How many dialysis sessions does Medicare cover?
In further detail, Medicare will cover up to 15 dialysis training sessions for peritoneal dialysis and pay for up to 25 dialysis sessions for hemodialysis. Does Part A Cover Dialysis? Part A will cover dialysis treatments at an approved center.
Can I get Medicare when I start dialysis?
But, you can get Medicare on the first day of the month you start dialysis if you start a home training program. (NOTE: You must start to train for a home treatment before your third full month of dialysis.)
Does Medicare Part B cover dialysis transportation?
Often, Medicare Advantage plans will cover transportation services too. In addition to your actual dialysis treatment, Part B will cover all other services. Durable Medical Equipment, all lab tests, and transportation can fall under Part B benefits. You still have coverage if traveling in the United States.
How do I talk to an insurance agent about dialysis?
Call the eHealth helpline for dialysis patients at 1-844-980-2102 (TTY 711) to speak to a licensed insurance agent. Agents are available 24/7 from October 15 to December 7. The rest of the year, agents are available Monday-Friday from 8 a.m. to 9 p.m. (ET).
Can a person be denied dialysis?
Circumstances where the physician must treat are: emergency situations, patient characteristics (not on the basis of race, color, religion, national origin, sexual orientation or other discrimination, infectious diseases), and pre-existing contracts. There are justifiable reasons to refuse to treat.
Does dialysis make you eligible for Medicare?
You can get Medicare no matter how old you are if your kidneys no longer work, you need regular dialysis or have had a kidney transplant, and one of these applies to you: You've worked the required amount of time under Social Security, the Railroad Retirement Board (RRB), or as a government employee.
What is Part A and B in dialysis?
Inpatient dialysis treatments: Medicare Part A (Hospital Insurance) covers dialysis if you're admitted to a hospital for special care. Outpatient dialysis treatments & doctors' services: Medicare Part B (Medical Insurance) covers many services you get in a Medicare-certified dialysis facility or your home.
What is QIP dialysis?
What is the ESRD QIP? The Centers for Medicare & Medicaid Services (CMS) administers the End-Stage Renal Disease Quality Incentive Program (ESRD QIP) to promote high-quality services in renal dialysis facilities.
How many months after dialysis does Medicare Start?
If you're on dialysis: Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. This 4-month waiting period will start even if you haven't signed up for Medicare.
Can kidneys start working again after dialysis?
Acute kidney failure requires immediate treatment. The good news is that acute kidney failure can often be reversed. The kidneys usually start working again within several weeks to months after the underlying cause has been treated. Dialysis is needed until then.
What are the 3 types of dialysis?
There are 3 main types of dialysis: in-center hemodialysis, home hemodialysis, and peritoneal dialysis. Each type has pros and cons. It's important to remember that even once you choose a type of dialysis, you always have the option to change, so you don't have to feel "locked in" to any one type of dialysis.
Why does dialysis take 4 hours?
Four hours enable adequate delivery of dialysis through the removal of toxins. More important, together with a sensible dietary sodium intake, 4 hours of dialysis allow an adequate time over which excess fluid volume can be removed without provoking uncomfortable dialysis symptoms.
At what creatinine level should dialysis start?
National Kidney Foundation guidelines recommend you start dialysis when your kidney function drops to 15% or less — or if you have severe symptoms caused by your kidney disease, such as: shortness of breath, fatigue, muscle cramps, nausea or vomiting.
What is quality incentive program?
The Quality Incentive Program (QIP) represents a new pay for-performance program for California's public health care systems that converts funding from previously-existing supplemental payments into a value-based structure, meeting the Managed Care Rule's option that allows payments tied to performance.
What medications are included in the ESRD bundle?
WHAT IS INCLUDED IN THE ESRD BUNDLE? Beginning in 2011, the current bundle includes your dialysis treatments, dialysis labs and injectable medications received during treatment like EPO, iron, and vitamin D.
