- Log into or create your online Medicare account.
- Select "Get Your Medicare Summary Notices (MSNs) electronically" under the "My Messages" section at the top of your...
- You'll reach the "My Communication Preferences" page. Select "Yes" under "Change eMSN Preference."
Full Answer
How long to keep Medicare summary notices?
Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance. How long you keep these records depends on your personal preference.
How to understand Medicare summary notices?
What should I do if I get this notice?
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
How to read your Medicare summary Notice (MSN)?
The Medicare Summary Notice
- Authenticity. An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself.
- Deductibles. Your deductible status will be listed in the left-hand column on Page 1. ...
- Claims. Page 1 of your Medicare Summary Notice lists a brief overview of "Your Claims & Costs This Period". ...
What is a concern about the future of Medicare?
The shift to pay for performance, with its additional burdens on providers to document quality outcomes, is what Norrell sees as the next major hurdle for Medicare. Tying in to that is the public's greatest concern: the future financial viability of Medicare.

Is Medicare Summary Notice same as Explanation of Benefits?
An Explanation of Benefits (EOB) is the notice that your Medicare Advantage Plan or Part D prescription drug plan typically sends you after you receive medical services or items. You only receive an EOB if you have Medicare Advantage or Part D. An EOB is not the same as a Medicare Summary Notice.
How do you read a Medicare EOB?
How to Read Medicare EOBsHow much the provider charged. This is usually listed under a column titled "billed" or "charges."How much Medicare allowed. Medicare has a specific allowance amount for every service. ... How much Medicare paid. ... How much was put toward patient responsibility.
What does the Medicare Summary Notice list?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period.
How do I read a Medicare Summary Notice?
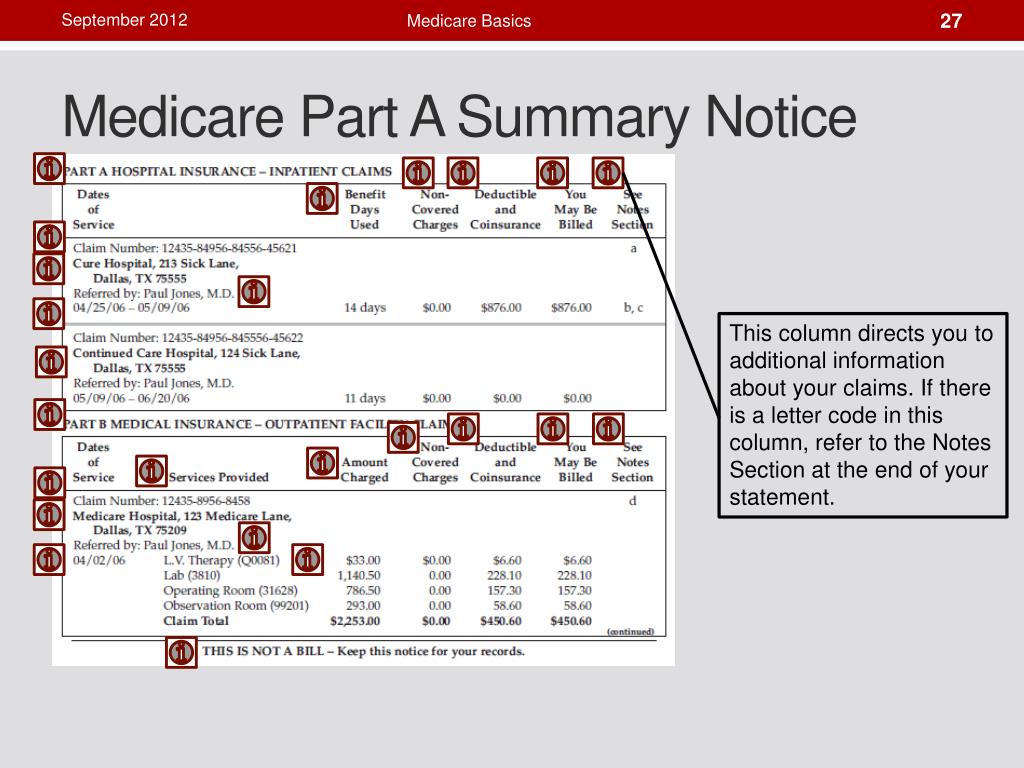
The Part A Medicare summary notice shows the dates of the claims, how much of the deductible you have met, whether Medicare approved all of the claims, and the total amount you may be billed from the facility. It also lists the facilities where you have had claims this period and the dates you received services there.
How does a patient read an EOB?
1:342:35How to Read Your Medical EOB - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe amount you pay for the service this is the amount that you will be billed. Remember the EOB isMoreThe amount you pay for the service this is the amount that you will be billed. Remember the EOB is not a bill it just shows you how the costs are distributed. If you have any questions by your EOB.
What is a summary of benefits and coverage?
An easy-to-read summary that lets you make apples-to-apples comparisons of costs and coverage between health plans. You can compare options based on price, benefits, and other features that may be important to you.
Is it necessary to keep Medicare summary notices?
There is no hard and fast rule for saving medical payment records. Certainly, they need to be kept while the medical services that are summarized on the forms are in the process of payment by Medicare and supplemental insurance policies.
Which is an easy to read monthly statement that clearly lists Medicare claims information?
The MSN is an easy‑to‑read statement that clearly lists your health insurance claims information. For more information on filing an appeal, visit Medicare.gov/appeals, or call 1‑800‑MEDICARE (1‑800‑633‑4227). TTY users can call 1‑877‑486‑2048.
