A better way: combine Medicare A and B into a single health plan, with a single deductible and uniform cost-sharing. This would greatly simplify the program, making it more understandable for seniors.
Full Answer
What can prevent you from getting Medicaid?
Review of the Survey
- 26 states are aligning to TANF-funded cash assistance;
- 11 states are aligning to TANF/MOE-funded non-cash assistance, primarily child care;
- 11 states are using categorical eligibility;
- 3 states are using a combination of categorical eligibility and aligning to TANF/MOE-funded assistance.
How well does Medicaid work in improving access to care?
- Is there an initial health assessment that looks at medical problems and asks about functional needs?
- Does the insurer develop plans of care shared across its hospitals and doctors and with home- and community-based providers?
- How does it interact with home- and community-based providers like adult day care, Meals on Wheels and home care providers?
How does Medicaid help people with low income?
- Estate Recovery
- MAGI Conversion Plan
- Seniors & Medicare and Medicaid Enrollees
- Verification Plans
- Minimum Essential Coverage
- Spousal Impoverishment
- Medicaid Third Party Liability & Coordination of Benefits
- Medicaid Eligibility Quality Control Program
Who really pays for Medicaid?
Who Really Pays For Health Care Might Surprise You
- Before Obamacare we had a free-market health-care system. Government has been part of the business of medicine at least since the 1940s, when Washington began appropriating billions to build private ...
- I fully paid for Medicare through taxes deducted from my salary. ...
- Premiums from my paycheck fund my company health plan. Probably not entirely. ...

How can we improve Medicare?
4 Evidence Based Strategies for Improving MedicareHelp people pick the right Medicare plans for them. ... Rethink benefit design to improve medication adherence and reduce health disparities. ... Determine value in medical innovations. ... Curb fragmented prescribing of opoids.
How can Medicare be more sustainable?
Increase co-payments from retirees – putting more of the costs of the program on retirees is another way to make Medicare more sustainable. This has already occurred by increasing the Medicare Part B premiums and increasing deductibles.
How can Medicare problems be solved?
Call 1-800-MEDICARE (1-800-633-4227) You can call 1-800-MEDICARE and speak with a representative to ask questions about Medicare or get help resolving problems with Medicare. We made a test call to this number and were greeted by a polite Medicare representative after being on hold for about 90 seconds.
What are some of the biggest challenges with Medicare today?
Top concerns for Medicare beneficiaries: Part B, appeals and affordable medications. The top concerns of Medicare enrollees include navigating Part B, appealing Medicare Advantage (MA) denials and affording meds, according to an annual report from the Medicare Rights Center.
What should the US do to reform Medicare?
Congress should reform Medicare graduate medical education payments by converting the payments into direct grants to institutions sponsoring residency training programs; allowing ambulatory care settings such as physician groups to receive funding for sponsoring residencies; and cutting the total amount of spending by ...
What are two challenges to the long term sustainability of the Medicare program?
A shrinking taxpayer base, swelling beneficiary numbers and growing healthcare costs all threaten Medicare's long-term viability, according to the HHS, and the agency warned the program would need to increase its revenue or drastically reduce benefits to balance its budget.
What are 3 rights everyone on Medicare has?
— Call your plan if you have a Medicare Advantage Plan, other Medicare health plan, or a Medicare Prescription Drug Plan. Have access to doctors, specialists, and hospitals. can understand, and participate in treatment decisions. You have the right to participate fully in all your health care decisions.
Is Medicare a crisis?
A report from Medicare's trustees in April 2020 estimated that the program's Part A trust fund, which subsidizes hospital and other inpatient care, would begin to run out of money in 2026.
How do you maintain Medicare solvent?
Legislators and the president will need to either: increase revenues flowing into the trust fund by at least $700 billion to extend solvency to 2036 (experts typically focus on 10-year time horizons); cut spending on Medicare beneficiaries or increase their monthly premiums or figure out a combination of these two ...
What are the advantages or disadvantages to serving Medicare and Medicaid populations?
