What is the highest income to qualify for Medicaid?
Income requirements: To qualify for Medicaid via expansion, your MAGI can't exceed $1,784 per month for an individual and $2,413 per month for a two-person family.
What is the lowest income to qualify for Medicaid?
OverviewIncome Eligibility Criteria. A single individual, 65 years or older, must have income less than $2,523 / month. ... Asset Requirements. ... Level of Care Requirements. ... Nursing Home Eligibility. ... Assisted Living Eligibility. ... In-Home Care Eligibility. ... Options When Over the Income Limit. ... Options When Over the Asset Limit.More items...•Dec 6, 2021
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).Feb 11, 2022
How does Medicaid check income?
Documentation of income might include any of the following: Most current pay stubs, award letter for Social Security, SSI, Railroad Retirement, or VA, pension statement, alimony checks, dividend checks, a written statement from one's employer or from a family member who is providing support, or an income tax return.Mar 14, 2022
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How much does Medicare Part B cost?
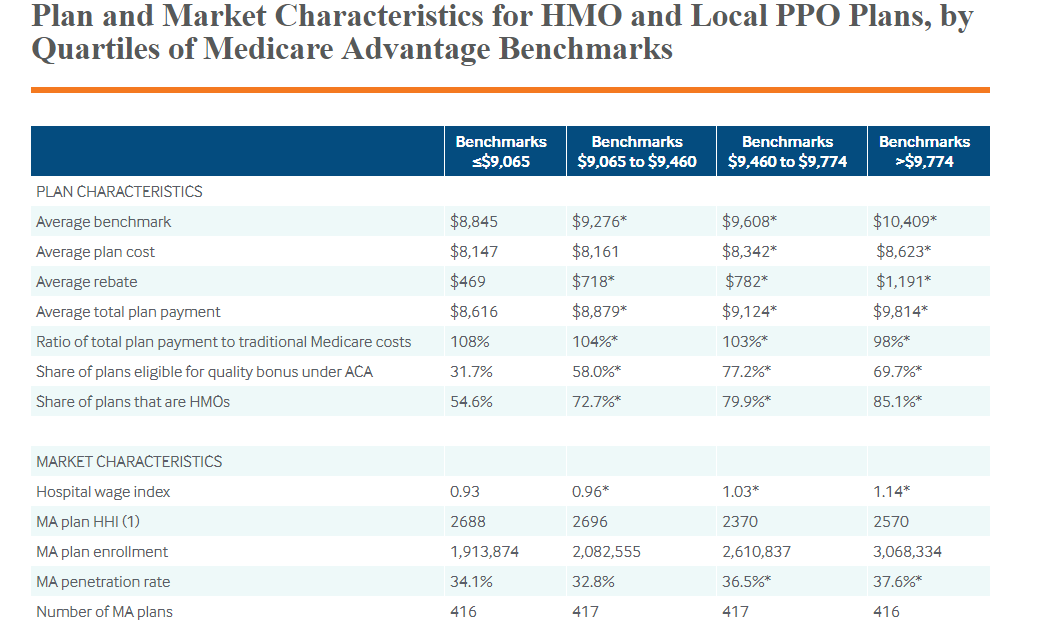
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
Who are the dual-eligible recipients?
People who are dual-eligible for Medicare and Medicaid are referred to as dual-eligible beneficiaries. Moreover, each state determines Medicaid coverage, and as a result, Medicaid benefits may differ.
Medicare Ineligibility
The Medicare eligibility requirement is that you must be 65 years old or older. If you or your spouse are 65 years old or older and have paid enough Medicare taxes through previous employment, you or your spouse may be eligible for premium-free Part A of the Medicare program (hospital coverage).
Medicaid Ineligibility
Medicaid eligibility varies depending on where a person resides, as various states have different qualifications.
Dual eligibility
A person must qualify for either partial-dual or full-dual coverage to be eligible for both Medicare and Medicaid.
Variations in geography
Medicaid benefits and coverage vary from one state to the next, and there are differences between them. Depending on the state, Medicaid coverage may be available to those who earn more than the standard income limits.
Medicare Part D Extra Assistance Program
Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual.
Summary
A person’s health and income level may qualify them for both Medicare and Medicaid.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).
Qualifying for Medicaid Explained
Caitlin McCormack Wrights has over a decade of experience writing hundreds of articles on all things finance. She specializes in insurance, mortgages, and investing and relishes making dull subject matter gripping and everyday topics amazing. Caitlin has a bachelor's from Duke and a master's from Princeton.
What Does Medicaid Cover?
