In order to have your supplies covered by Medicare, you musthave a prescription from your doctor, and receive the items over the counterfrom an authorized seller. The items must also be on Medicares approved list,otherwise they wont be covered.
Full Answer
What medical supplies are covered by Medicare?
Supplies. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually doesn’t cover common medical supplies that you typically use at home, like bandages and gauze. Medicare covers some supplies as durable medical equipment.
Which are medical supplies accept Medicare?
Dec 17, 2020 · That’s why we’ve launched an improved supplier directory to help you more easily search for suppliers of Medicare-covered equipment and supplies. Medicare’s improved supplier directory includes new features and functionality to help you: Customize your search with better search capabilities, and compare up to 3 suppliers at a time. The improved directory also …
Which medical services are covered by Medicare?
Oct 21, 2018 · In order to qualify, your equipment or medical supplies must be prescribed by and purchased from providers who participate in the Medicare program and accept assignment (you can search the directory for a supplier on Medicare.gov). In most cases, you pay 20 percent of the amount allowed under Medicare after you’ve met any applicable Part B deductible amounts.
How to get medical equipment through Medicare?
Step 1: Get an NPI. If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website. Not sure if you have an NPI? Search the NPI Registry.
What supplies will Medicare pay for?
DME that Medicare covers includes, but isn't limited to:Blood sugar meters.Blood sugar test strips.Canes.Commode chairs.Continuous passive motion devices.Continuous Positive Airway Pressure (CPAP) devices.Crutches.Hospital beds.More items...
How do I get a product approved by Medicare?
Go to an in-person doctor visit, where your doctor will write an order for the DME. Take the order to a Medicare-approved DME supplier. Depending on the product, ask the supplier if they will deliver it to your home. Find out if Medicare requires prior authorization for your DME.Jul 1, 2020
What can I use my Medicare card for?
You'll use your Original Medicare card to fill prescriptions only if they are covered by Medicare Part B (examples include drugs you administer through an infusion pump). In all other cases, you'll use your Part D prescription drug plan when filling prescriptions.Jul 10, 2021
Does Amazon accept Medicare?
En español | Already a household name in almost everything from books to electronics to household items, Amazon is now a major health care player with its new digital pharmacy that offers free home delivery and other perks to some customers with Medicare Part D, Medicare Advantage plans and most major commercial health ...Nov 30, 2020
Does Medicare pay for walkers and canes?
Usually, Medicare Part B covers 80% of allowable charges for walking canes and walkers; you pay 20% plus any remaining Part B deductible. A Medicare Supplement Insurance plan may be able to cover your 20% coinsurance for your walking cane, and other out-of-pocket costs not covered by Medicare Part A and Part B.Jul 25, 2021
Does Medicare pay for wheel chairs?
Medicare Part B (Medical Insurance) covers power-operated vehicles (scooters), walkers, and wheelchairs as durable medical equipment (DME). Medicare helps cover DME if: The doctor treating your condition submits a written order stating that you have a medical need for a wheelchair or scooter for use in your home.
Does your Medicare card expire?
Healthcare providers use the Medicare number on the card to bill services. Generally, a person does not have to renew their Medicare card each year, as it will automatically renew. If a card is lost, stolen, or damaged people can get a new card at no cost.Aug 11, 2020
Should I keep my Medicare card in my wallet?
Keep your Medicare Advantage Card: If you're in a Medicare Advantage Plan (like an HMO or PPO), your Medicare Advantage Plan ID card is your main card for Medicare – you should still keep and use it whenever you need care. However, you also may be asked to show your new Medicare card, so you should carry this card too.
Will the new Medicare cards be plastic?
The short answer is no. Medicare is not replacing your paper card with a plastic chip card. Scammers tried this con a few years ago. They've apparently fired it up again, as a lot of viewers are telling us about getting this call.Feb 25, 2022
Will Medicare pay for a walker from Amazon?
Medicare Part B (Medical Insurance) covers walkers as durable medical equipment (DME). The walker must be Medically necessary and prescribed by your doctor or other treating provider for use in your home. No, although exceptions exist under Medicare Part B (80%-20%) if deductibles are met.
How Much Does Medicare pay for a rollator walker?