What does CMS stand for?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
When does Medicare start ESRD?
When you enroll in Medicare based on ESRD and you’re on dialysis, Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. For example, if you start dialysis on July 1, your coverage will begin on October 1.
When does Medicare start covering kidney transplants?
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
How to replace blood?
You can replace the blood by donating it yourself or getting another person or organization to donate the blood for you. The blood that’s donated doesn’t have to match your blood type. If you decide to donate the blood yourself, check with your doctor first.
How much is Part B insurance?
Most people must pay a monthly premium for Part B. The standard Part B premium for 2020 is $144.60 per month, although it may be higher based on your income. Premium rates can change yearly.
What is assignment in Medicare?
Assignment—An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare cover home dialysis?
Medicare Part B covers training for home dialysis, but only by a facility certifed for dialysis training. You may qualify for training if you think you would benefit from home dialysis treatments, and your doctor approves. Training sessions occur at the same time you get dialysis treatment and are limited to a maximum number of sessions.
Does Medicare cover dialysis for children?
Your child can also be covered if you, your spouse, or your child gets Social Security or RRB benefits, or is eligible to get those benefits.Medicare can help cover your child’s medical costs if your child needs regular dialysis because their kidneys no longer work, or if they had a kidney transplant.Use the information in this booklet to help answer your questions, or visit Medicare.gov/manage-your-health/i-have-end-stage-renal-disease-esrd/children-end-stage-renal-disease-esrd. To enroll your child in Medicare, or to get more information about eligibility, call or visit your local Social Security oce. You can call Social Security at 1-800-772-1213 to make an appointment. TTY users can call 1-800-325-0778.
When does Medicare start covering dialysis?
Medicare coverage will take effect depending on the route of treatment. If you’re a Hemodialysis patient, coverage will start in your 4th month of dialysis. When you’re a home dialysis patient, Medicare is active in the first month of treatment.
How many sessions does Medicare cover for peritoneal dialysis?
In further detail, Medicare will cover up to 15 dialysis training sessions for peritoneal dialysis and pay for up to 25 dialysis sessions for hemodialysis.
How much does hemodialysis cost?
Just one year of hemodialysis may cost you $72,000. And a single year of peritoneal dialysis can cost you around $53,000 each year. Keep in mind, Medicare will only cover 80%, you’ll be left with the remaining costs. Even with the majority of your treatment covered, you’ll still have costly bills.
Does Medicare cover medical equipment?
Medicare will cover a range of treatments, including tests, medications, and equipment. We know how important it is to understand your coverage. You need to know what isn’t covered just as much as you need to know what is covered. Below we’ll review how Medicare works with each treatment you may need. Then, you can make decisions ...
Can you get dialysis at home?
You can get dialysis in several different types of facilities. If you qualify, your dialysis can take place within the comforts of your own home. Or, you can also get dialysis at a certified dialysis center. For Medicare to cover your treatment, though, the center must be Medicare-certified.
Does Medicare cover ambulance transportation?
Your doctor will need to specify that transportation is medically necessary. Often, Medicare Advantage plans will cover transportation services too.
Does Medicare cover dialysis?
Yes, Medicare will cover you should you need dialysis treatments. Dialysis can come in many different forms. Below we’ll go over different types of dialysis treatments that have coverage.
When does Medicare start covering dialysis?
If you enroll in Medicare based on ESRD and you’re currently on dialysis, your Medicare coverage usually begins on the 1st day of your dialysis treatment’s 4th month. Coverage can start the 1st month if: During the first 3 months of dialysis, you participate in home dialysis training at a Medicare-certified facility.
How much does Medicare pay for home dialysis?
Once those premiums and deductibles are paid, Medicare typically pays 80 percent of the costs and you pay 20 percent . For home dialysis training services, Medicare typically pays a flat fee to your dialysis facility to supervise home dialysis training.
How long does it take for Medicare to resume?
