What is the lowest income to qualify for Medicare?
an individual monthly income of $4,379 or less. an individual resources limit of $4,000. a married couple monthly income of $5,892 or less. a married couple resources limit of $6,000.
What is the income limit for Medicare Colorado?
The income limit for Medicaid HCBS in Colorado is $2,349 a month if single and $4,698 a month if married (and both spouses are applying). In Colorado in 2020, spousal impoverishment rules can increase income between $2,155 and $3,216 per month for a non-applying spouse.
Can you have Medicare and Medicaid in Colorado?
Remember: Medicaid always pays last. Now that you are eligible for Medicare, Health First Colorado (Colorado's Medicaid program) requires you to use Medicare.
What is the income cutoff for Medicaid in CO?
See if you can sign up for Health First ColoradoFamily SizeApproximate Monthly Family Income to Qualify for Health First ColoradoAdults 19 – 64Children 0 – 181Up to $1,428Up to $1,5252Up to $1,931Up to $2,0623Up to $2,434Up to $2,5993 more rows
Is Medicare free in Colorado?
Nearly all Medicare recipients get Part A for free. If you do not get Part A for free, we will pay your Part A premiums if you are in the Qualified Medicare Beneficiary (QMB) tier of the Medicare Savings Program. If you get Part A free, we can still pay the Part B premiums even if you have refused or terminated Part B.
What is the Medicaid income limit for 2022 in Colorado?
Income & Asset Limits for Eligibility2022 Colorado Medicaid Long Term Care Eligibility for SeniorsType of MedicaidSingleMarried (both spouses applying)Medicaid Waivers / Home and Community Based Services$2,523 / month$5,046 / monthRegular Medicaid / Aged Blind and Disabled$841 / month$1,261 / month2 more rows•Dec 6, 2021
How do I apply for Medicare in Colorado?
Ways to sign up: Online (at Social Security) – It's the easiest and fastest way to sign up and get any financial help you may need. (You'll need to create your secure my Social Security account to sign up for Medicare or apply for benefits.) Call Social Security at 1-800-772-1213. TTY users can call 1-800-325-0778.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Is Medicare better than Medicaid?
Medicaid and Original Medicare both cover hospitalizations, doctors and medical care. But Medicaid's coverage is usually more comprehensive, including prescription drugs, long-term care and other add-ons determined by the state such as dental care for adults.
Who is qualified for Colorado Medicaid?
Be responsible for a child 18 years of age or younger, or. Blind, or. Have a disability or a family member in your household with a disability, or. Be 65 years of age or older.
Can adults qualify for Medicaid in Colorado?
Health First Colorado (Colorado's Medicaid program) is a public health assistance program for Coloradans who qualify. Children, pregnant women, parents and caretakers, people with developmental, intellectual, and physical disabilities, and adults can all potentially qualify.
What is the monthly income limit for food stamps in Colorado?
During this time, ABAWDs will not be required to meet the work requirement to keep receiving SNAP. For more information on COVID-19 and food assistance, visit this page....What you need to know.Household sizeGross monthly income limitsMaximum monthly allotment1$2,148$2502$2,904$4593$3,660$6584$4,418$8355 more rows
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
What does SLMB cover?
SLMB benefits cover the cost of the monthly Medicare Part B premium. The standard Part B premium in 2021 is $148.50 per month and is required of all Medicare Part B beneficiaries.
How do you qualify for SLMB?
Each state Medicaid program has its own rules concerning qualification.
What other Medicare Savings Programs are there?
SLMB is just one of the available Medicare Savings Programs. Others include:
How do you apply for SLMB?
Contact your state Medicaid program for information and assistance with applying for the SLMB program.
Is there Medicaid assistance for Medicare Advantage beneficiaries?
Individuals who qualify for both Medicare and Medicaid are considered “dual eligible” and may qualify for a certain type of Medicare Advantage plan called a Special Needs Plan. And one particular type of Special Needs Plan is a Dual Eligible Special Needs Plan (D-SNP).
Medicaid
Medicaid is a joint federal/state program that helps with medical costs for some people with limited income and resources.
Medicare Savings Programs
State Medicare Savings Programs (MSP) programs help pay premiums, deductibles, coinsurance, copayments, prescription drug coverage costs.
PACE
PACE (Program of All-inclusive Care for the Elderly) is a Medicare/Medicaid program that helps people meet health care needs in the community.
