Section 1 – PATIENT INFORMATION.
- Print your name as shown on your Medicare card (Last Name, First Name, Middle Name)
- Print your Medicare Number exactly as it is shown on the Medicare card.
- Print your date of birth (mm/dd/yyyy)
- Check the appropriate box for the patient’s sex.
- Furnish your mailing address and include your telephone number.
How to file a Medicare claim?
How to file a Medicare claim. 1. Fill out a Patient’s Request for Medical Payment form. . You can also pick up a form at your local Social Security office. Instructions are included with the form. 2. Get an itemized bill for your medical treatment. Your itemized bill is the evidence for the Medicare claim.
Where to file Medicare claims?
- Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. ...
- View the Electronic Filing Instructions
- Palmetto GBA Interactive CMS-1500 Claim Form Instructions — This resource can also be helpful to providers who submit electronic claims. ...
How to bill Medicare?
Nowinski and the surgical centers billed Medicare and the Ohio Bureau of Workers' Compensation for the services. The settlement calls for OrthoNeuro to pay $498,182 to Medicare and $533,482 to BWC; the New Albany Surgery Center to pay $772,650 to Medicare and $468,406 to BWC; and Mount Carmel to pay $760,901 to Medicare and $156,139 to BWC.
Are you eligible for a Medicare reimbursement?
Only the member or a Qualified Surviving Spouse/Domestic Partner enrolled in Parts A and B is eligible for Medicare Part B premium reimbursement. 4. I received a letter stating that I pay a higher Part B premium based on my income level (Income-Related Monthly Adjustment Amount, i.e., IRMAA).

How long does it take to get paid by Medicare?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
Can I submit a claim to Medicare myself?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Does Medicare reimburse patients directly?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
How do I check my Medicare billing?
Visiting MyMedicare.gov. Calling 1-800-MEDICARE (1-800-633-4227) and using the automated phone system. TTY users can call 1-877-486-2048 and ask a customer service representative for this information. If your health care provider files the claim electronically, it takes about 3 days to show up in Medicare's system.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
How do I claim medical reimbursement?
How to claim Medical reimbursement? One can claim reimbursement of medical expenses by submitting the original bills to the employer. The employer would accordingly reimburse such expenses incurred subject to the overall limit of Rs 15,000 without tax deduction.
How much is Medicare reimbursement?
The rate at which Medicare reimburses health care providers is generally less than the amount billed or the amount that a private insurance company might pay. According to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill.
How do I claim Medicare online?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov pin. On your homepage, select Make a claim. Make sure you have details of the service, cost and amount paid to continue your claim.
When should I receive my Medicare bill?
Medicare bills usually arrive on or around the 10th day of the month. The bill will list the dates for which a person is paying, which is usually a 1-month period for Part A and Part D but a 3-month period for Part B. Medicare must receive payment by the 25th day of the month.
Can I view my Medicare account online?
Medicare's Blue Button is an online tool you can use to access your health information securely. You can decide to share that information with your doctors, loved ones, or anyone else of your choosing. It's available on the MyMedicare.gov site, which helps you keep track of your Medicare claims, and more.
Can I view my Medicare bill online?
You can find more information at Medicare.gov or CMS's online bill pay webpage. Remember, CMS does not charge a fee for processing the electronic payments, but in some situations, a bank may charge their customers a fee for using their online bill payment service.
How to contact Medicare Solutions?
Just call us toll-free at 855-350-8101 and we’ll guide you through the Medicare reimbursement process. We can also help you find the right plan for your unique needs.
How to file a claim for reimbursement?
To file a claim for reimbursement, you need to submit the proper form and backup documentation. First, download the Patient’s Request for Medical Payment form from the Centers for Medicare and Medicaid Services (CMS).
How Are Providers Reimbursed for Their Services?
