
How to get Both Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
What's the income level requirement to qualify for Medicaid?
What’s the Income Level Requirement to Qualify for Medicaid?
| Family Size | 100% | 120% | 140% | 150% |
| 1 | $11,770 | $14,124 | $16,478 | $17,655 |
| 2 | $15,930 | $19,116 | $22,302 | $23,895 |
| 3 | $20,090 | $24,108 | $28,126 | $30,135 |
| 4 | $24,250 | $29,100 | $33,950 | $36,375 |
What are the requirements for Medicaid in Utah?
What are the Income Requirements for Medicaid in Utah?
- A single applicant cannot exceed a maximum annual income of $15,800.
- A two-person household cannot exceed a maximum annual income of $21,307.
- A three-person household cannot exceed a maximum annual income of $26,813.
- A four-person household cannot exceed a maximum annual income of $32,319.
What is the annual income limit for Medicaid?
[Please note that the annual income limit for Medicaid for Employees with Disabilities enrollees is $75,000 and asset limits are much higher. For more on Medicaid for Employees with Disabilities, please scroll down this page or visit www.ct.gov/med. For information on applying, please follow this link.
How do you verify Medicaid eligibility?
- Provider Registration
- Verify Eligibility
- CoverRx
- Managed Care Organizations
- Medicare/Medicaid Crossover Claims
- Miscellaneous Provider Forms
- Pharmacy
- Report Provider Fraud
- Current P.O. Box List
- Electronic Data Interchange

How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
What is the income limit for Medicaid in Utah?
Income & Asset Limits for Eligibility2022 Utah Medicaid Long Term Care Eligibility for SeniorsType of MedicaidSingleMarried (both spouses applying)Regular Medicaid / Aged, Blind or Disabled$1,133 / month (eff. 3/1/22-2/28/23)$1,526 / month (eff. 3/1/22-2/28/23)3 more rows•Jan 10, 2022
Can you have Medicare and Medicaid?
Medicare-Medicaid Plans Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They're called Medicare-Medicaid Plans.
Who qualifies for Medicare in Utah?
65 or olderIn Utah, as in the rest of the country, you're eligible for Medicare if you're 65 or older and either an American citizen or a legal permanent resident who has lived here at least five continuous years.
Is it hard to get Medicaid in Utah?
To be eligible for Medicaid, you must meet a program type and meet the rules for Utah residency, income, and citizenship. An individual must qualify each month for continued coverage. The monthly income standard varies between approximately 55% and 133% of the Federal Poverty Level, depending on category.
What qualifies as low-income in Utah?
To qualify for Utah Section 8, first examine your household income. You cannot earn more than the annual low-income limits for your household size. For a household of one, your annual income cannot exceed $40,150 to be considered low-income, while a family size of five cannot earn more than $61,950 a year.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Which is a combination Medicare and Medicaid option that combines medical?
What are dual health plans? Dual health plans are designed just for people who have both Medicaid and Medicare. They're a special type of Medicare Part C (Medicare Advantage) plan. Dual health plans combine hospital, medical and prescription drug coverage.
How much does Medicare cost in Utah?
Medicare in Utah by the NumbersPeople enrolled in Original MedicareAverage plan costAnnual state spending per beneficiary247,159Plan A: $0 to $499 per month* Plan B: $170.10 per month**$9,103
Who qualifies for Medicaid?
To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, 177.87 KB).
What age can you get Medicare in Utah?
In Utah, as in the rest of the country, you're eligible for Medicare if you're 65 or older and either an American citizen or a legal permanent resident who has lived here at least five continuous years.
Who are the dual-eligible recipients?
People who are dual-eligible for Medicare and Medicaid are referred to as dual-eligible beneficiaries. Moreover, each state determines Medicaid coverage, and as a result, Medicaid benefits may differ.
Medicare Ineligibility
The Medicare eligibility requirement is that you must be 65 years old or older. If you or your spouse are 65 years old or older and have paid enough Medicare taxes through previous employment, you or your spouse may be eligible for premium-free Part A of the Medicare program (hospital coverage).
Medicaid Ineligibility
Medicaid eligibility varies depending on where a person resides, as various states have different qualifications.
Dual eligibility
A person must qualify for either partial-dual or full-dual coverage to be eligible for both Medicare and Medicaid.
Variations in geography
Medicaid benefits and coverage vary from one state to the next, and there are differences between them. Depending on the state, Medicaid coverage may be available to those who earn more than the standard income limits.
Medicare Part D Extra Assistance Program
Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual.
Summary
A person’s health and income level may qualify them for both Medicare and Medicaid.
How to apply for medicaid in Utah?