Lower prescription costs
Qualify for extra help from Medicare to pay the costs of Medicare prescription drug coverage (Part D). You'll need to meet certain income and resource limits.
Programs for people in U.S. territories
Programs in Puerto Rico, U.S. Virgin Islands, Guam, Northern Mariana Islands, American Samoa, for people with limited income and resources.
Find your level of Extra Help (Part D)
Information for how to find your level of Extra Help for Medicare prescription drug coverage (Part D).
Insure Kids Now
The Children's Health Insurance Program (CHIP) provides free or low-cost health coverage for more than 7 million children up to age 19. CHIP covers U.S. citizens and eligible immigrants.
What is Medicaid in Colorado?
Medicaid is a wide-ranging health care insurance program for low-income individuals of all ages. Jointly funded by the state and federal government, it provides health coverage for diverse groups of Colorado residents, including pregnant women, parents with dependent children, adults with no dependent children, disabled individuals, and seniors.
How long does Colorado have to look back on Medicaid?
This is because Colorado has a Medicaid Look-Back Period, which is 60 months (5 years) immediately preceding one’s Medicaid application date.
What is the exemption for Medicaid?
Exemptions include personal belongings, household furnishings, an automobile, irrevocable burial trusts, and one’s primary home, given the Medicaid applicant lives in it or is intending to live in it in the future, and has an equity interest in the home no greater than $603,000 (in 2021).
What is CSRA in Medicaid?
This is called the Community Spouse Resource Allowance (CSRA). As with the spousal income allowance, this asset allowance rule only applies to married couples with one spouse applying for institutional Medicaid or a Medicaid waiver. It does not apply to a married couple with one spouse applying for regular Medicaid.
What is NFLOC in nursing home?
For nursing home Medicaid and many HCBS Medicaid Waivers, a nursing facility level of care (NFLOC) is required. Furthermore, there may be additional eligibility requirements for some program benefits.
What are countable assets for Medicaid?
Countable assets include cash, stocks, bonds, investments, credit union, savings, and checking accounts, and real estate in which one does not reside. However, for Medicaid eligibility, there are many assets that are not counted. In other words, they are exempt from Medicaid’s asset limit.
How much does a nursing home need to pay monthly?
Instead, all of a beneficiary’s monthly income, with the exception of a personal needs allowance of approximately $89.55 / month, and possibly a monthly maintenance needs allowance for a non-applicant spouse, must be paid to the nursing home.
What is Medicaid coverage?
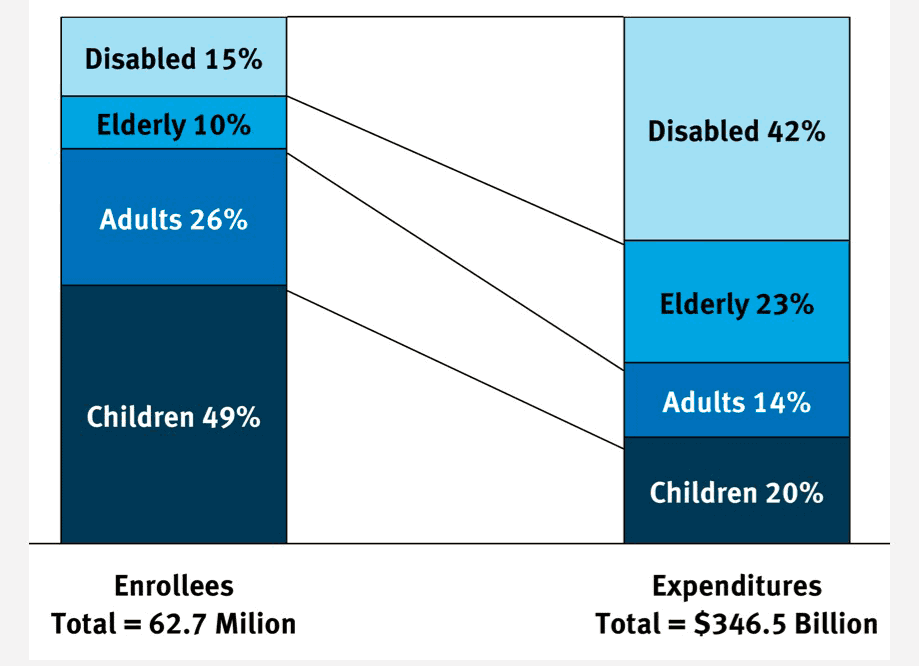
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