If your provider (doctor, nurse, lab, etc.) accepts assignment, Medicare pays them for any covered services. That’s what “ accepts assignment ” means. It is an agreement between your provider and Medicare. The provider agrees to accept the Medicare-approved amount for the service and Medicare agrees to pay for the service.
What Do You Pay When Your Provider Accepts Assignment?
Providers who accept assignment agree to charge only the amount Medicare approves for a particular service. In other words, if the provider normally charges $150 for a service, but Medicare sets the rate at $100, the provider cannot charge more than $100.
How to find Medicare contractor?
Send both documents to the appropriate Medicare contractor. Choose your state from the Contractor Directory on this page. You can also call 1-800-MEDICARE if you need help finding the correct Medicare contractor.
Does Medicare bill supplement insurance?
The provider bills Medicare directly. Once they receive payment, they then bill for the remainder (deductibles and coinsurance). If you have Original Medicare and a Medigap plan, your supplement insurance is next on the list. If you do not have a Medigap plan, or if the service is not covered by Medicare, the provider sends you the bill.
Does Medicare Advantage have a pharmacy network?
Most Medicare Advantage plans have a provider network. Part D plans may also have a pharmacy network. Obtaining services from a provider outside your plan’s network typically means you are responsible for 100 percent of the cost of those services. If you receive care from an out-of-network provider and your claim is denied, you should contact your plan, not Medicare. In these instances, coverage is typically granted only if you required emergency care.
Where Do You Submit Medicare Payment Claims?
As a patient, you should mail your completed form, your itemized bill, and any supporting documents to your state’s Medicare Administrative Contractor (MAC). You can find the address on the chart included on the last twelve pages of the form. You’ll need to find the address that best corresponds with both:
What is Medicare number?
Your Medicare number. A description of the illness, injury or service for which you received treatment. An itemized bill. If applicable, you’ll also need to provide information about any health insurance coverage you have outside of Medicare, including a policy number.
What Information Do You Need to Fill Out This Form?
Medicare will need you to fill out a patient request form with some basic information about yourself as well as the service or medical item you are filing about. You’ll need to provide:
How long does it take for Medicare to pay for a ship?
The ship is in a U.S. port or within 6 hours of the ship arriving or departing from a U.S. port. If the ship is further than 6 hours from a U.S. port and you receive medical care while on it, Medicare will not pay for the services. If you’re filing a claim to get reimbursement for shipboard services, you must also include a copy ...
How long does it take to file a Medicare claim?
Before you take action, you should first ask your doctor or healthcare supplier to file the claim. They have up to 12 months to do so. Nevertheless, if it’s close to the end of that timeframe and your doctor still hasn’t complied, you may need to file the claim yourself. To do that, you’ll need to fill out and mail a Medicare Patient’s Request ...
What is the NPI on a medical bill?
The name and address of your doctor or healthcare provider, as well as their National Provider Identifier (NPI), if known. Since bills often list more than one doctor or provider, you should circle or highlight the appropriate name to make it easier for your claim to be processed.
What is a treatment?
A description of the illness, injury or service for which you received treatment
How to sign up for Medicare online?
Log in or create your secure Medicare account — Select "My Premiums" and then "Sign Up" to complete a short, online form.
How long does it take to get Medicare Easy Pay?
Mail your completed form to: It can take up to 6-8 weeks for your automatic deductions to start. Until your automatic deductions start, you'll need to pay your premiums another way. If you can't process your Medicare Easy Pay request, we'll send you a letter explaining why.
How do I change bank accounts or stop Medicare Easy Pay?
Log into your secure Medicare account — Select "My Premiums" and then "See or change my Medicare Easy Pay" to complete a short, online form.
What is Medicare Easy Pay?
Medicare Easy Pay is a free way to set up recurring payments for your Medicare premium. If you sign up for Medicare Easy Pay, your Medicare premiums will be automatically deducted from your checking or savings account each month. If you get a "Medicare Premium Bill" (Form CMS-500) from Medicare, you can sign up for Medicare Easy Pay.
