To qualify for home health services for in-home caregiving, you generally must:
- Have Medicare Part A and Part B
- Be under the care of a doctor and getting services under a plan of care regularly reviewed by a doctor
- Have a doctor certify that you need intermittent skilled nursing care or physical therapy, speech-language pathology or continued occupational services
- Receive care from a home health agency that is Medicare-certified
Full Answer
How much does Medicare pay for in home care?
In order to qualify for benefits, the following five requirements must be met, according to the Medicare Learning Network’s (MLN) pamphlet, “Medicare & Home Health Care.” 1. You’re under the care of a doctor, and you’re getting services under a plan of care established and reviewed regularly by a doctor. 2.
Does Medicare or Medicaid pay for home care?
Jan 06, 2022 · The primary step in getting approved for in-home care is that you and the nursing plan must be under the care of a Medicare-approved doctor. This doesn’t mean that the doctor will be at every visit. A home health nurse specialist will administer your plan, which your will “create and regularly review.”.
Does Medicare usually cover in home care?
Jun 20, 2019 · Instead of getting Part A and Part B through the federal government directly, you get them through a private insurance company that contracts with Medicare. So, your in-home health care benefits will be at least the same as what Medicare Part A and Part B offer (except for hospice care, which comes directly from Part A).
How long does Medicare pay for home health care?
Jul 12, 2021 · For Medicare to provide in-home care, you’ll generally need a medical professional to certify to the fact that your husband needs skilled nursing care or therapy related to a specific condition, surgery, or illness. But your husband may be eligible for certain durable medical equipment that lend to his mobility.

What Is Home Health Care?
Home health care can involve a wide range of services you may need when you’re ill or recovering from an illness or surgery. In some cases it can i...
In-Home Care: Medical and Non-Medical
Depending on what is available in your community, home care can include: 1. Health care – skilled nursing care; physical, speech, occupational and...
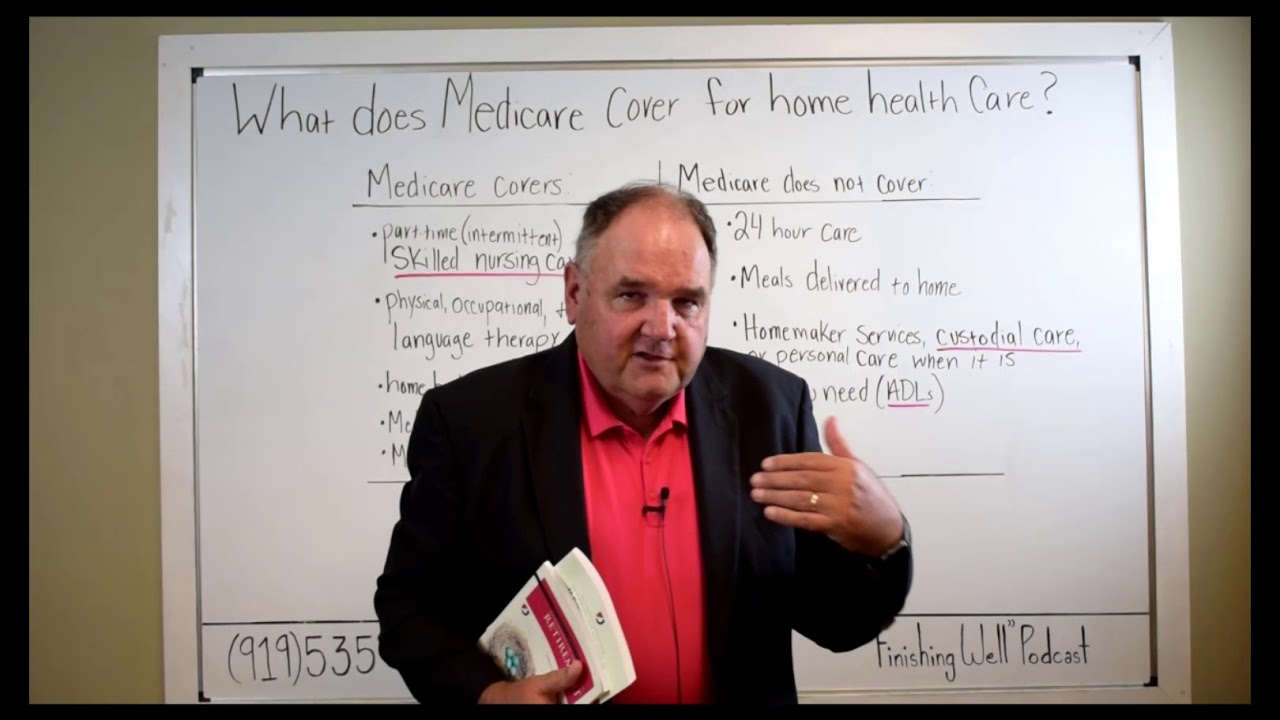
Does Medicare Cover Home Health Care?
