- Department of Health and Human Services (HHS) Office of Inspector General (OIG) Medicare fraud hotline at 1-800-HHS-TIPS
- Contact the HHS by mail at HHS Tips Hotline, PO Box 23489, Washington, DC 20026-348
- Centers for Medicare and Medicaid Services at 1-800-MEDICARE
- Contact CMS by mail at Medicare Beneficiary Contact Center, PO Box 39, Lawrence, KS 66044
- You can report it by calling the CMS report hotline or submit the information online.
How to report Medicare fraud?
Aug 08, 2021 · How To Report Medicare Fraud. Reporting Medicare fraud is as simple as making a phone call. If you know Medicare fraud, waste, or abuse that's happening, it’s vital that you report the incident. As citizens, it’s our job to be courageous and …
Which is considered Medicare fraud?
Contact: Provider fraud or abuse in Original Medicare (including a fraudulent claim, or a claim from a provider you didn’t get care from) 1-800-MEDICARE (1-800-663-4227) or. The U.S. Department of Health and Human Services – Office of the Inspector General.
What defines fraud, waste and abuse?
Aug 06, 2014 · How do I report fraud, waste or abuse of Medicare? To report suspected Medicare fraud, call toll free 1-800-HHS-TIPS (1-800-447-8477). Medicare fraud happens when Medicare is billed for services or supplies you never got.
What is Medicare fraud?
Medicare Fraud & Abuse: Prevent, Detect, Report. MLN Booklet ... Resources for reporting suspected fraud and abuse Help Fight Fraud by Reporting It The Office of Inspector General (OIG) Hotline accepts tips and complaints from all sources on potential fraud, waste, and abuse. View instructional videos about the .
What is considered Medicare abuse?
Medicare abuse includes practices that result in unnecessary costs to the Medicare program. Any activity that does not meet professionally recognized standards or provide patients with medically necessary services is considered abuse. Committing abuse is illegal and should be reported.
Which is an acceptable way to report potential fraud waste and abuse?
Report Fraud, Waste, and Abuse Just report any concerns to your compliance department or your sponsor's compliance department. Your sponsor's compliance department area will investigate and make the proper determination.
What are examples of Medicare fraud?
Additional examples of Medicare scams include: A person without Medicare coverage offering money or goods to a Medicare beneficiary in exchange for their Medicare number in order to use their Medicare benefits. A sales person offering a prescription drug plan that is not on Medicare's list of approved Part D plans.Dec 7, 2021
What are examples of fraud waste and abuse?
Examples of Fraud, Waste and AbuseBilling for services not rendered.Altering medical records.Use of unlicensed staff.Drug diversion (e.g. dispensing controlled substances with no legitimate medical purpose)Kickbacks and bribery.Providing unnecessary services to members.
What are two ways to report potential fraud waste and abuse?
How can I report fraud, waste, and abuse about an HHS program?Toll-free phone: 1-800-HHS-TIPS (1-800-447-8477), 8:00 am - 5:30 pm, Eastern Time, Monday-Friday.Fax: 1-800-223-8164 (10 pages or less, please)TTY: 1-800-377-4950.Mail: HHS TIPS Hotline. P.O. Box 23489. Washington, DC 20026.
What resources are available to report Medicare compliance fraud waste or abuse concerns?
National Benefit Integrity MEDIC website. Medicare Fraud website. For Medicare Managed Care or Prescription Drugs: 1-877-7SafeRx (1-877-772-3379)
What is the difference between fraud waste and abuse?
Fraud requires the person to have intent and obtain payment and knowledge that their actions are wrong. Waste and abuse may involve obtaining an improper payment, but does not require the same intent and knowledge.
What is the difference between healthcare fraud and abuse?
What is health care fraud and abuse? Fraud is an intentional deception or misrepresentation of fact that can result in unauthorized benefit or payment. Abuse means actions that are improper, inappropriate, outside acceptable standards of professional conduct or medically unnecessary.
What are some of the penalties for violating fraud waste and abuse FWA laws?
Penalties include fines up to $25,000, imprisonment for up to 5 years and exclusion from Federal Health Care Programs (e.g., Medicaid & Medicare).
Which of the following are examples that may constitute Medicare fraud waste or abuse?
Examples of actions that may constitute Medicare abuse include: • Billing for unnecessary medical services; • Billing for brand name drugs when generics are dispensed; • Charging excessively for services or supplies; and • Misusing codes on a claim, such as upcoding or unbundling codes.
What is the False Claims Act in healthcare?
The False Claim Act is a federal law that makes it a crime for any person or organization to knowingly make a false record or file a false claim regarding any federal health care program, which includes any plan or program that provides health benefits, whether directly, through insurance or otherwise, which is funded ...