When will Medicare Easy Pay deduct premiums?
We'll deduct your premium from your bank account on or around the 20th of the month.
How long does it take to get Medicare if you change your bank account?
If you stop Medicare Easy Pay: It can take up to 4 weeks for your automatic deductions to stop.
How to mail Medicare claim form?
Send the completed form and supporting documentation to your Medicare contractor. Reference the Medicare Administrative Contractor Address table for the correct address to mail your claim form. If you still do not know the address of your Medicare contractor, call 1-800-MEDICARE (1-800-633-4227). TTY users should call 1-877-486-2048.
What is the number to call for Medicare?
If a physician or supplier furnishes Medicare covered services to you and refuses to submit a claim on your behalf for those services, please call 1-800-MEDICARE (1-800-633-4227) in order to file a complaint with the Medicare contractor. TTY users should call 1-877-486-2048.
What is the authority to collect Medicare information?
COLLECTION AND USE OF MEDICARE INFORMATION. We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205 (a), 1872 and 1875 of the Social Security Act, as amended.
How long does it take for Medicare to process a claim?
Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
What happens if you submit a claim to Medicare?
If the claim form has incomplete or invalid information, the Medicare contractor will return the claim along with a letter to you clearly stating what information is missing or invalid.
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
How long does it take to file a Medicare claim?
Physicians and other suppliers, such as clinical laboratories, imaging service suppliers, and durable medical equipment suppliers are required by law to submit a claim for Medicare covered services furnished to you, the Medicare beneficiary, within one year of the date of service.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What is Medicare Reimbursement?
If you’re on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
What if my doctor doesn't bill Medicare?
If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.
How to get reimbursement for health insurance?
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand. The form asks for information about you, your claim, and other health insurance you have.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
How to mail Medicare claim form?
Send the completed form and supporting documentation to your Medicare contractor. Reference the Medicare Administrative Contractor Address table for the correct address to mail your claim form. If you still do not know the address of your Medicare contractor, call 1-800-MEDICARE (1-800-633-4227). TTY users should call 1-877-486-2048.
How long does it take for Medicare to process a claim?
Include a copy of the itemized bill and any supporting documents. Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request. Reference the Medicare Administrative Contractor Address Table for the correct address to mail your claim form. Medicare will not process a beneficiary request for payment for diabetic test strips, Part B drugs, or for items paid for under the DMEPOS Competitive Bidding program.
What is the authority to collect Medicare information?
We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205(a), 1872 and 1875 of the Social Security Act, as amended.
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
What to do if you can't sign your name on Medicare?
If you cannot sign your name, mark an (X) on the signature line. Have a witness sign his/her name next to the “X” and complete the section below. If signing this form on behalf of a Medicare patient, on the ‘Signature of Patient’ line above, indicate the patient’s name followed by “By” and sign your name. Provide your name, address, and relationship to the patient with a brief explanation why the patient cannot sign.
What does it mean when a provider refuses to file a claim for Medicare covered services?
The provider or supplier refused to file a claim for Medicare Covered Services The provider or supplier is unable to file a claim for the Medicare Covered Services The provider or supplier is not enrolled with Medicare
Can a physician submit a Medicare claim?
In most situations, your physician, other practitioner or supplier will submit your claim to Medicare, if they do not , you can submit a claim.
