically necessary.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
ICD-10-CM Codes that Support Medical Necessity
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the LCD section on “ Coverage Indications, Limitations, and/or Medical Necessity ” for other coverage criteria and payment information.
ICD-10-CM Codes that DO NOT Support Medical Necessity
For the specific HCPCS codes indicated above, all ICD-10 codes that are not specified in the preceding section. For all other HCPCS codes, diagnoses are not specified.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
Does Medicare cover prescriptions?
applies. Medicare will only cover these items if your doctors and suppliers are enrolled in Medicare.
Can a doctor be enrolled in Medicare?
Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers if they participate in Medicare before you get these items.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare cover therapeutic shoes?
Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers ...
Does Medicare cover custom molded shoes?
One pair of custom-molded shoes and inserts. One pair of extra-depth shoes. Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes. 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts.
Do suppliers have to accept assignment for therapeutic shoes?
It's also important to ask your suppliers if they participate in Medicare before you get therapeutic shoes. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren't "participating," they may choose not to accept assignment.
When is L5856 required?
Additionally, prior authorization will be required for certain Lower Limb Prosthetics (L5856, L5857, L5858, L5973, L5980, and L5987), with dates of service on or after September 1, 2020 in California, Michigan, Pennsylvania, and Texas. On December 1, 2020, prior authorization for these codes will be required in all of the remaining states ...
When is the CMS call for pressure reducing support surfaces?
CMS will host a call to discuss the addition of pressure reducing support surfaces to the Required Prior Authorization List on Tuesday, June 4, 2019 from 2:00 p.m. to 3:30 p.m. Eastern Time (ET). For more information, please visit the Special Open Door Forums webpage.
How long does it take to get a prior authorization?
Please note that all initial prior authorization decisions should be made in no more than 10 days. In cases where that timeframe could seriously jeopardize the life or health of the beneficiary, you may request an expedited review. Decisions for substantiated expedited reviews should be made within 2 business days.
When will LLPs be approved?
Prior Authorization for LLPs will be implemented in two phases. Phase one will begin May 11, 2020 in one state from each DME MAC jurisdiction: California, Michigan, Pennsylvania, and Texas. Phase two will begin October 8, 2020 and expands prior authorization of these codes to all of the remaining states and territories.
How to know how much to pay for surgery?
For surgeries or procedures, it's hard to know the exact costs in advance. This is because you won’t know what services you need until you meet with your provider. If you need surgery or a procedure, you may be able to estimate how much you'll have to pay. You can: 1 Ask the doctor, hospital, or facility how much you'll have to pay for the surgery and any care afterward. 2 If you're an outpatient, you may have a choice between an ambulatory surgical center and a hospital outpatient department. 3 Find out if you're an inpatient or outpatient because what you pay may be different. 4 Check with any other insurance you may have to see what it will pay. If you belong to a Medicare health plan, contact your plan for more information. Other insurance might include:#N#Coverage from your or your spouse's employer#N#Medicaid#N#Medicare Supplement Insurance (Medigap) policy 5 Log into (or create) your secure Medicare account, or look at your last "Medicare Summary Notice" (MSN)" to see if you've met your deductibles.#N#Check your Part A#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#if you expect to be admitted to the hospital.#N#Check your Part B deductible for a doctor's visit and other outpatient care.#N#You'll need to pay the deductible amounts before Medicare will start to pay. After Medicare starts to pay, you may have copayments for the care you get.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. if you expect to be admitted to the hospital. Check your Part B deductible for a doctor's visit and other outpatient care.
Can you know what you need in advance with Medicare?
Your costs in Original Medicare. For surgeries or procedures, it's hard to know the exact costs in advance. This is because you won’t know what services you need until you meet with your provider. If you need surgery or a procedure, you may be able to estimate how much you'll have to pay. You can:
Does Medicare cover medical care?
Medicare’s general rule is that it will provide coverage for medical care and treatment if services are deemed medically necessary by a Medicare-approved physician. In order for something to qualify as a medical necessity, Medicare tends to require that it be ordered by a licensed medical professional.
Does Medicare cover eyelid surgery?
Original Medicare benefits do not cover the cost of cosmetic surgical procedures, meaning Medicare recipients will have to pay for eyelid surgery on their own if the reason for wanting the procedure is to improve appearance.
What is Medicare approved braces?
Medicare Approved Braces and Devices. Medicare approves braces and devices when medically necessary to treat or maintain a medical condition. Orthotic devices like braces are otherwise known as Durable Medical Equipment. Braces may be used to support the knee, neck, arm, or back. Combining the use of orthotic devices with other treatments may delay ...
What is durable medical equipment?
The Durable Medical Equipment must be a functional and rehabilitative device for coverage to apply . Knee orthotics must also aid a patient’s healing process of joint or neighboring tissue after an injury or surgery. Functional – A pre-injured knee may be the result of a fall, sporting injury, or trauma to the area.
Does Medicare pay for cervical collars?
Currently, Medicare doesn’t pay for these devices. Cervical collars may be either soft or hard. Soft collars are more comfortable; typically, these braces are made of foam, felt, or rubber. Hard neck supports may keep the head and neck completely still. After invasive surgery or severe neck injury, your doctor may prescribe hard neck support.
Does Medicare require a prescription for a medical device?
However, in some situations, Medicare may require prior authorization before paying for Durable Medical Equipment. Every injection comes with a specific cost. Talk to your plan directly to determine the allowable amount for a procedure or injection.
Does Medicare cover ankle braces?
Yes, Medicare will help cover the costs of ankle braces. Beneficiaries pay only 20% of the cost for ankle braces with Part B. Benefits may include ankle braces, straps, guards, stays, stabilizers, and even heel cushions. Acute and chronic ankle or foot pain is a common, everyday use for these devices.
Is back braces covered by Medicare?
When a medical condition requires it, all back braces are under Medica re coverage. Coverage for back braces and supports include lumbosacral orthoses. The purpose of a lumbosacral orthosis is to support the muscular and bony aspects of the spine. Medicare-approved back braces such as lumbosacral orthotics may provide extra stability ...