The takeaway Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
What would happen if Medicare ended?
Payroll taxes would fall 10 percent, wages would go up 11 percent and output per capita would jump 14.5 percent. Capital per capita would soar nearly 38 percent as consumers accumulated more assets, an almost ninefold increase compared to eliminating Medicare alone.
What are the cons of Medicare?
Cons of Medicare AdvantageRestrictive plans can limit covered services and medical providers.May have higher copays, deductibles and other out-of-pocket costs.Beneficiaries required to pay the Part B deductible.Costs of health care are not always apparent up front.Type of plan availability varies by region.More items...•
Who said it is important to have a plan of care that integrates medical services and home- and community services?
Says Chernof , a former general practitioner: “As a physician, I think it’s very important there be a plan of care that integrates medical services and home- and community services and one that’s built around a person’s goals, not just medical problems.”.
What would happen if the SCAN Foundation's proposals in its Top 10 Recommendations to Strengthen?
If The SCAN Foundation's proposals in its Top 10 Recommendations to Strengthen Integrated Care turn into reality , dual eligibles could have a better quality of life, which would be great for them and for their families. It might save the government some money, too.
Why are people over 65 considered dual eligible?
Roughly 11 million poor Americans over 65 have the most severe health needs: they’re called “dual eligibles,” because they’re eligible for Medicare’s medical benefits as well as for Medicaid’s long-term care benefits. Problem is, as Dr. Bruce Chernof, The SCAN Foundation ’s president and CEO, says: “Medicare and Medicaid don’t talk to each other, or work with each other, very well.”
Should CMS provide non-covered services?
CMS should “better define opportunities, incentives and parameters for health plans to provide non-covered services,” like home modifications and certain medical equipment, The SCAN Foundation report says. Right now, Medicare Advantage plans, the alternatives to “original Medicare” sold by private health insurers, require that supplemental benefits be “primarily health-related” and have strict limits on coverage for things like home-delivered meals and minor home modifications.
Does Pace reduce hospitalizations?
PACE has been found to reduce hospitalizations, nursing home use and mortality. And, Chernof says, some of the new dual-eligible demonstration projects have “reported some early successes and savings.”. Washington state’s, for example, generated over $60 million in Medicare savings over its first two years.
Does Medicare Advantage cover home delivery?
Right now, Medicare Advantage plans, the alternatives to “original Medicare” sold by private health insurers, require that supplemental benefits be “primarily health-related” and have strict limits on coverage for things like home-delivered meals and minor home modifications.
Can Medicare and Medicaid work together?
But Chernof says this is a problem both on the conceptual level (Medicare and Medicaid aren’t set up to work with each other) and on the operational level. He offers this example: To cover some home- or community-based services, Medicaid requires a denial letter from Medicare, but Medicare “will say it’s not a benefit [we provide], so we can’t deny it.”
How many people are covered by Medicare?
Medicare has undoubtedly helped millions of seniors and disabled adults receive health coverage since being signed into law in 1965. Today, Medicare covers 55 million beneficiaries across the US. In the coming decades though, Medicare faces a complex multitude of competing environmental pressures. First, the sheer size of the Medicare-eligible population is projected to increase significantly: according to the US census, by 2029 all the baby boomers will be 65 or older which will account for 20 percent of the US population. Adding to that increased pressure is the trends showing this population will be living with more disabilities and living longer than previous generations.
How does medical technology impact healthcare?
Policymakers acknowledge that new medical technologies can improve patient care. Yet they often focus on how these new products and services put fiscal strain on government budgets rather than their benefit to society. Recently, the Medicare Payment Advisory Commission cited medical technology as having the greatest impact on health care spending. Nevertheless, medical innovations can provide health benefits that outweigh their additional costs. By applying a framework for the quality-adjusted cost of care, which takes into account both value and direct financial costs, policymakers can gain more complete insight into the value of investments from Medicare into new medical technologies that better takes into account patients’ health outcomes.
What is fragmented prescribing of opioids?
