How to properly compose Medicare appeal letter and its sample?
Filing an initial appeal for Medicare Part A or B: File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare’s decision is …
How to file and win a Medicare appeal?
Write your Medicare Number on all documents you submit with your appeal request. • You must send your request for a redetermination to the MAC at the address listed in the “File an Appeal in Writing” section of your MSN. 2. Fill out a “Medicare Redetermination Request” form (CMS Form number 20027). To get a copy, visit CMS
When can I file an appeal to a Medicare claim?
At each level, you'll get instructions in the decision letter on how to move to the next level of appeal. Level 1: Reconsideration from your plan; Level 2: Review by an Independent Review Entity (IRE) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council)
How to write an appeal letter [sample template]?
If the plan or doctor agrees, the plan must make a decision within 72 hours. The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.

What should I say in a Medicare appeal?
- your name and address.
- your Medicare number (as shown on your Medicare card)
- the items you want Medicare to pay for and the date you received the service or item.
- the name of your representative if someone is helping you manage your claim.
How do I write an effective insurance appeal letter?
- Patient name, policy number, and policy holder name.
- Accurate contact information for patient and policy holder.
- Date of denial letter, specifics on what was denied, and cited reason for denial.
- Doctor or medical provider's name and contact information.
What are the chances of winning a Medicare appeal?
What are the five levels for appealing a Medicare claim?
How do you write a basic appeal letter?
- Review the appeal process if possible.
- Determine the mailing address of the recipient.
- Explain what occurred.
- Describe why it's unfair/unjust.
- Outline your desired outcome.
- If you haven't heard back in one week, follow-up.
- Appeal letter format.
What are the first steps that must be taken before you begin to write the appeal letter?
- Step 1: Use a Professional Tone. ...
- Step 2: Explain the Situation or Event. ...
- Step 3: Demonstrate Why It's Wrong or Unjust. ...
- Step 4: Request a Specific Action. ...
- Step 5: Proofread the Letter Carefully. ...
- Step 6: Get a Second Opinion.
How do I fight Medicare denial?
How long does Medicare have to respond to an appeal?
How do I dispute a Medicare claim?
Can providers appeal denied Medicare claims?
How do I appeal a Medicare Part B premium?
What is the difference between reconsideration and redetermination?
Can you appeal a Medicare Advantage plan?
Medicare Advantage plans, which are administered by private insurance companies, are required by Medicare to have an appeals process by which you can get a redetermination if your plan denies you a service or benefit you think should be covered. If you disagree with the decision, you can request an independent review.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
What is a denial of a request?
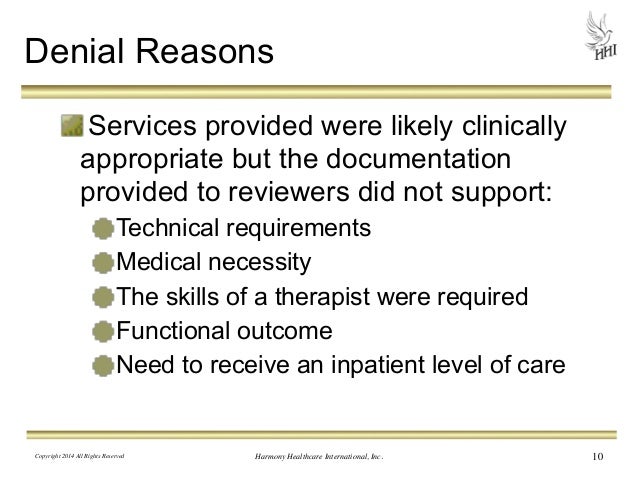
Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition. Denials of a request you and your doctor have made to change the price you pay for a prescription drug. For example: Your Medicare Part D drug plan rejects ...
Can you appeal a Part D plan?
If your life or health could be at risk by having to wait for a medication approval from your plan, you or your doctor can request an expedited appeal by phone. If you disagree with your Part D plan’s decision, you can file a formal appeal.
How long does it take to appeal a Part D plan?
The first level of appeal is to your plan, which is required to notify you of its decision within seven days for a regular appeal and 72 hours for an expedited appeal. If you disagree with this decision, you can ask for an independent review of your case.
Is a wheelchair medically necessary?
For example: Medicare determines that a wheelchair is not medically necessary for your condition. Denials of a request you and your doctor have made to change the price you pay for a prescription drug.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Can you request a fast reconsideration?
If you disagree with the plan’s redetermination, you, your representative, or your doctor or other prescriber can request a standard or expedited (fast) reconsideration by an IRE. You can’t request a fast reconsideration if it’s an appeal about payment for a drug you already got.
How long does it take to appeal a health insurance plan?
If the plan or doctor agrees, the plan must make a decision within 72 hours.
How long does it take for a health insurance plan to make a decision?
If the plan or doctor agrees, the plan must make a decision within 72 hours. The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision.
What is BFCC QIO?
Centered Care Quality Improvement Organization (BFCC-QIO)—A type of QIO (an organization under contract with Medicare) that uses doctors and other health care experts to review complaints and quality of care for people with Medicare.
What is a medical letter of appeal?
It is the responsibility of a health insurance company to cover for a patient’s medical claim as long as that patient’s coverage is still active. In some cases, however, an insurance company may deny a medical claim and give reasons for doing so.
Can insurance companies deny medical claims?
However, the law requires insurance companies to give an objective reason for denying a medical claim. If the reasons provided are not clear, or less convincing, a patient or their physician can write a professional letter to appeal the decision by the insurance company.
Can insurance deny a claim?
A health insurance company may deny a medical claim, making it hard for an insured patient to access medical care. If this ever happens, you will need to write a professional letter to appeal the claim. Here are some examples of medical appeal letter templates that you can download and use.
Does insurance cover medical claims?
It is the responsibility of a health insurance company to cover for a patient’s medical claim as long as that patient’s coverage is still active. In some cases, however, an insurance company may deny a medical claim and give reasons for doing so.
Does health insurance cover everything?
Download. Health insurance is as significant as any other type of coverage. But, just because you have a cover doesn’t mean that your insurance company will cover for everything that your doctor orders. Sometimes, your insurance company will deny your claim, so it is up to you to follow up to understand why they made that kind of a decision.
What is an appeal letter?
An appeal letter is something you write if you feel you’ve been treated unfairly in some way in your workplace, and you want someone to reconsider a decision they made about you. There are various times you might need to write an appeal letter.
How to write a letter to a friend?
Be confident and persuasive, but not aggressive. Consider asking a friend to read through the letter to make sure the tone is appropriate. Admit Any Mistakes.
Who is Alison Doyle?
Alison Doyle is the job search expert for The Balance Careers , and one of the industry's most highly-regarded job search and career experts. An appeal letter is something you write if you feel you’ve been treated unfairly in some way in your workplace, and you want someone to reconsider a decision they made about you.
Can you file a complaint with Medicare?
You can file a complaint if you have concerns about the quality of care or other services you get from a Medicare provider. How you file a complaint depends on what your complaint is about.
What is the difference between a complaint and an appeal?
What's the difference between a complaint and an appeal? A complaint is about the quality of care you got or are getting. For example, you can file a complaint if you have a problem calling the plan, or you're unhappy with how a staff person at the plan treated you. You file an appeal if you have an issue with a plan's refusal to cover a service, ...
What is a complaint in health care?
A complaint is about the quality of care you got or are getting. For example, you can file a complaint if you have a problem calling the plan, or you're unhappy with how a staff person at the plan treated you. You file an appeal if you have an issue with a plan's refusal to cover a service, supply, or prescription. Learn more about appeals.