Medicare coverage will resume if: within 12 months after the month , you stop getting dialysis, you start dialysis again or have a kidney transplant. within 36 months after the month you get a kidney transplant you get another kidney transplant or start dialysis.
How long does Medicare cover kidney transplants?
If you’re only eligible for Medicare due to permanent kidney failure, your coverage will stop: 12 months after the month dialysistreatments are stopped. 36 months following the month youhave a kidney transplant. Medicare coverage will resume if:
How long does Medicare retroactive coverage last?
If you’re eligible for Medicare based on ESRD but miss your initial enrollment period, you may be eligible for retroactive coverage of up to 12 months, once you’ve enrolled.
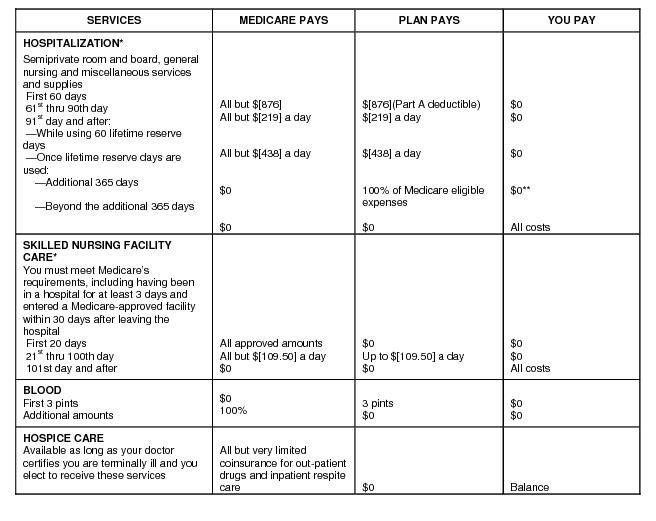
How much is Medicare Part A 2020?
The annual deductible for Medicare Part A is $1,408 (when admitted to a hospital) in 2020. This covers the first 60 days of hospital care in a benefit period. According to the U.S. Centers for Medicare & Medicare Services, about 99 percent of Medicare beneficiaries do not have a premium for Part A.
What services are covered by Medicare?
certain home support services: covered by Medicare Part B. most drugs for in-facility and at-home dialysis: covered by Medicare Part B. other services and supplies, such as laboratory tests: covered by Medicare Part B.
Who administers original Medicare?
Original Medicare is administered by the federal government and available to ESRD patients. It covers hospital services (Part A) and outpatient services (Part B). Individuals covered by Original Medicare can see any provider who accepts Original Medicare and is accepting new patients.
What is Medicare.gov?
Medicare.gov provides official benefit information on Medicare and Medicare Advantage. The Medicare Plan Finder tool shows you the plans available in your area. It also helps you compare plans and check if your doctors, dialysis facility and transplant center are in-network.
What is Medicare Plan Finder?
At Medicare.gov, the Medicare Plan Finder can help you compare pricing and benefits between Original Medicare, Medicare Advantage and other types of plans. It also can help you check if your doctors, dialysis facility and current or potential transplant center are in-network with Medicare Advantage plans you are considering.
What are the benefits of Medicare Advantage?
Medicare Advantage plans typically offer additional benefits Original Medicare doesn’t, such as vision, dental and hearing coverage. Other covered services could include transportation (such as to your dialysis center), meal delivery service and over-the-counter drugs.
How much does Medicare pay for outpatient therapy?
Individuals typically pay 20 percent of the Medicare-approved amount for most doctor services, outpatient therapy (including dialysis) and durable medical equipment. Original Medicare doesn’t have an annual out-of-pocket maximum, so there is no cap on the amount you may pay in a plan year.
Does Medicare Advantage pay monthly?
Many Medicare Advantage plans have low to no monthly premiums, which vary based on where you live, the plan and benefits offered . If you enroll in a Medicare Advantage plan, you’d still have a Medicare Part B premium, but the plan may pay part or all of that premium.