Medicare Part A and/or Part B may help pay for your home health care if these conditions apply to you: 1. You’re under the care of a doctor who acc...
Home Health Care and Medicare Supplement Insurance
You might have to pay a coinsurance amount in some cases; for example, under Medicare Part B, you usually pay 20% of durable medical equipment cost...
Not All Home Health Care Agencies Are Created Equal
Home health agencies vary in the services they offer, and not every agency is certified by Medicare. You may want to match your needs with the serv...
Will Medicare cover skilled nursing care?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily...
Will Medicare cover physical, occupational, and speech therapy?
Medicare will pay for physical therapy when it’s required to help patients regain movement or strength following an injury or illness. Similarly, i...
Does Medicare cover durable medical equipment?
Medicare will cover the cost of medically necessary equipment prescribed by a doctor for in-home use. This includes items such as canes or walkers,...
Does Medicare cover medical social services?
Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may inc...
Who’s eligible for in-home care through Medicare?
Medicare enrollees are eligible for in-home care under Medicare Parts A and B provided the following conditions are met: The patient is under the c...
Will Medicaid pay for long-term care services?
Many Medicare enrollees are qualify for Medicaid due to their limited incomes and assets. Unlike Medicare, Medicaid covers both nursing home care a...
What does it mean to be homebound?
To be homebound means: You have trouble leaving your home without help (such as a cane, wheelchair, walker, crutches, special transportation or help from another person) because of an illness or injury, or leaving your home isn’t recommended because of your condition. 5. As part of your certification of eligibility, a doctor, ...
What is the definition of a doctor?
1. You’re under the care of a doctor, and you’re getting services under a plan of care established and reviewed regularly by a doctor. 2. You need, and a doctor certifies that you need, one or more of these: Intermittent skilled nursing care (other than drawing blood) Physical therapy.
Do you need a therapist for your aging parents?
You are doing everything you can for your aging parents, but sometimes it comes to the point where that is not enough. After a hospitalization, or to simply maintain or slow the decline of their health, Mom or Dad may need skilled therapists and nurses. This new twist in caring for Mom and Dad raises many questions.
Do parents have rights to health care?
You also may be comforted by the fact that your parents have rights as far as their health care is concerned. These include having their property treated with respect; to be told, in advance what care they’ll be getting and when their plan of care is going to change; to participate in their care planning and treatment.
Do you have to have a face to face encounter with a doctor?
As part of your certification of eligibility, a doctor, or other health care professional that works with a doctor, must document that they’ve had a face-to-face encounter with you within required time frames and that the encounter was related to the reason you need home health care.
Does Medicare cover home aides?
Medicare also covers continuous health care but on a different level. It only covers a percentage of the cost. Unfortunately, home aides that help with housework, bathing, dressing and meal preparations are not covered by Medicare.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
What is home health aide?
Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom. Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
Do you have to be Medicare approved to be homebound?
The in-home health agency must be Medicare-approved. Your doctor must certify that you’re unable to leave your home without some difficulty – for example, you might need transportation and/or help from a cane, a walker, a wheelchair, and/or someone to help you. In other words, you’re homebound.
