Go to an in-person doctor visit, where your doctor will write an order for the DME. Take the order to a Medicare-approved DME supplier. Depending on the product, ask the supplier if they will deliver it to your home.
Full Answer
What DME does Medicare pay for?
What durable medical equipment does Medicare cover? Medicare covers a range of items, supplies and equipment such as durable medical equipment. The list of DME that is covered by Medicare includes (but is not limited to): Air-fluidized beds and various other support surfaces Blood pressure monitors Blood sugar monitors Blood sugar test strips Canes
Does Medicaid cover DME?
“Medicare does not currently pay for over-the-counter ... As of Jan. 15, people with private health insurance have been eligible for coverage of up to eight at-home tests per month, per person ...
What does Medicare cover DME?
What Equipment Does Medicare Pay For?
- Glucose monitors and strips
- Prosthetics
- Hospital beds
- Lancet devices & lancets
- Canes
- Wheelchairs & scooters
- Commode chairs
- Oxygen equipment & accessories
- Suction pumps
- Continuous Positive Airway Pressure (CPAP) devices
How do I become a Medicare DME provider?
3 Steps to Becoming DME Supplier for Medicare
- Acquire a National Providers Identification (NPI) Number If you don’t have one already, you won’t meet the DME license requirements. ...
- Complete Your Medicare Enrollment Application You will need to complete the enrollment application using the PECOS’s online system through their website here.
- Work with Your Medicare Administrative Contractor (MAC)

How do I get a product approved by Medicare?
Go to an in-person doctor visit, where your doctor will write an order for the DME. Take the order to a Medicare-approved DME supplier. Depending on the product, ask the supplier if they will deliver it to your home. Find out if Medicare requires prior authorization for your DME.
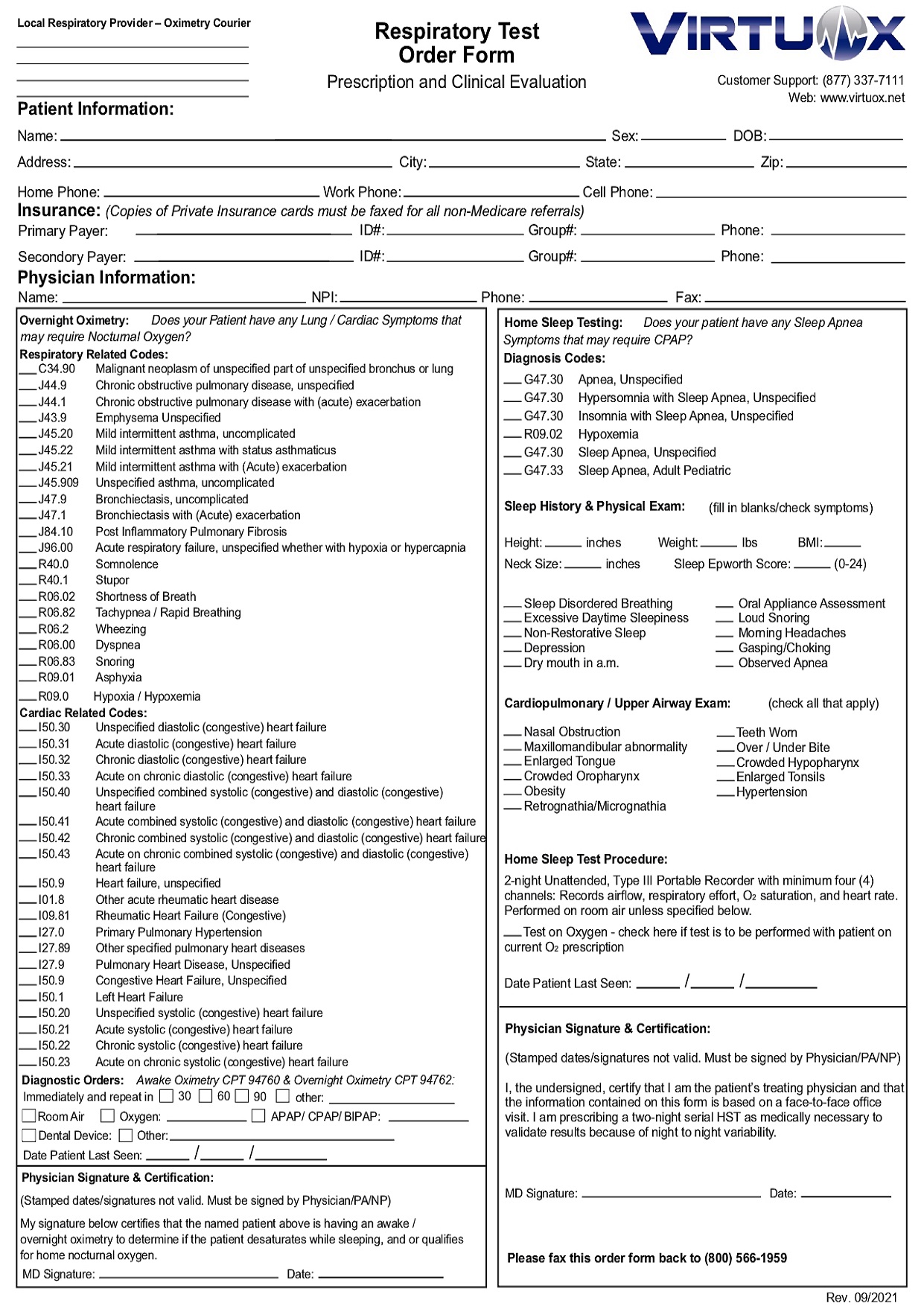
How do you write a prescription for durable medical equipment?