In most cases, Medicare will pay 80% of the rolling walker costs. Be sure to check your supplemental insurance policy for the details of your plan that will cover whatever Medicare does not –minimizing as much out of pocket expense as possible.
What walkers Will Medicare pay for?
rollatorsMedicare will cover rollators as long as they're considered medically necessary, they're prescribed by a doctor and the doctor and supplier both accept Medicare assignment. Rollators are considered to be durable medical equipment just like walkers.Nov 18, 2021
What Types of Medical Supplies May Qualify For Medicare Coverage?
Only equipment or medical supplies prescribed by your health care provider may qualify for coverage under your Original Medicare Part B benefits, s...
What Are The Restrictions of Medicare Coverage For Medical Supplies?
Medicare coverage for durable medical equipment (DME) is part of your Part B benefits, provided that it is medically necessary and prescribed by yo...
Are Prescription Drugs Considered Medical Supplies Under Medicare?
Prescription drugs you take at home generally do not qualify for coverage under Original Medicare, Part A and Part B, except under very limited cir...
What medical supplies are covered by Medicare?
In general, the following types of medical supplies or DME would be eligible for Medicare coverage: Hospital beds, lifts, and commode chairs. Infusion pumps and supplies. Blood glucose monitors and test strips. Canes, crutches, walkers, and certain types of wheelchairs. Oxygen, nebulizers, and nebulizer supplies and medications.
What are the requirements for medical equipment?
Medicare requires that durable medical equipment (DME) be: 1 Durable (expected to last three years or more) 2 Medical in nature (used for a medical reason) 3 For use in your home 4 Generally, not useful to someone who isn’t injured or ill
How long does a DME last?
Medicare requires that durable medical equipment (DME) be: Durable (expected to last three years or more) Medical in nature (used for a medical reason) For use in your home. Generally, not useful to someone who isn’t injured or ill.
What is DME in Medicare?
Medicare coverage for durable medical equipment (DME) is part of your Part B benefits, provided that it is medically necessary and prescribed by your doctor for use at home. In order to qualify, your equipment or medical supplies must be prescribed by and purchased from providers who participate in the Medicare program and accept assignment ...
Does Medicare cover prescription drugs?
If you need prescription drug coverage, you may want to consider a Medicare plan that includes prescription drug coverage. Please note that a Medicare plan that includes prescription drug coverage will have a formulary, or a list of covered prescription drugs, and the formulary may change at any time ...
What is Medicare Advantage Plan?
A Medicare Advantage plan covers the same medical supplies and other health care services as Original Medicare (except for hospice care, which Part A still provides).
Is Medicare Part D a stand alone plan?
If you have health-care expenses for prescription drugs and are covered by Original Medicare, you may want to consider a stand-alone Medicare Part D Prescription Drug Plan to help lower your prescription drug costs now and in the future.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is part B?
Part B covers a once-per-lifetime health behavior change program to help you prevent type 2 diabetes. The program begins with weekly core sessions in a group setting over a 6-month period. In these sessions, you’ll get:
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is coinsurance in insurance?
Coinsurance: An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
How to get supplies through Medicare?
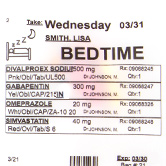
The first step to getting supplies through Medicare is to visit your doctor and get a diagnosis. A doctor’s confirmation that the supplies are medically necessaryis required for coverage. If you don’t see a doctor, you cannot get the paperwork necessary to get your supplies through Medicare.
How long does it take to enroll in Medicare?
We’ll collect the Medicare paperwork for you, set up monthly deliveries of supplies, and bill Medicare on your behalf. Enrollment takes just 5 minutes!
What is a Physician's Order?
A Physician’s Order is the most common document required by Medicare plans for incontinence supply coverage. It’s basically a prescription that establishes what urology products are needed for treatment. All urology products require a Physician’s Order for coverage.
What is an ABN?
Advanced Beneficiary Notice (ABN) An Advance Beneficiary Notice of Noncoverage (ABN) is a document that alerts individuals to the possibility that their supplies may not be covered by Medicare.
What is considered medically necessary?
Services or supplies are considered medically necessary if they: Are proper and needed for diagnosis, or treatment of your medical condition. Are provided for the diagnosis, direct care, and treatment of your medical condition. Meet the standards of good medical practice in the medical community of your local area.