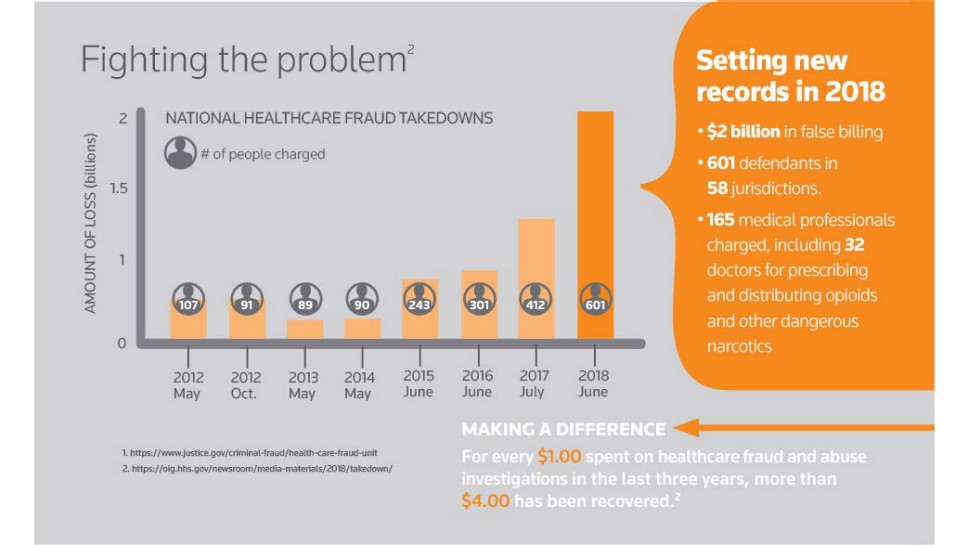
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
What is the OIG self disclosure protocol?
The OIG Provider Self-Disclosure Protocol is a vehicle for providers to voluntarily disclose self-discovered evidence of potential fraud. The protocol allows providers to work with the Government to avoid the costs and disruptions associated with a Government-directed investigation and civil or administrative litigation.
What does "knowingly submitting" mean?
Knowingly submitting, or causing to be submitted, false claims or making misrepresentations of fact to obtain a To learn about real-life cases of Federal health care payment for which no entitlement Medicare fraud and abuse and would otherwise existthe consequences for culprits,
What is the role of third party payers in healthcare?
The U.S. health care system relies heavily on third-party payers to pay the majority of medical bills on behalf of patients . When the Federal Government covers items or services rendered to Medicare and Medicaid beneficiaries, the Federal fraud and abuse laws apply. Many similar State fraud and abuse laws apply to your provision of care under state-financed programs and to private-pay patients.
What is the OIG?
The OIG protects the integrity of HHS’ programs and the health and welfare of program beneficiaries. The OIG operates through a nationwide network of audits, investigations, inspections, evaluations, and other related functions. The Inspector General is authorized to, among other things, exclude individuals and entities who engage in fraud or abuse from participation in all Federal health care programs, and to impose CMPs for certain violations.
What is the Stark Law?
Section 1395nn, often called the Stark Law, prohibits a physician from referring patients to receive “designated health services” payable by Medicare or Medicaid to an entity with which the physician or a member of the physician’s immediate family has a financial relationship , unless an exception applies.
What is the OIG exclusion statute?
Section 1320a-7, requires the OIG to exclude individuals and entities convicted of any of the following offenses from participation in all Federal health care programs:
What is the HHS OIG?
HHS-OIG has a long history of protecting the health and well-being of HHS beneficiaries, including residents in long-term care facilities such as nursing homes. HHS-OIG collects and investigates tips and complaints about fraud, waste, and abuse in these facilities.
What is the HHS?
HHS is the largest grant-making organization in the federal government, and its funding of health and human services programs touches the lives of almost all Americans. Fraud or misconduct related to the receipt or expenditure of HHS grants should be reported to our Hotline.
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
What is the OIG self disclosure protocol?
The OIG Provider Self-Disclosure Protocol is a vehicle for providers to voluntarily disclose self-discovered evidence of potential fraud. The protocol allows providers to work with the Government to avoid the costs and disruptions associated with a Government-directed investigation and civil or administrative litigation.
What is the role of third party payers in healthcare?
The U.S. health care system relies heavily on third-party payers to pay the majority of medical bills on behalf of patients . When the Federal Government covers items or services rendered to Medicare and Medicaid beneficiaries, the Federal fraud and abuse laws apply. Many similar State fraud and abuse laws apply to your provision of care under State-financed programs and to private-pay patients.
What is the OIG?
The OIG protects the integrity of HHS’ programs and the health and welfare of program beneficiaries. The OIG operates through a nationwide network of audits, investigations, inspections, evaluations, and other related functions. The Inspector General is authorized to, among other things, exclude individuals and entities who engage in fraud or abuse from participation in all Federal health care programs, and to impose CMPs for certain violations.
What is the Stark Law?
Section 1395nn, often called the Stark Law, prohibits a physician from referring patients to receive “designated health services” payable by Medicare or Medicaid to an entity with which the physician or a member of the physician’s immediate family has a financial relationship , unless an exception applies.
What is the OIG exclusion statute?
Section 1320a-7, requires the OIG to exclude individuals and entities convicted of any of the following offenses from participation in all Federal health care programs:
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