You can apply for Utah Medicaid either online, by mail, by fax, or in person. To apply in person, find a Department of Workforce Services (DWS) office near you.
What are the benefits of Medicaid in Utah?
Dental benefits for Utah Medicaid members include preventive services like six-month checkups, cleanings, and X-rays as well as fillings, root canals, pullings, dentures, and surgical care/emergencies. Children can also get space maintainers and some orthodontic care.
What counties does Utah Medicaid work with?
Anyone in Box Elder, Cache, Davis, Iron, Morgan, Rich, Salt Lake, Summit, Tooele, Utah, Wasatch, Washington, or Weber counties is required to select one of the four. Anyone in another county can choose an ACO but does not have to. The benefit of joining an ACO is that they might offer additional benefits that the Medicaid program does not provide on its own. The advantage of not selecting an ACO is that you can see any doctor that accepts Utah Medicaid insurance.
What is the Healthy U plan?
The Healthy U plan from University of Utah Health Plans offers statewide coverage, virtual healthcare appointments, a 24-7 nurse helpline, and more. They also specialize in Diabetes care and treatment and cover most exams, tests, and vaccinations related to your ongoing diabetes management.
Does Utah have a PDL?
Since 2007, Utah has used a preferred drug list (PDL) to administer prescription benefits. As of 2009, doctors who want to prescribe you a non-preferred drug will need to seek prior approval from the state Medicaid program. Your drug list will vary based on whether you are in the regular Utah Medicaid program or an Accountable Care Organization. Each ACO has its own PDL.
Can you use Medicaid in Utah?
Non-emergency Medical Transportation. If you are eligible for Traditional Medicaid and do not have your own means of transportation, you can use the Utah Medicaid non-emergency medical transportation system.
Is Medicaid a federal program?
While Medicaid is a federal program, each state has some liberties to decide what’s covered, how it’s covered, and who is eligible. The Utah Medicaid program may be able to cover most of your healthcare needs at a minimal cost.
What is Medicaid in Utah?
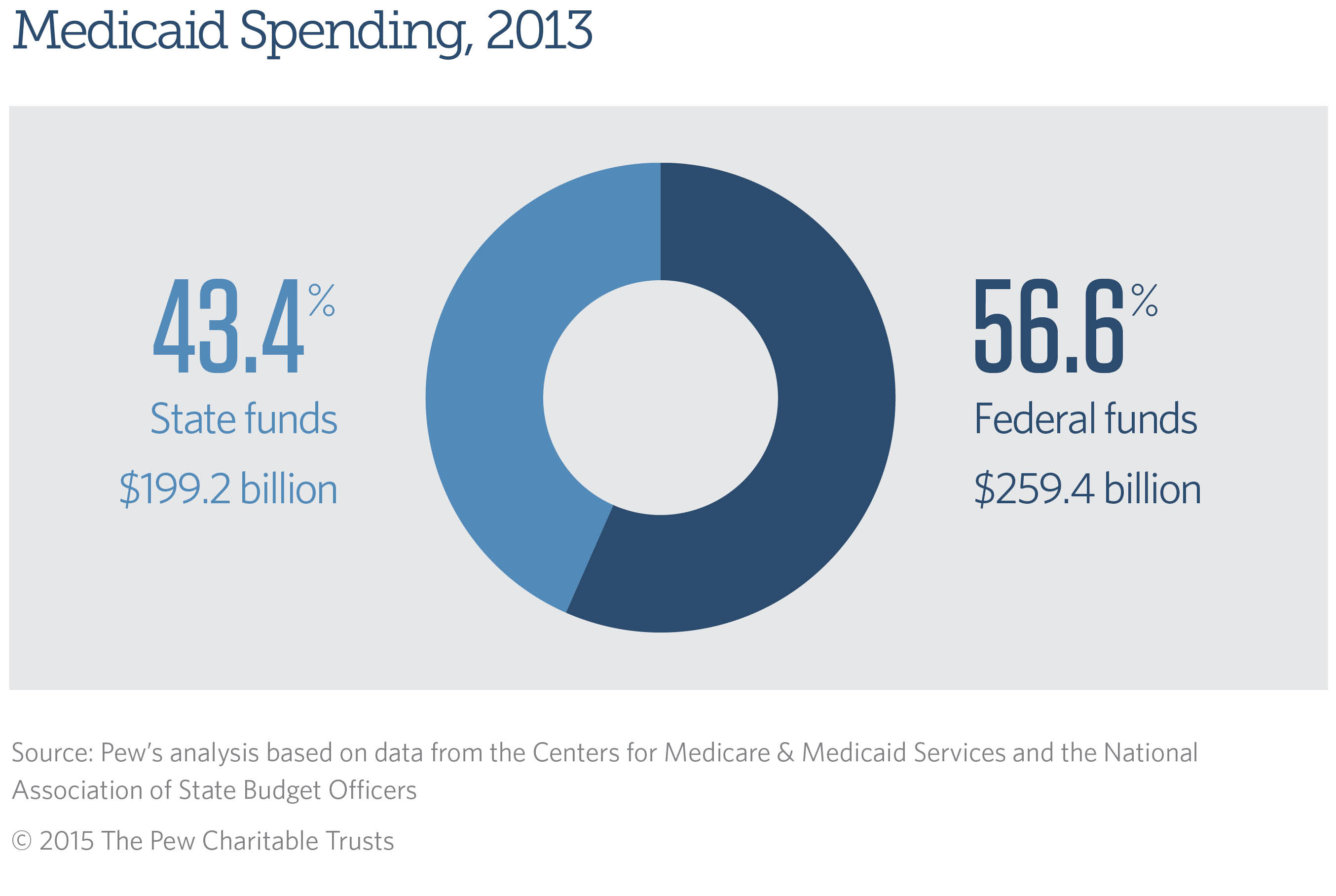
Medicaid is a wide-ranging health insurance program for low-income individuals of all ages. Jointly funded by the state and federal government, it provides health coverage for various groups of Utah residents, including pregnant women, parents and caretaker relatives, adults with no dependent children, disabled individuals, and seniors.
How much is the equity in a home for Medicaid in 2021?
One’s primary home, given the Medicaid applicant lives in it or has “intent” to return to it, and his or her home equity interest is not more than $603,000 (in 2021), is exempt. (The amount of the home’s value owned by the applicant is his or her equity interest in the home).
How much can a spouse retain in a nursing home in 2021?
