
You need to get the completed form from your employer and include it with your Application for Enrollment in Medicare (CMS-40B). Then you send both together to your local Social Security office. Find your local office here: www.ssa.gov.
What tax form shows proof of insurance?
To get the Medicare form you need, find the situation that applies to you. Get forms in alternate formats. I want to make sure Medicare can give my personal health information to someone other than me (Authorization to Disclose Personal Health Information form/CMS-10106). Fill out Authorization to Disclose Personal Health Information. This form is available both in English …
How do you show proof of health insurance?
Any way other than Original Medicare that you can get your Medicare health or drug coverage. This term includes all Medicare health plans and Medicare drug plans. , your plan will send you an "Evidence of Coverage" (EOC) each year, usually in the fall. The EOC gives you details about what the plan covers, how much you pay, and more.
How do I provide proof of insurance?
Ask your employer to fill out Section B. You need to get the completed form from your employer and include it with your Application for Enrollment in Medicare (CMS-40B). Then you send both together to your local Social Security office. Find your local office here: www.ssa.gov. GET HELP WITH THIS FORM. Phone: Call Social Security at 1-800-772-1213.
How to obtain proof of insurance?
Learn about the "Notice of Creditable Coverage," which your employer or union plan sends you to tell you about Medicare Savings Programs (MSPs) and the Extra Help available for Medicare prescription drug coverage.
How do I get a copy of my 1095-B form online?
How to find your 1095-A onlineLog in to your HealthCare.gov account.Under "Your Existing Applications," select your 2021 application — not your 2022 application.Select “Tax Forms” from the menu on the left.Download all 1095-As shown on the screen.
Does Medicare provide a 1095-A form?
It gives a breakdown of each month of the previous year, noting which months you had coverage, the cost of your premium, and any tax credit advance. Since this form applies only to insurance coverage purchased through the Marketplace, Medicare and Medicare Advantage programs do not provide a 1095-A form.
How do I get a 1095-B form?
How to find or request your Form 1095-BCall the number on your ID card or other member materials.Complete the 1095B Paper Request Form (pdf) and email it to your health plan at the email address listed on the form.
Do you get a 1095 C from Medicare?
If you were enrolled in Medicare: For the entire year, your insurance provider will not send a 1095 form. Retirees that are age 65 and older, and who are on Medicare, may receive instructions from Medicare about how to report their health insurance coverage.
How do I get a copy of my Medicare Form 1095-B?
Medicare. Call 1-800-MEDICARE (1-800-633-4227) to ask for a copy of your IRS Form 1095-B. TTY users can call 1-877-486-2048.
Is 1095 the same as 1095-B?
Form 1095-A, Health Insurance Marketplace Statement, is provided by the Marketplace to individuals who enrolled or who have enrolled a family member in health coverage through the Marketplace. Form 1095-B, Health Coverage, is provided by insurance companies and other coverage providers.Mar 22, 2022
Why did I get a 1095-B and not a 1095-A?
You need a 1095-A only if you bought health insurance through the Marketplace in 2021. If you did not buy that insurance, then you won't get a 1095-A.Jun 4, 2019
How do I know if I have a 1095-A form?
If you can't find your 1095-A, check online. If your form didn't come by mail or you can't find it, check your online Marketplace account.Mar 7, 2019
Do I need a 1095-B to file my taxes?
You do not need 1095-B form to file taxes. It is for your records. IRS 1095-B form is your proof of the month(s) during the prior year that you received qualifying health coverage.
Does Medicare send tax statements?
Medicare sends a tax statement to beneficiaries between December and January of each year. The document shows a person had Medicare Part A during the tax year. Medicare Part A and Medicare Advantage are classed as qualifying health coverage, under the Affordable Care Act.Aug 31, 2020
Do I need a 1095-C to file my taxes?
Do I need my Form 1095-C to file my taxes? No, you do not need to send a copy of your 1095-C to the IRS when filing your tax return. However, you should keep the form with your tax records.
How do I get proof of Medicare payments?
Frequently Asked Questions What can I use as proof of eligible Medicare premium expenses? The easiest receipt for you to use as proof of eligible expenses is the annual statement you receive from Social Security for the upcoming calendar year.