What is medical record?
2. Medical Records: Medical Records are documents that contain the recorded medical history of a patient. They include notes about all your visits, lab tests, surgeries and medications. They are provided by a physician, and generally contain a history of all the conditions and healthcare services a person has received.
Does Medicare cover urology?
Medicare provides coverage for a wide range of urology products. Coverage may vary depending on need and your doctor’s orders, but here is a list of products that could potentially be received: Intermittent Catheters. Indwelling Catheters. Condom/External Catheters. Drainage Bags.
What is Medicare for Type 1 diabetes?
Medicare is a federally run health insurance program for people age 65 and older and people with disabilities. The best places to find information on the Medicare program are www.medicare.gov , the Medicare and You Handbook and the Medicare Plan Finder . This guide will provide some general detail about options for Medicare coverage and identify specific issues that are very important for people with type 1 diabetes (T1D) to understand as you make decisions about your Medicare coverage. Medicare consists of four basic parts, including: Part A, which covers primarily inpatient hospital and skilled nursing facility services. Part B, which covers primarily physician and outpatient hospital services, as well as durable medical equipment such as insulin pumps, test strips and some CGMs. Part C, also known as Medicare Advantage (MA) plans, are offered by private insurance companies and cover the same benefits as Medicare Part A and B, plus many offer drug coverage, similar to Part D Part D, which covers prescription drugs that you typically obtain at a pharmacy, and may also cover disposable insulin patch pumps. As a person with T1D, Parts B and D will be the most relevant to your day-to-day diabetes management. Well discuss why below. When you are eligible to enroll in Medicare, you have two basic options. The first option is to enroll in Original Medicare Parts A and B, which is managed by the federal government. Youll need to enroll in a Part D drug plan separately from your enrollment in Original Medicare since the Part D portion of the benefit is offered only through commercial insurers. Depending on your income, your costs for Part D coverage may be significantly reduced. In order to receive this reduction, you have to apply for the extra help. Theres no downside for a Continue reading >>
Does Medicare cover diabetic supplies?
Medicare Coverage of Diabetic Services and Supplies Medicare covers many diabetic services, if they are delivered by a doctor or other provider who accepts Medicare assignment. Medicare also covers a range of common diabetic supplies when theyre considered medically necessary. Different parts of the Medicare program cover the various aspects of diabetic treatment. What do Medicare Part B and Medicare Advantage plans cover? Medicare Part Bcovers diabetic test supplies, screenings, and education for beneficiaries with diabetes, or for those who are at risk for diabetes. Medicare Advantage, also called Medicare Part C, is optional private insurance. Medicare Advantage plans cover the same diabetic supplies and screenings that Medicare Part B covers. Medicare Advantage plans are required to provide at least the same amount of coverage as Original Medicare (Part A and Part B), except for hospice care. Medicare Part B covers diabetic supplies such as: Therapeutic shoes or sole inserts, if you meet all of these conditions: You have diabetes and youre being treated under a comprehensive diabetes care plan. You need therapeutic shoes or inserts because of your diabetes. In one or both feet, you have any of these: poor circulation, past foot ulcers, calluses that could lead to foot ulcers, deformity, nerve damage and potential callus problems because of diabetes, or partial or complete amputation. If you get therapeutic shoes or inserts, a podiatrist or other qualified doctor must prescribe them, and a doctor or other qualified individual like a pedorthist, orthotist, or prosthetist must fit and provide the shoes or inserts. Medicare Part B covers diabetic services such as: Up to two diabetes screenings each year if your doctor indicates youre at risk for diabetes. After the fir Continue reading >>
Does Medicare pay for blood glucose testing?
Blood glucose testing is an important part of diabetes management. Most insurance companies and Medicare/Medicaid will pay for blood glucose testing supplies. With private insurance or managed care, patients will most likely be asked to pay a co-pay to cover part of the cost of the supplies. Medicare pays for 80% of supplies once the patient has met their yearly deductible and the patient is responsible for the remaining 20% of the cost. See the www.Medicare.gov site for a full explanation of how your blood glucose testing supplies are covered. Prodigy Diabetes Care is contracted with certain insurance providers and state Medicaid programs, which may make the Prodigy brand products available to those individuals at a lower co-pay or no co-pay depending on the program. Continue reading >>