Medicaid is a joint state and federal program that provides health care coverage to qualifying individuals. Anyone who meets the eligibility requirements has a right to enroll in Medicaid coverage. Although each state has its own Medicaid program, the federal government places rules that all states must follow.
Who Is Eligible for Medicaid?
Medicaid provides low-cost health coverage to qualifying individuals in different groups. People who meet the eligibility rules have a right to Medicaid coverage. Generally, your eligibility for Medicaid depends on one or a combination of the following factors:
State Expanded Medicaid Eligibility
As of August 2021, 38 states (plus the District of Columbia) had expanded Medicaid to cover all low-income adults whose household incomes are below a specified threshold. If your state has expanded Medicaid, you are eligible for coverage based on your income alone. Typically, your household income shouldn’t exceed 138% of the federal poverty level.
Appealing for Denial of Coverage
You’ll start receiving the appropriate Medicaid services if you meet all the requirements and are deemed financially eligible. If you don’t meet all the eligibility requirements, you will be notified of your right to a fair hearing.
Frequently Asked Questions (FAQs)
Medicaid eligibility is determined once every 12 months. You could lose benefits during the renewal process for failing to submit the required paperwork.
What percentage of Medicare beneficiaries are eligible for Medicaid?
Around 20 percent of Medicare beneficiaries are also eligible for Medicaid. They are called dual-eligible. You would need to apply for each one separately to determine if you can qualify for both. Dual-eligibles are categorized based on whether they receive full or partial Medicaid benefits.
How old do you have to be to get Medicare?
Since Medicare is a government insurance program, anyone aged 65 or older can apply and receive insurance through this program.
What is the difference between Medicare and Medicaid?
The benefit is the plan will have very low copays and very few additional fees. Medicare is for those aged 65 and older or those with disabilities or specific medical conditions. Medicaid is for people of any age, with or without medical conditions, so long as they meet the state’s economic conditions.
How are Medicare premiums paid?
Premiums are typically paid on a monthly basis. In the federal Medicare program, there are four different types of premiums. ... , deductibles, copays, and more. Medicaid assists with these costs, but you may be required to use an approved Medicaid health plan.
What percentage of Medicare is covered by deductible?
In fact, from the beginning, Medicare was designed to cover only about 80 percent of a beneficiary’s major medical expenses. All other costs, typically in the form of deductibles. A deductible is an amount a beneficiary must pay for their health care expenses before the health insurance policy begins to pay its share....
What is Medicare Part B?
If not, you will pay a monthly premium for Part A. With Part B. Medicare Part B is medical coverage for people with Original Medicare. It covers doctor visits, specialists, lab tests and diagnostics, and durable medical equipment. Part A is for hospital inpatient care....
How can low income people get help with prescriptions?
The first and most important way is to apply for the Social Security Administration’s Extra Help program . This program provides low-income subsidies (LIS) to those who need them.
For those who qualify, there are multiple ways to have your Medicare Part B premium paid
In 2022, the standard Medicare Part B monthly premium is $170.10. Beneficiaries also have a $233 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What is the Part B premium reduction benefit?
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.
How to find plans that offer the giveback benefit
Not all MA plans offer this benefit, so you must find a plan that does in order to take advantage of the opportunity. In 2022, these plans are offered in nearly all states, so you may find one close to you.
Other Part B reimbursement options
There are other ways you can lower or eliminate how much you pay for the Medicare Part B premium. This includes certain Medicaid programs or benefits from some retiree health plans.
Determining Eligibility For Medicaid
- Financial Eligibility
The Affordable Care Act established a new methodology for determining income eligibility for Medicaid, which is based on Modified Adjusted Gross Income (MAGI). MAGI is used to determine financial eligibility for Medicaid, CHIP, and premium tax credits and cost sharing reductions avail… - Non-Financial Eligibility
To be eligible for Medicaid, individuals must also meet certain non-financial eligibility criteria. Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, suc…
Medically Needy
- States have the option to establish a “medically needy program” for individuals with significant health needs whose income is too high to otherwise qualify for Medicaid under other eligibility groups. Medically needy individuals can still become eligible by “spending down” the amount of income that is above a state's medically needy income standard. Individuals spend down by incu…
Appeals
- States must provide individuals the opportunity to request a fair hearing regarding a denial, an action taken by the state agency that he or she believes was erroneous, or if the state has not acted with reasonable promptness. States have options for how to structure their appeals processes. Appeals may be conducted by the Medicaid agency or delegated to the Exchange or …
Related Topics
- Spousal Impoverishment: Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services. Treatment of Trusts: When an individual, his or her s…