Does Medicare Advantage have a provider network?
Provider Network. With Original Medicare, you can see any provider that accepts Medicare, but Medicare Advantage plans have provider networks. Network providers are contracted with the insurance company to provide services at a certain rate. You'll want to check if your preferred providers are in the plan's network.
How much does Medicare pay for dialysis?
As a primary payer, Medicare Part B pays 80% of the Medicare allowed charge for dialysis. The other 20% can be paid by an EGHP or Medicaid (if you have it) or by a Medigap plan. Hospitals and doctors have 18 months to bill Medicare. Tell them if your Medicare is backdated.
How does Medicare work?
How Medicare works. Medicare Part A (hospital care) is free if you have enough credits. There is a premium if you don't have enough credits. As long as you're on dialysis or within 36 months of a transplant, you can work and keep Part A for free.
How long do you have to pay Medicare Part B premiums?
Why would you want to pay extra premiums for Medicare Part B if you have an EGHP? The law is that your EGHP must pay first for 30 months. The "clock" starts when you are eligible for Medicare—whether or not you take it.
How to pay less for dialysis?
There are steps you can take to pay less for care related to your dialysis: Ask your doctors if they accept Medicare assignment. All dialysis clinics do. Tell your doctor, clinic, and other healthcare providers what health coverage you have and always report any changes in coverage right away.
How many nights per week does Medicare pay for HD?
This fourth payment can make it possible for a center to offer you daily home HD or nocturnal home HD more than three nights per week.
Is Medicare 101 for dialysis?
Medicare 101 for People on Home Dialysis. Article by Beth Witten, MSW, ACSW, LSCSW. One good thing about kidney failure is having help from Medicare to pay for treatment. In 1973, Medicare was extended to those with permanent kidney failure who need dialysis or a transplant and who qualify for Social Security.
Can I apply for medicaid in California?
Apply for Medicaid (Medi-Cal in California) if you have limited income and assets. Ask the Medicaid caseworker if you qualify for a Medicare savings program to pay premiums, deductibles, and co-pays, and apply if you do. Ask your state insurance department if you can get a Medigap plan and apply for one.
What is dialysis for kidney disease?
Dialysis is a common procedure that can improve the health and well-being of some individuals diagnosed with kidney disease. These patients understand the importance of making it to their regular dialysis appointments.
Does Medicare cover transportation?
While Medicare coverage provides benefits for a wide range of care, services, and supplies, it does not cover the cost of transportation to or from medical appointments. The only exception to this is if a Medicare recipient requires transport by ambulance in the event of an emergency.
Does Medicare pay for transportation to appointments?
Although Medicare coverage may not pay for transportation to medical appointments, there are a number of free or low-cost alternatives that may be accessible depending on where you live. In many urban and suburban areas, dialysis centers themselves will offer transportation services to patients who are unable to get back and forth to appointments.
Can seniors drive themselves on dialysis?
Unfortunately, transportation can be a factor for some individuals who need to receive regular dialysis treatments, especially as they age. Many seniors find that they aren’t able to drive themselves, so they rely on family, friends, public transportation and ride sharing to get where they need to go.
Can you get transportation for dialysis?
In rural areas, dialysis patients may be able to receive transportation through county services. Many areas have specific care services available for seniors who can’t access transportation for medical appointments, and these are often available at no charge.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
When managing dialysis for patients with acute kidney injury, physicians may bill CPT ® codes 90935, 90937, 90945 or 90947 in Places of Service (POS) 11 (Office), 19 (Off Campus-Outpatient Hospital), 22 (On Campus-Outpatient Hospital), 23 (Emergency Room-Hospital), 31 (Skilled Nursing Facility), 65 (Free Standing Dialysis Facility) or 72 (Rural Health Clinic) with the diagnosis codes listed in the Covered ICD-10 Codes Section below..
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
