Obtaining Conditional Payment Letter from Medicare
- Is your client a medicare recipient? In your initial meeting with your client ask them if they are a medicare recipient,...
- Initial Claim Call medicare personal injury department at 1-800-999-1118 to open the initial claim.
- Representation Fax a medicare representation letter and a signed medicare proof of representation...
Full Answer
How do you write a letter for payment received?
Tips for writing a letter for requesting payment
- Express gratitude for doing business with you
- Use courteous and sincere language
- Mention the urgency of the dues to be paid on time for account purposes
- Highlight details about the goods or services supplied
- Give details like reference numbers of the delivery
- Highlight the outstanding amount of money the customer has not paid
What is conditional payment?
• A conditional payment is a payment that Medicare makes. for services where another payer may be responsible. This. conditional payment is made so that the Medicare beneficiary won’t have to use their own money to pay the bill.
What term explains Medicare payments and denials?
Medicare denial code and Description A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service.
What is conditional billing?
ifyou are contractually obligated to accept an amount less than the total charges and higher than the payment received as your payment in full.
What is a Medicare conditional payment letter?
Conditional Payment Letter (CPL) A CPL provides information on items or services that Medicare paid conditionally and the BCRC has identified as being related to the pending claim.
What is a conditional payment notice?
conditional payment is made so that the Medicare beneficiary won't have to use their own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is secured.
When would Medicare make a conditional payment to a beneficiary?
MSP provisions allow conditional payments in certain situations when the primary payer has not paid or is not expected to pay within 120 days after receipt of the claim for specific items and/or services. Medicare makes these payments “on condition” that it will be reimbursed if it is shown another payer is primary.
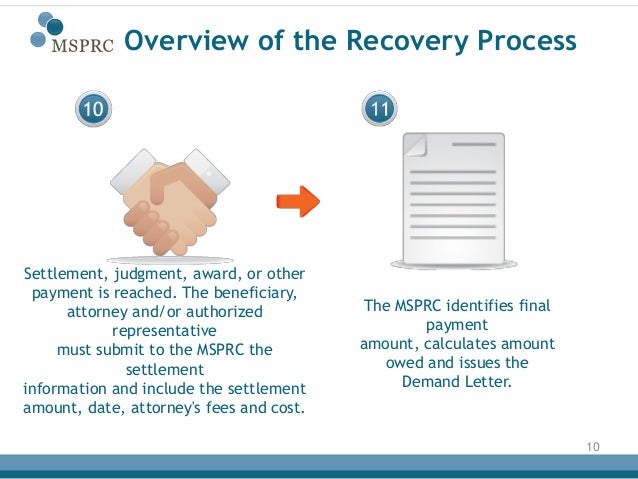
What is a demand letter from Medicare?
When the most recent search is completed and related claims are identified, the recovery contractor will issue a demand letter advising the debtor of the amount of money owed to the Medicare program and how to resolve the debt by repayment. The demand letter also includes information on administrative appeal rights.
Do I have to pay back conditional payments?
If you continue to certify for benefits while we review, you may have to pay back any conditional payments you received if we later find you ineligible.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
What letter sent to the beneficiary provides an interim estimate of conditional payments to date?
The CPL explains how to dispute any unrelated claims and includes the BCRC's best estimate, as of the date the letter is issued, of the amount Medicare should be reimbursed (i.e., the interim total conditional payment amount).
How does Medicare calculate final demand?
Step number two: take the gross settlement amount and subtract the total procurement cost to determine Medicare's final lien demand.
What is a Medicare release?
General. A “consent to release” document is used by an individual or entity who does not represent the Medicare beneficiary but is requesting information regarding the beneficiary's conditional payment information.
How long does Medicare have to recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
How do I get reimbursed from Medicare?
How to Get Reimbursed From Medicare. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out.
Can you negotiate Medicare liens?
This means that if you get a settlement, you will have to pay back Medicare before anything else gets taken out. While you can get the lien reduced, paying back Medicare after a settlement is not optional. The only path around a Medicare lien is to negotiate the lien to zero.
Initial Claim
Initial Claim Call medicare personal injury department at 1-800-999-1118 to open the initial claim.
Conditional Payment Letter
Conditional Payment Letter In 65 days you should receive a "conditional payment letter" which the insurance company will require in order to properly resolve your claim.