Your prescription can be handwritten on a standard prescription pad. It must include the physician's name, contact information and signature of the care provider; your name; and a statement about the equipment needed, for example "Oxygen at LPM" “CPAP” , “BiPAP”, “CPAP Mask”, “CPAP Humidifier” or “CPAP Supplies”.
How often can you get DME from Medicare?
Note: The equipment you buy may be replaced if it's lost, stolen, damaged beyond repair, or used for more than the reasonable useful lifetime of the equipment, which is generally 5 years from the date you start using the item. If you rent DME and other devices, Medicare makes monthly payments for use of the equipment.
Is DME covered by Medicare Part B?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What DME is not covered by Medicare?
This includes stairway elevators, grab bars, air conditioners, and bathtub and toilet seats. Items that get thrown away after use or that are not used with equipment. For example, Medicare does not cover incontinence pads, catheters, surgical facemasks, or compression leggings.
What is a standard written order?
Standard Written Order (SWO) All claims for items billed to Medicare require a written order/prescription from the treating practitioner as a condition for payment. This written order/prescription is referred to as the Standard Written Order (SWO). / Beneficiary's name or Medicare Beneficiary Identifier (MBI)
Does Medicare cover toilet risers?
Medicare generally considers toilet safety equipment such as risers, elevated toilet seats and safety frames to be personal convenience items and does not cover them. Medicare Advantage may offer some coverage if your plan includes supplemental OTC benefits.
What are the documentation guidelines for durable medical equipment DME )?
Documentation, including pertinent portions of the beneficiary's medical records (e.g., history, physical examination, diagnostic tests, summary of findings, diagnoses, treatment plans), supporting the medical necessity of the prescribed PMD must be furnished to the supplier within 45 days of the examination.
Is Amazon a Medicare supplier?
En español | Already a household name in almost everything from books to electronics to household items, Amazon is now a major health care player with its new digital pharmacy that offers free home delivery and other perks to some customers with Medicare Part D, Medicare Advantage plans and most major commercial health ...
What part of Medicare will pay a pharmacy for durable medical equipment DME quizlet?
Medicare Medical Insurance (Medicare Part B) pays for doctor's services; outpatient hospital care; durable medical equipment; and some medical services that are not covered by Part A.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Does Medicare pay for walkers and shower chairs?
Q: Will Medicare cover the cost of wheelchairs and walkers? A: Yes. Medicare Part B covers a portion of the cost for medically-necessary wheelchairs, walkers and other in-home medical equipment.
What is a DMEPOS file?
The DMEPOS public use file contains fee schedules for certain items that were adjusted based on information from the DMEPOS Competitive Bidding Program in accordance with Section 1834 (a) (1) (F) of the Act.
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
What is gap filling in Medicare?
For newly covered items of DMEPOS paid on a fee schedule basis where a Medicare fee does not exist , the Centers for Medicare & Medicaid Services (CMS) uses a process to establish fees called gap-filling. This allows Medicare to establish a price that aligns with the statutory requirements for the DMEPOS fee schedule.
What is TTFT in Medicare?
TTFT is a system consisting of an electromagnetic field generator and transducer arrays and will be covered under the Medicare Part B benefit for durable medical equipment (DME) for items and services furnished on or after September 1, 2019.