What is it?
If you're in a Medicare Plan Any way other than Original Medicare that you can get your Medicare health or drug coverage. This term includes all Medicare health plans and Medicare drug plans. , your plan will send you an "Evidence of Coverage" (EOC) each year, usually in the fall.
What should I do if I get this notice?
Review any changes to decide whether the plan will continue to meet your needs in the next year.
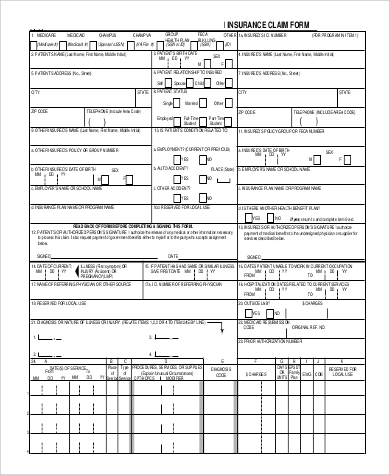
How to complete a health insurance form?
HOW IS THE FORM COMPLETED? Complete the first section of the form so that the employer can find and complete the information about your coverage and the employment of the person through which you have that health coverage. The employer fills in the information in the second section and signs at the bottom.
What to do if you get group health insurance through another person?
If you get group health plan coverage through another person, like a spouse or family member, write their Social Security Number. Once you complete Section A: Once Section A is completed, give this form to your employer to complete Section B.
How long do you have to be in a special enrollment period to get Medicare?
In order to apply for Medicare in a Special Enrollment Period, you must have or had group health plan coverage within the last 8 months through your or your spouse’s current employment. People with disabilities must have large group health plan coverage based on your, your spouse’s or a family member’s current employment.
What is section A in Medicare?
SECTION A: The person applying for Medicare completes all of Section A. Employer’s name: Write the name of your employer. Date: Write the date that you’re filling out the Request for Employment Information form . Employer’s address: Write your employer’s address. Applicant’s Name:
What is a group health plan?
A group health plan is any plan of one or more employers to provide health benefits or medical care (directly or otherwise) to current or former employees, the employer, or their families. If yes, give the date the coverage began. Write the month and year the date the applicant’s coverage began in your group health plan.
What is it?
You'll get this notice each year if you have drug coverage from an employer/union or other group health plan. This notice will let you know whether or not your drug coverage is “creditable.”
What should I do if I get this notice?
Keep the notice. You may need it if you decide to join a Medicare drug plan later. (Don't send creditable coverage letters/certificates to Medicare.)
What is it?
The Affordable Care Act requires people to have health coverage that meets certain standards (called qualifying health coverage or minimal essential coverage). The Qualifying Health Coverage (QHC) notice lets you know that your
What should I do if I get this notice?
Keep your Form 1095-B with your other important tax information, like your W-2 form and other tax records.
What is a 1095-B form?
The 1095-B form is a tax document with proof of your coverage and should be stored with any of your other tax documents for the previous year.
What is Medicare Advantage?
Original Medicare Part A and Medicare Advantage programs provide minimum essential coverage required by law as defined by the Affordable Care Act. The government provides a slightly different form to individuals with this coverage, which can include Medicare Part A, Medicare Advantage, Medicaid, CHIP, Tricare, and more.
What is a 1095A?
In short, the 1095-A form is the document provided to people who purchase their health insurance through the government-run healthcare Marketplace. The form includes basic personal information, such as your name, address, and insurance provider. It also lists anyone covered on the insurance policy, such as you, your spouse, and any children.
Does the 1095-B cover insurance?
Since the 1095-B form also covers certain employer-sponsored plans, it provides space for other people covered by the insurance plan . These extra spaces typically shouldn’t apply to you or be a source of concern.
Does Medicare provide a 1095-A?
Since this form applies only to insurance coverage purchased through the Marketplace, Medicare and Medicare Advantage programs do not provide a 1095-A form.
What is a 1095 form?
This is known as a 1095 form which provides details about the amount along with the period of time you received coverage. A 1095 form acts as proof of your health insurance and is useful to keep for your own personal records.
Who should receive a 1095-B?