Fragmented prescribing-whereby no specific physician is solely responsible for a patient’s needs for opioid prescription-or intentional doctor shopping by patients, lead to adverse health outcomes. We found that Medicare patients who received prescription opioids from four or more unique providers had twice the annual rate of hospital admission than those who received prescription opioids from only one provider.#N#STRATEGIES IN ACTION:
What are the four evidence-based recommendations that would measurably improve the delivery of services?
Through this research four evidence-based recommendations which would measurably improve the delivery of services have been found: 1. Help people pick the right Medicare plans for them. Center experts found that when Medicare beneficiaries choose a prescription drug plan, poor plan choices result in extra costs and reduced access to necessary drugs.
Will the baby boomer generation have a larger price tag?
With the increase in beneficiaries from the aging baby boomer generation inevitably will come a larger price tag. This is leading many policy and industry experts to speculate and worry about the program’s long term ability to provide quality and affordable coverage.
How many states have expanded Medicaid?
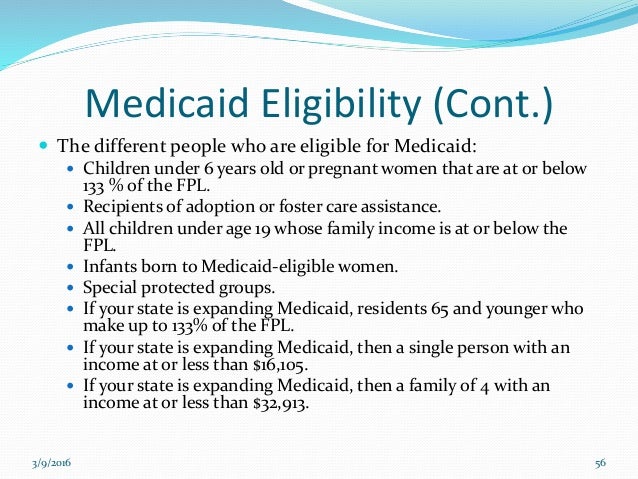
Expanding coverage. To date, 38 states and the District of Columbia have expanded Medicaid coverage under the Affordable Care Act (ACA) to individuals with incomes up to 133% of the federal poverty level.
How does the AMA work?
To expand access to care, the AMA works with state advocates to fully fund the Medicaid program and increase physician participation with policies to streamline enrollment, ensure fair audit procedures and improve managed care programs. Expanding coverage.
Is Medicaid a viable program?
Reform efforts must ensure that Medicaid is a viable and effective program to provide health insurance coverage to low-income individuals, seniors and the disabled .
Can a physician accept a new patient on medicaid?
Research demonstrates that low Medicaid reimbursement rates significantly affect a physician’s ability to accept new Medicaid patients. Physicians have a strong sense of responsibility to provide care for Medicaid patients, but cannot remain economically viable if they lose money on the care they provide. Without enough participating physicians, patients may have coverage but not real access to care.
Fix Medicare Part A
Medicare has an urgent solvency problem that impacts just one part of the program: Part A, which pays for hospital bills.
Control Drug Costs
The controversial new Alzheimer's drug OK'd by the U.S. Food and Drug Administration last year has put a bright spotlight on the issue of drug costs in Medicare.
Cover Dental, Hearing, and Vision Care
Medicare has never covered dental, hearing, or vision care, with a few exceptions. These gaping holes in care are bad for the well-being of seniors, and they lead to additional health problems that boost overall program costs. Studies have linked poor oral health with higher rates of diabetes, cardiovascular disease, and pulmonary infections.
Level the Playing Field
Medicare has been privatized on a massive scale over the past two decades, mainly through the Part D and Medicare Advantage. Advantage is on track to cover half of all enrollees by 2030, with very little public discussion of the implications for government spending and the well-being of participants.
Improve Protections for Low-Income Seniors
Affluent seniors are well-equipped to cope with the rising cost of Medicare. Higher premiums and out-of-pocket costs may be painful, but well-off seniors don't need to contemplate skipping their medications or choosing between buying groceries, rent, and healthcare bills.