When will Medicare change the KU modifier?
As aforementioned, these system changes will be implemented on July 1, 2020.
What is a CGM?
CGMs are items of durable medical equipment (DME) that provide critical information on blood glucose levels to help patients with diabetes manage their disease . In January 2017, CMS issued a ruling providing for Medicare coverage of therapeutic CGMs.
Does Medicare cover CGMs?
Based on input from patients and other stakeholders, The Centers for Medicare & Medicaid Services (CMS) is announcing important changes in its written policies regarding how Medicare covers continuous glucose monitors (CGMs). These changes are consistent with the Agency’s approach of putting patients first and incentivizing innovation and use of e-technology.
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
What does DMEPOS mean?
When you opt out or enroll as an ordering and certifying provider, Medicare coverage will apply when you order or certify: Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Clinical Laboratory Services. Imaging Services. Home Health Services.
Is there a duplicate NPI?
There are no duplicates in the file. Many physicians and non-physician practitioners share the same first and last name; each unique NPI assures that nobody is included more than once. Deceased physicians and non-physician practitioners are not included in the file.
What is DME in medical terms?
If you're managing a health condition or recovering from an operation , you might need durable medical equipment, or DME. Durable medical equipment includes things like wheelchairs, oxygen machines, walkers and hospital beds. Just like medication, your doctor will write a prescription for the equipment you need.
Does Medicare cover medical equipment?
All Medicare plans cover basic equipment for you to use at home. If you need something more advanced, your plan may still cover it if your doctor says it's medically necessary. Usually, you'll only be responsible for paying coinsurance. However, each plan covers durable medical equipment a little differently.
Does a durable medical equipment plan have a deductible?
However, each plan covers durable medical equipment a little differently. Some plans only cover certain brands or equipment from specific manufacturers. Some plans require you to pay a deductible before they begin to pay for your durable medical equipment.
What is a standardized DMEPOS order?
Standardized DMEPOS Written Order/Prescription. Any Medicare provider or supplier that writes DMEPOS orders or prescriptions will now use a standard set of elements that will be applicable to all DMEPOS items. The treating practitioner must submit the complete written order to the supplier prior to submitting a claim for Medicare payment.
Who maintains the written order/prescription?
A supplier must maintain the written order/prescription and the supporting documentation provided by the treating practitioner and make them available to CMS and its agents upon request. CMS may suspend the face-to-face encounter and written order prior to delivery requirements generally, or for a particular item or items, ...
When was CMS 1713 finalized?
Final Rule CMS-1713: The rule, finalized in 2019, streamlines the requirements for ordering DMEPOS items, and develops a new list of DMEPOS items potentially subject to a face-to-face encounter, written orders prior to delivery, and/or prior authorization requirements.
Can CMS suspend a face to face meeting?
CMS may suspend the face-to-face encounter and written order prior to delivery requirements generally, or for a particular item or items, at any time and without creating a new rule, except for those items included on the Master List due to statutory mandate.
Do PMDs require face to face encounter?
Some items (such as PMDs) have statutorily imposed requirements. For items that do not have statutory requirements, a face-to-face encounter and written order is required only if the item is selected from the Master List and placed on the Required Face-to-Face and Written Order Prior to Delivery List. Items selected for the list will be published ...
What is DMEPOS in Medicare?
Suppliers who receive Medicare reimbursement for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) are required to: If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers.
What to do if your business doesn't dispense DMEPOS?
If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should refer to the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing information?
It’s important to keep your enrollment information up to date. To avoid having your Medicare billing privileges revoked, be sure to report any change within 30 days. Changes include, but are not limited to: a change in ownership. an adverse legal action. a change in practice location.
What chapter does Medicare have to be in before dispensed with DMEPOS?
As noted in the Medicare Program Integrity Manual, Chapter 5 (Items and Services Having Special DME Review Considerations), before you dispense any DMEPOS item to a beneficiary, you need to have an order from the treating physician.
What is a detailed written order?
detailed written order may be a photocopy, facsimile image, electronic, or pen-and-ink original document. For all items, the supplier shall have a detailed written order prior to submitting a claim.
Do you need a written order for DMEPOS?
While many items of DMEPOS can be dispensed based on a verbal order or preliminary written order from the treating physician/practitioner, there are certain items that statutorily require a written order prior to dispensing/delivery and are subject to face-to-face requirements.