Form 1095-B. Individuals and their families who do not receive a Form 1095-A or Form 1095-C should receive a Form 1095-B. This includes people who receive insurance from health care providers, government agencies and smaller employers who are not required to send the other types of forms. For example, you may receive a 1095-B if you bought health ...
Why are 1095s important?
During the first years of the Affordable Care Act (ACA), 1095 forms were more important as they would allow the IRS to verify health insurance coverage. If the IRS identified gaps in health coverage, then you would be required to pay the tax penalty for not having minimum essential coverage.
What is a 1095-A?
Form 1095-A. You would receive the Form 1095-A if you were enrolled in a marketplace health plan during the tax year. The form is a statement from the marketplace (either the HealthCare.gov federal marketplace or one of the state-run health care exchanges) acknowledging you were enrolled in medical insurance coverage, ...
How to reconcile 1095A?
To reconcile this information, check the 1095-A form: 1 If you used more credits than you were due, then you would owe additional tax on the difference between the two amounts. 2 If you used less than you were eligible for, then you would receive a tax refund on the difference.
When is the 1095-A deadline?
The deadline for the marketplace to provide you with a Form 1095-A is Jan. 31. The deadline for insurers, companies and government agencies to deliver forms 1095-B and 1095-C has been extended to March 4.
Is the 1095 tax form still valid for 2020?
In 2020, the tax penalty for lacking coverage is no longer in effect. But, as mentioned above, the forms are still useful for filing tax returns and claiming tax deductions. Like a W-2 that includes information about an individual's income, the Form 1095 contains information about health insurance for the previous year.
What is self insured coverage?
Employers that offer health coverage referred to as “self-insured coverage” send this form to individuals they cover, with information about who was covered and when. You can use Form 1095-C to help determine your eligibility for the premium tax credit.
Who will send 1095-C?
Certain employers will send Form 1095-C to certain employees, with information about what coverage the employer offered. The IRS has posted questions and answers about the Forms 1095-B and 1095-C.
What is a 1095-A?
Form 1095-A, Health Insurance Marketplace Statement. If you or your family had coverage through a Marketplace, the Marketplace will send you information about the coverage on Form 1095-A. The form will show coverage details such as the effective date, amount of the premium, and the advance payments of the premium tax credit or subsidy.
What is the simplest way to file a tax return?
Filing a tax return electronically is the simplest way to file a complete and accurate tax return as it guides you through the process and does all the math for you. Electronic Filing options include free Volunteer Assistance, IRS Free File, commercial software and professional assistance.
Who is required to send out a 1095-C?
Form 1095-C. Form 1095-Cis sent out by large employers who are required to offer health insurance coverage as a provision of the ACA. This applies to employers with 50 or more full-time equivalent employees. Form 1095-C is sent to the IRS and to the employees.
Who sends out 1095-A?
Form 1095-A is sent out by the health insurance exchanges (HealthCare.gov or a state-based exchange, depending on the state). This form is mailed to the IRS and to the policyholder.
What is a 1095-A?
Form 1095-A is your proof that you had health insurance coverage during the year , and it’s also used to reconcile your premium subsidy on your tax return, using Form 8962 (details below).
What to do if 1095-A is delayed?
If delivery of your 1095-A is delayed or the information on it is incorrect, you can contact your exchange. For the 2020 plan year, however, the rules are different. People who received excess premium tax credits in 2020 do not have to repay them to the IRS, and do not even have to file Form 8962 at all.
What does 1095-C mean?
For example, if you work for a large company and have access to coverage from your employer, but you opted to buy coverage in the exchange instead, you’d receive Forms 1095-A and 1095-C (the 1095-C would indicate that you were offered employer-sponsored coverage, even though you declined it).
Is Form 8962 required for 2020?
The information on Form 1095-A is used to complete Form 8962 (again, Form 8962 is not required for 2020 if you would have had to repay some or all of the premium tax credit; not filing it for 2020 will not affect subsidy eligibility in future years).
When will the IRS issue 1095-B?
The latest extension, detailed in IRS Notice 2020-76, gives insurers and employers until March 2, 2021, to distribute Forms 1095-B and 1095-C to plan members and employees.