Share This Article
Mark Miller does not own (actual or beneficial) shares in any of the securities mentioned above. Find out about Morningstar’s editorial policies .
Sponsor Center
Transparency is how we protect the integrity of our work and keep empowering investors to achieve their goals and dreams. And we have unwavering standards for how we keep that integrity intact, from our research and data to our policies on content and your personal data.
When will Medicare run out of money?
If medical expenses rise at an even quicker rate, the HI Trust could, in theory, run out of money by as early as 2022. Should the program burn through its cash safety valve, it would only be able to pay hospitals at a rate commensurate with what it's bringing in via payroll tax revenue.
How much is Medicare taxed?
Medicare is currently taken out as part of your payroll taxes along with Social Security at a rate of 2.9% of your modified adjusted gross income. Like Social Security, this tax is typically split down the middle between you and your employer, with each side paying 1.45%.
What does it mean to test for Medicare?
What's means testing? In short, it would entail using an income scale to determine whether or not someone actually "needs" Medicare or not. For instance, a low-income retiree with $40,000 in savings probably needs Medicare to help pay for qualified medical expenses, whereas a single retiree with $4 million in assets can likely afford to pay for medical care privately, without the use of Medicare. Removing well-to-do individuals and couples from the program could save it from unnecessary expenditures.
How much did Medicare spend in 2014?
First, Medicare Part D (drug plans) spending was "only" $78 billion in 2014, meaning even with staunch negotiations the program might only save between 2% and 5% of its total annual expenditures, by my estimate. That's not going to give the Medicare program much of an extension beyond 2030. The other issue is simply innovation.
How much Medicare did the average person pay in 2010?
As of 2010 (but based on 2012 dollars), the average man and woman were paying $61,000 in Medicare taxes over their lifetimes. Yet, men and women were receiving $180,000 and $207,000, respectively, worth of lifetime benefits (women have a longer life expectancy than men). This gap between taxes paid and benefits received is only expected ...
What is Bernie Sanders' plan?
Democratic Party candidate Bernie Sanders has suggested creating a universal health plan for Americans of all ages, which would require a 2.2% healthcare premium tax on all individuals and a 6.2% tax on employers. 2. Institute means-testing. Another popular solution would be to institute means testing.
Is it tougher for Medicare to police claims?
The problem is in convincing lawmakers that a model beyond the institutional hospital setting should be reimbursed. It may also be tougher for Medicare officials to police claims if they aren't made within the traditional settings of a hospital.
What happens if you don't sign up for Medicare?
Consider the bind you're in if you're one of them, age 65 or older. If you sign up for Medicare, you'll get no treatment in return for your premiums, because Medicare doesn't cover services abroad. If you don't sign up, you'll probably face a penalty when you return home: a 10 percent lifelong markup for every year you delayed (though having had qualifying health insurance while working abroad is an exception). "The penalty for late enrollment is unreasonable and punitive," says the Paris-based Association of Americans Resident Overseas. Many expats would also like to see Medicare move toward covering treatment abroad, as the U.S. military's Tricare program does.
What happens if you sign up for Medicare late?
If you're late signing up for Medicare, you may be hit with late penalties that permanently raise your premiums. A lesser-known penalty for lateness is that you can sign up only during an annual general enrollment period, Jan. 1 to March 31, and your coverage won't begin until July 1 of the same year.
What is the AARP reform?
Many consumer organizations, including AARP, have called for reform. Says the American Physical Therapy Association: "An arbitrary cap on outpatient therapy services without regard to clinical appropriateness of care discriminates against the most vulnerable Medicare beneficiaries.".
How long do you have to be inpatient for Medicare?
To qualify for reimbursed time at a skilled nursing facility after your hospital stay, you must be an "inpatient" for at least three days.
Does Medicare cover speech therapy?