Do you have to pay coinsurance for osteoporosis?
Medical supplies. Injectable osteoporosis drugs. If you qualify for home health care under Medicare, you generally don’t have to pay any coinsurance or copayment. If you need durable medical equipment, you’ll typically pay 20% of the Medicare-approved amount as coinsurance.
Does Medicare cover in-home care?
When might Medicare cover in-home health care? In general, Medicare doesn’t cover long- term home health care. Here’s how Medicare coverage of in-home health care typically works. In most cases, even when Medicare covers in-home health care, it’s for part-time care, and for a limited time.
Does Medicare Advantage have a deductible?
Medicare Advantage plans may have annual deductibles, and may charge coinsurance or copayments for these services. Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending.
How many hours does Medicare pay for a week?
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it won’t cover 24-hour-a-day care.
How long does Medicare pay for custodial care?
Medicare will sometimes pay for short-term custodial care (100 days or less) if it’s needed in conjunction with actual in-home medical care prescribed by a doctor.
What is a long term care policy?
A long-term care policy can help defray the cost of home health aides whose services are strictly custodial in nature. It can also help pay for assisted living facilities, which offer seniors the ability to live independently, albeit with help.
How long does Medicare pay for intermittent nursing?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
What is skilled nursing?
Skilled nursing services are generally required to treat an illness or assist in the recovery of an injury. As the name implies, those who provide this care are licensed to administer medical treatment such as injections, catheter changes, wound dressings, and tube feedings.
Does Medicare cover social services?
Does Medicare cover medical social services? Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may include in-home counseling from a licensed therapist or social worker.
Does Medicaid have a higher income limit?
Due to the high cost of long-term care, many states have higher Medicaid income limits for long-term care benefits than for other Medicaid coverage. However, Medicaid’s asset limits usually require you to “spend-down” resources before becoming eligible.
What do you need to qualify for home health care?
To qualify for home health services for in-home caregiving, you generally must: Have Medicare Part A and Part B. Be under the care of a doctor and getting services under a plan of care regularly reviewed by a doctor. Have a doctor certify that you need intermittent skilled nursing care or physical therapy, speech-language pathology ...
How many hours of care do you need to be in a skilled nursing facility?
If you need more than intermittent skilled nursing care (less than 7 days a week and less than 8 hours a day you generally are not eligible for a the home health benefit and must receive care in a skilled nursing facility. You might have to pay for in-home caregiving on your own in this situation.
What does dementia mean?
The Alzheimer’s association (ALZ) defines dementia as a decline in mental ability severe enough to interfere with daily life. According to ALZ, 60% of people with dementia will wander, not remembering his name or address and becoming disoriented in familiar places. If you’re a loved one of someone with dementia who wanders, you may feel that they need 24-hour supervision by an in-home caregiver. Unfortunately Medicare doesn’t generally cover 24-hour care at home. To cover in-home caregivers you may want to consider long-term care insurance, available from private insurance companies.
Does Medicare cover skilled nursing?
Medicare also may cover intermittent skilled nursing care at home. If you need in-home caregiving, Medicare Part A and Part B may also cover other home health services such as: To qualify for home health services for in-home caregiving, you generally must:
Does Medicare cover meals delivered to your home?
Medicare generally doesn’t cover meals delivered to your home. You might want to look into the Meals on Wheels program, which delivers free meals to older people in many communities. Especially if you’ve had a stroke and resulting paralysis, some personal care may also be difficult to do alone such as: Dressing.
Do you need skilled nursing after a heart attack?
Some people may want to be home after undergoing surgery or experiencing a health event such as a heart attack or stroke. They may need skilled nursing care. Skilled nursing care could include: Medicare Part A generally covers skilled nursing care in a skilled nursing facility under certain conditions for a limited time.
Does Medicare cover homemaker services?