In 2021, for married couples with just one spouse applying for Medicaid nursing home care or a HCBS waiver, the community spouse can retain half of the couples’ joint assets (up to a maximum of $130,380), as shown in the chart above.
What is Utah State Plan Personal Care Services?
1) Utah State Plan Personal Care Services – assistance with daily living activities is provided via the state Medicaid plan (available to anyone who meets the eligibility requirements) to promote independent living and prevent nursing home admissions. Benefits include aid with mobility, preparation of meals, bathing, grooming, and toiletry.
What is MMMNA in Medicaid?
For married couples, with non-applicant spouses’ of institutional Medicaid applicants or HCBS Medicaid waiver applicants with insufficient income in which to live, there is a Minimum Monthly Maintenance Needs Allowance (MMMNA). The MMMNA is intended to ensure non-applicant spouses do not become impoverished.
What are countable assets for Medicaid?
Countable assets include cash, stocks, bonds, investments, promissory notes, credit union, savings, and checking accounts, and real estate in which one does not reside. However, for Medicaid eligibility purposes, there are many assets that are not counted. In other words, they are exempt.
Do you need nursing home for Medicaid?
For nursing home Medicaid and home and community based services via a Medicaid waiver, a nursing home level of care is required. Furthermore, some program benefits may require additional eligibility criteria be met.
What is Medicaid in Utah?
Medicaid is a medical program for people who have low-income and limited resources. To be eligible for Medicaid, you must meet a program type and meet the rules for Utah residency, income, and citizenship. An individual must qualify each month for continued coverage.
Can a provider accept Medicaid?
If the provider accepts Medicaid, Medicaid may pay for the service.
Can you return to a provider with a medicaid card?
A person who received medical, dental, or mental health services and subsequently qualifies for Medicaid may return to each provider with a Medicaid Identification Card for the month in which service was provided.
When does Medicaid coverage begin?
Coverage begins the first of the month following the month the member is determined eligible. A Medicaid card will be issued each month. If the individual does not receive Medicaid, the card will read “MEDICARE COST-SHARING ONLY.”. Otherwise, the card will look like a regular Medicaid card.
How many Medicare cost sharing programs are there?
Medicare Cost-Sharing Programs. There are three Medicare cost-sharing programs for people with Part A Medicare. These programs help cover some of the member’s costs for Medicare services.
What is the QMB income limit?
Applicants must pass all the QMB rules except that they must be receiving Part A Medicare and their income exceeds 120% of the Federal Poverty Level but not more than 135% of the Federal Poverty Level and the individual cannot be receiving Medicaid. This is not an entitlement program.
How long does it take for Medicare to pay Social Security?