In 2015, traditional Medicare covers outpatient physical therapy and speech therapy only up to $1,940 per year for the two combined. Occupational therapy is capped at the same amount, which doesn't buy much. Patients can apply for exceptions if therapy is "medically necessary," but the process is cumbersome and raises administrative costs. Many consumer organizations, including AARP, have called for reform. Says the American Physical Therapy Association: "An arbitrary cap on outpatient therapy services without regard to clinical appropriateness of care discriminates against the most vulnerable Medicare beneficiaries."
Why would seniors benefit from a single deductible?
And knowing they were protected from the potentially huge costs of catastrophic illness would give seniors peace of mind—crucial benefit for those living on fixed incomes.
Does Medicare pay for outpatient procedures?
Medicare generally pays more for inpatient hospital procedures and less for the same procedures performed in an outpatient setting. The Trump administration has started to promote “site neutrality” in Medicare payment—a move widely applauded by conservative analysts eager to unleash greater competition within the health-care sector.
Should Congress work with the President to end this statutory restriction?
Congress should work with the president to end this statutory restriction, break down barriers to competition within America’s hospital markets, and permit more Medicare beneficiaries to have access to the high-value of high-volume specialized medical care.
Is Medicare site neutral?
The Trump administration has started to promote “site neutrality” in Medicare payment —a move widely applauded by conservative analysts eager to unleash greater competition within the health-care sector. Once again, however, there is support from the left as well.
Should GME be funded separately?
They should finance GME separately, instead of through the traditional Medicare program. Moreover, GME funds should be allocated to the states, but should come with the proviso that the money will follow the medical resident. This change will let states allocate funds to insure that rural and remote areas receive a sufficient number of medical residents—something that would not only benefit Medicare beneficiaries in those areas, but also broaden the training experience of new physicians.
What is CMS's role in the HHS?
CMS is the lead agency for a number of actions in the HHS Disparities Action Plan, including efforts to increase access to dental care for children in Medicaid and CHIP, and improve language access in Medicaid and CHIP.
What is the HHS Action Plan?
HHS Action Plan to Reduce Racial and Ethnic Disparities. HHS unveiled its Action Plan to Reduce Racial and Ethnic Health Disparities ("HHS Disparities Action Plan") in April 2011, which outlines goals and actions HHS will take to reduce health disparities among racial and ethnic minorities.
What is CMS in healthcare?
As part of the overarching Centers for Medicare & Medicaid Services (CMS) initiative to support health care quality improvement to underserved Medicare and Medicaid enrollees, CMS is engaged in a multi-partner health disparities collaboration. This unique collaboration includes:

Fix Medicare Part A
Control Drug Costs
- The controversial new Alzheimer's drug OK'd by the U.S. Food and Drug Administration last year has put a bright spotlighton the issue of drug costs in Medicare. Aduhelm is administered by healthcare providers, so it is covered under Part B, and it was a big factor in the eye-popping increase in the Part B premium this year. Biogen (BIIB), which makes the drug, announced in Dec…
Cover Dental, Hearing, and Vision Care
- Medicare has never covered dental, hearing, or vision care, with a few exceptions. These gaping holes in care are bad for the well-being of seniors, and they lead to additional health problems that boost overall program costs. Studies have linkedpoor oral health with higher rates of diabetes, cardiovascular disease, and pulmonary infections. Vision loss and hearing loss are associated w…
Level The Playing Field
- Medicare has been privatized on a massive scale over the past two decades, mainly through the Part D and Medicare Advantage. Advantage is on track to cover half of all enrollees by 2030, with very little public discussion of the implications for government spending and the well-being of participants. Medicare Advantage is popular with many seniors. But in part, it's growth stems fro…
Improve Protections For Low-Income Seniors
- Affluent seniors are well-equipped to cope with the rising cost of Medicare. Higher premiums and out-of-pocket costs may be painful, but well-off seniors don't need to contemplate skipping their medications or choosing between buying groceries, rent, and healthcare bills. But half of Medicare beneficiarieshad per capita income below $29,650 in 2019...