How do providers check Medicare claim status?
Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
Why is my first Medicare bill so high?
If you're late signing up for Original Medicare (Medicare Parts A and B) and/or Medicare Part D, you may owe late enrollment penalties. This amount is added to your Medicare Premium Bill and may be why your first Medicare bill was higher than you expected.
Does everyone on Medicare have a deductible?
Summary: Medicare Part A and Part B have deductibles you may have to pay. Medicare Part C and Part D may or may not have deductibles, depending on the plan. Original Medicare has two parts: Part A for hospital insurance and Part B for medical insurance.
How do you meet your Medicare Part B deductible?
3:045:05How Do You Pay the Part B Deductible? - YouTubeYouTubeStart of suggested clipEnd of suggested clipBy sending 233 dollars to medicare. Itself you just pay the first 233. Dollars of your first part meMoreBy sending 233 dollars to medicare. Itself you just pay the first 233. Dollars of your first part me medical care in that year. This means you pay that deductible to a medical provider. And like i
What is the summary notice for Medicare?
This summary is in the right-hand column and lets you know if Medicare denied coverage for any services that quarter and how much you can expect to be billed. Page 3 provides a more detailed summary of each service and its charges.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is an ABN for Medicare?
The ABN is an acknowledgment that Medicare may not cover the service and that you are willing to pay out of pocket for the service. If you did sign an ABN, it is not valid if it is illegible, if it is signed after the service was performed, or if it is otherwise incomplete.
What is MSN bill?
An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself. THIS IS NOT A BILL will be printed in bold capitalized letters at the top of the statement.
How long does a deductible last for a nursing home?
It ends when you have not received inpatient hospital or skilled nursing facility care for 60 days in a row. You will pay a deductible for each benefit period and multiple deductibles may be listed here. In 2020, each deductible costs $1,408.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
Does Medicare cover limiting charges?
Medicare does not cover the limiting charge. Amount Medicare Paid: This lets you know the total amount Medicare paid for covered services. Medicare covers 80% of the cost for most services but will pay for 100% of costs for preventive care services if they are ordered by a participating provider.
What is the most important part of a Medicare notice?
Let’s talk a bit about the notes column. In our opinion, the footnotes are the most important part of the notice. Medicare is required to give an explanation for every claim that is denied, every charge you may be incurring. Each charge usually has one footnote, sometimes even more than that.
What is the gray box on Medicare Part A?
Under the gray box is your deductible status. Please do not get the deductibles for Medicare Part A and Part B confused. A deductible period for part A can happen multiple times in a year and is significantly higher than the Medicare Part B deductible.
What is a Medicare Part A deductible?
Remember the definition of deductible: this is the amount that someone must pay before Medicare pays its share.
What does "assigned claim" mean?
An assigned claim means a doctor has agreed to accept Medicare’s charges in full and may not bill you the difference. Please be aware this is not the same as the typical 20% amount owed. That may still be charged as it is part of the assignment-agreed upon amount. Under the top section are definitions.
Is Part A an annual period?
This is especially important under the Part A notice, because many people are unaware how Part A’s benefit period works. It is not an annual period. The last section on page two is a message from Medicare. Medicare typically has two or three advisories on each notice for you each time you get one.
Do Medicare Advantage members get notices?
Please note that Medicare Advantage members will NOT receive notices like these. If you have a Medicare Advantage plan and need help understanding your bills, it will be in your best interest to speak with your qualified insurance broker or a member of that company’s customer service team for assistance.
Introduction
If you are enrolled in Medicare, you should be receiving Medicare plan documents like the Medicare Explanation of Benefits (EOB) or Medicare Summary Notices (MSN) when you receive care or use your plan’s benefits.
What information is included in the Medicare EOB?
The Explanation of Benefits contains your plan’s description and claim-related details like:
What is the purpose of the Medicare EOB?
These Medicare plan documents help you save money and track fraud. Here’s how:
What should you expect to see in the MSN?
If you’re enrolled in Original Medicare, you will receive an MSN instead of an EOB. An MSN shows similar information to an EOB.
Conclusion
In summary, Medicare EOBs and MSNs are important notices to help you keep track of your healthcare expenses and what your insurance covers, amongst other things. They’re also important documents if you want to make a claim or contest a charge. Remember to keep these Medicare plan documents for at least one calendar year.
How often is Medicare mailed?
account. Each MSN includes instructions to file an appeal if one of your claims is denied. MSNs are mailed every three months if you’ve received any Medicare-covered services.
What is an MSN statement?
Medicare Summary Notices are detailed statements mailed by Medicare every three months. Your MSN will include your account’s claims, the doctors you visited, how much was paid, and more. An MSN is not a bill. Think of your MSNs as Medicare statements. As with your bank statements, you can use an MSN to verify that your account’s activity matches ...
Is Medicare a bill?
A Medicare Summary Notice (MSN) is not a bill. Original Medicare is a fee-for-service health insurance program available to Americans aged 65 and older and some individuals with disabilities. Original Medicare is provided by the federal government and is made up of two parts: Part A (hospital insurance) and Part B (medical insurance). account.
Is Medicare Supplement endorsed by the government?
Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. If you’re looking for the government’s Medicare site, please navigate to www.medicare.gov.
Does Medicare Advantage have an EOB?
Private health insurance companies provide Medicare Advantage and Part D plans, and each company creates its own EOB to send to its customers. That means an EOB from one company can look very different from another company’s EOB. MSNs, however, are all formatted the same way.