Washing dishes/putting dishes in the dishwasher. Doing laundry. Medicare generally doesn’t cover “homemaker services” such as shopping, cleaning, and laundry when this is the only care you need and when the services aren’t related to a plan of care.
1. Medicare
If prescribed by a physician, Medicare will pay for a small amount of home care delivered by a Medicare Home Health Agency. The services you’ll receive are based on the specific medical condition and are usually only provided for a set period of time.
2. Private Pay (Out of Pocket)
The majority of families pay out of pocket for in-home care. Possible sources for private pay funds include:
3. Long-term Care Insurance
Long-term care insurance (LTCi) can pay for in-home assistance with “activities of daily living,” which include bathing, dressing, toileting, eating, and transferring from bed to chair or chair to chair. LTCi will also typically pay for things like meal preparation, medication reminders, light housekeeping, transportation, and more.
4. Private Health Insurance
Private health insurance offers very few benefits for in-home care. Some health insurance policies will cover some doctor-prescribed in-home care for acute health issues, usually following an in-hospital or skilled nursing facility stay. No health insurance policies or Medigap policies to supplement Medicare cover in-home long-term care.
5. Medicaid
Medicaid will cover short-term home care for acute conditions, typically after a hospital stay, skilled nursing facility stay, or physical rehabilitation. Medicaid will also only pay for home care provided by a Medicaid-certified home care agency.
6. Veterans Benefits
If your loved one served in the armed forces more than 90 days of active duty, with at least one day during a wartime period, and was honorably discharged, they may be eligible for benefits, including in-home care. Eligibility is calculated using a complex rating system based on how disabled your loved one is.
Let Help at Home Help
Help at Home has been helping families understand their options to pay for home care for over 20 years, and we’d love to help you. We serve the Chevy Chase, MD, Virginia, and Washington, DC metropolitan areas, and our mission is to provide the most compassionate senior home care possible.
What are the different ways to pay for home health care?
Consumers use different ways to pay for home health care services, including out-of-pocket, health insurance policies, long-term care policies, Medicare, and Medicaid. Some low-income families get help from volunteer programs.
What is home health aide?
Home care offers the elderly, seniors, people with disabilities, and family members the trained assistance to help with personal and medical care. But it limits specific tasks. Whether you hire a home health aide through an agency or privately, understand each person's role. Know what each person can and cannot do.
What is LTC insurance?
LTC is a privately paid insurance plan that covers long-term care needs like personal care . Most LTC policies pay segments of assisted living or nursing home care. Some pay for services in the community, such as home care and adult day services. Care's limited, based on the plan.
What is the number to call for home care for veterans?
Call 877-222-8387 toll-free to determine eligibility for these services. Find More at CHAMPVA and TRICARE.
Why is home care so difficult?
Paying for home care is challenging for families because most elders and adult children pay out-of-pocket. It's an abrasive reality for working families, yet home care is the only way to keep an older loved one out of a nursing home.
How long does it take to get long term care benefits?
Review the policy for details to learn when benefits kick in for collecting. Usually, it's anywhere from 30 to 120 days.
What is the number to call for eldercare?
Administration on Aging connecting you to services for older adults and their families. Call 1-800-677-1116.
Will Medicare cover family caregivers?
If you develop a medical condition that requires frequent or constant at-home healthcare, this can be time consuming and expensive. Often, the responsibility of becoming a caregiver for a mother, father, or parent can fall to an adult child, leaving many to wonder “does Medicare pay for family caregivers?”
When will Medicare pay for a caregiver?
For the most part, whether Medicare will cover in-home caregivers depends on exactly what type of care one is receiving. Keep in mind that to remain eligible for Medicare at-home medical care coverage, you will need to see your doctor fewer than 90 days before, or 30 days after, you begin to receive home healthcare services.
What are some other professional caregiver services that may be covered under Medicare?
Medicare does not typically cover caregivers who are solely responsible for custodial care needs, such as dressing, personal hygiene, restroom assistance, meal prep and delivery, and daily living, unless these services are provided short-term and by professionals approved by Medicare.