About three months after becoming eligible for a Medicare cost-sharing program, the state begins paying the Medicare Part B premium and the Social Security check will increase. However, members will be reimbursed by Social Security for each month of eligibility during which a Medicare premium was deducted from the person’s check.
Does the QI program have a guaranteed benefit?
When funds have been allocated for a calendar year, no new applicants will receive any benefits. Eligibility in future calendar years is not guaranteed. No card is issued for the QI program .
Does SLMB pay Medicare?
The SLMB program pays the Part B Medicare premium only. Part B Medicare covers a person’s physician care, and a variety of outpatient services including outpatient hospital services. Applicants must pass all the QMB rules, except that they must be receiving Part A coverage and their income exceeds 100% of the Federal Poverty Level and does not exceed 120% of the Federal Poverty Level. No card is issued for the SLMB program. An individual may be eligible for both Medicaid and SLMB.
Who is eligible for Medicaid in Utah?
Additionally, applicants eligible to receive Medicaid include children 18 years of age or younger and parents and caretaker relatives with dependent children. Other groups who may qualify for UT Medicaid benefits include certain refugees, foster children and some former foster children, among others. Procedures to qualify for Medicaid in Utah ...
How to apply for medicaid in Utah?
The application to qualify for Medicaid in Utah is available through several methods. Candidates can apply for Utah Medicaid benefits online, by fax or in person . While all required information is the same for all Medicaid application methods, there are slight differences between each method of application.
What is meeting Medicaid eligibility?
Meeting Medicaid benefits eligibility means applicants will receive coverage that includes a variety of medical expenses such as doctor visits and prescriptions. However, eligibility for Medicaid relies on a broad range of factors such as income levels, legal status in the country and age. Find out what are the requirements for Medicaid in UT by ...
What is FMAP in Medicaid?
The federal government provides states with funds based on Federal Medical Assistance Percentages (FMAP). The states administer the guidelines to qualify for Medicaid to potential beneficiaries and offer some additional funding. Meeting Medicaid benefits eligibility means applicants will receive coverage that includes a variety ...
What is the Department of Health of Utah?
The Utah Department of Health manages Medicaid eligibility requirements in Utah by overseeing the Medicaid application process, determining eligibility and reviewing petitions. Determining eligibility for Medicaid first begins with the particular situation of a potential beneficiary.
Can non-citizens get medicaid in UT?
Non-citizens must provide officials with proof of legal status, which includes any relevant documents. For both citizens and legal immigrants, qualifying for Medicaid in UT requires proof of residency in the state with documents such as utility bills. To learn more about applying for Medicaid, download our free guide today.
Who Are The Dual-Eligible Recipients?
Medicare Ineligibility
- The Medicare eligibility requirement is that you must be 65 years old or older. If you or your spouse are 65 years old or older and have paid enough Medicare taxes through previous employment, you or your spouse may be eligible for premium-free Part A of the Medicare program (hospital coverage). They may also be eligible for Medicare Part B, covering doctor visits and var…
Medicaid Ineligibility
- Medicaid eligibility varies depending on where a person resides, as various states have different qualifications. Every year, Medicaid rules may change. The Federal Poverty Level (FPL), which the Department of Health and Human Services (HHS) determines every year, is used to determine a person’s eligibility for a variety of government benefits. In addition to the 48 contiguous states a…
Dual Eligibility
- A person must qualify for either partial-dual or full-dual coverage to be eligible for both Medicare and Medicaid. The amount of Medicaid assistance a person receives determines their eligibility for partial-dual coverage. The following are some examples of various coverage: 1. The premium for Part A (if applicable) 2. The premium for Part B 3. Coi...
Variations in Geography
- Medicaid benefits and coverage vary from one state to the next, and there are differences between them. Depending on the state, Medicaid coverage may be available to those who earn more than the standard income limits. The Medicaid website can assist a person in determining which services are available to them in their area based on their geographic location.
Medicare Part D Extra Assistance Program
- Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual. To be eligible for Extra Help, a person’s combined investments, real estate property, and savings must total no more than $29,1…
Summary
- A person’s health and income level may qualify them for both Medicare and Medicaid. Meanwhile, Medicare will generally cover healthcare costs initially, and Medicaid assists with out-of-pocket and non-covered expenses. Medicaid eligibility varies by state, as well as the income level restrictions.
Overview
Healthcare
Programs
Components
Risks
Qualification
Examples
Issues
Health
Benefits
- 2) Utah Aging Waiver for Individuals Age 65 or Older also referred to as the Aging Waiver, this home and community based services Medicaid waiver allows program participants to hire the caregiver of their choosing, including some relatives. Other benefits include adult day care, homemaker services, meal delivery, home modifications and more. 3) Ut...