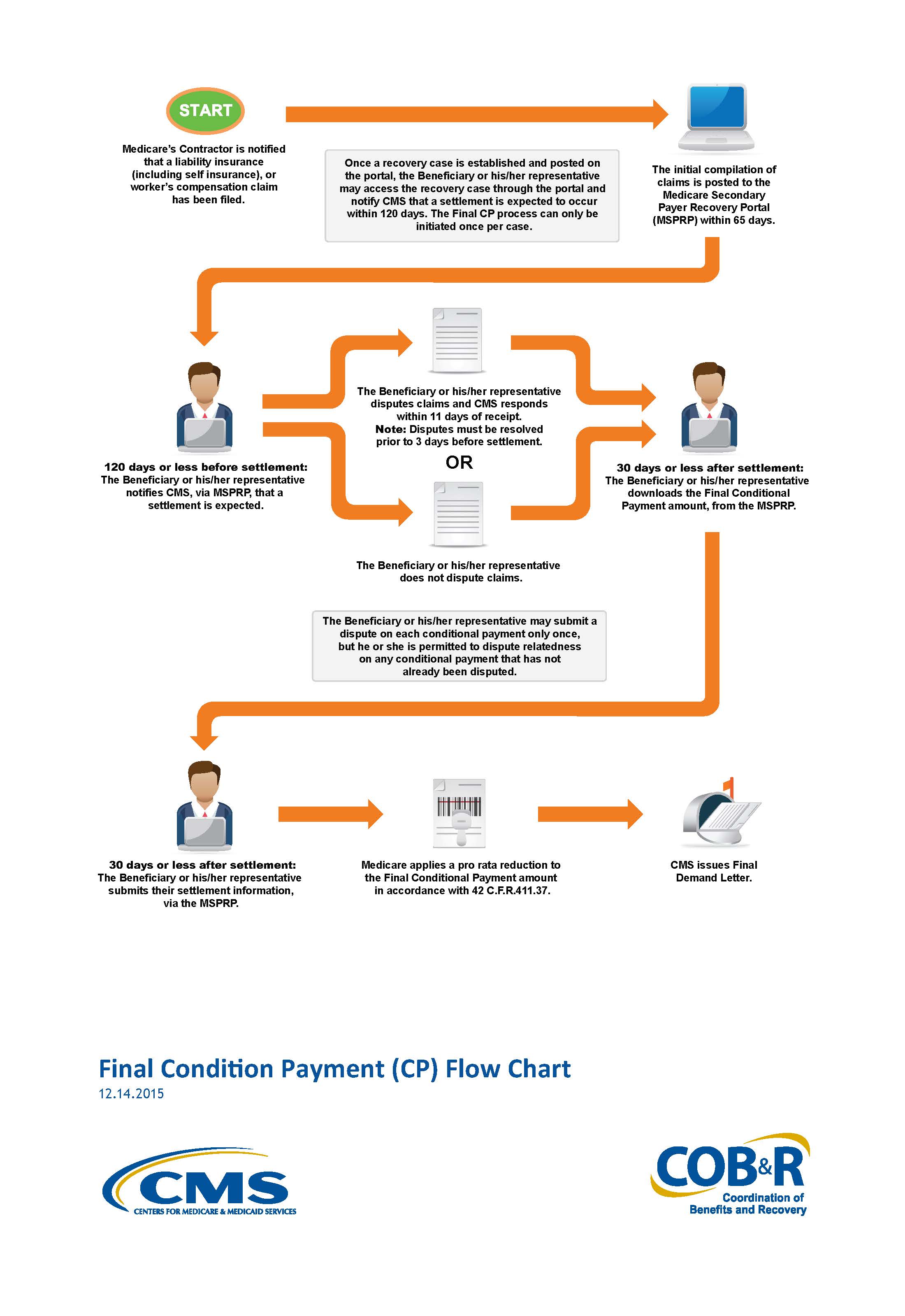
How to get conditional payment information?
You can obtain the current conditional payment amount and copies of CPLs from the BCRC or from the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627. To obtain conditional payment information from the MSPRP, see the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below. If a settlement, judgment, award, or other payment occurs, it should be reported to the BCRC as soon as possible so the BCRC can identify any new, related claims that have been paid since the last time the CPL was issued.
How to remove CPL from Medicare?
If the beneficiary or his or her attorney or other representative believes any claims included on the CPL or CPN should be removed from Medicare's conditional payment amount , documentation supporting that position must be sent to the BCRC. The documentation provided should establish that the claims are not related to what was claimed or were released by the beneficiary. This process can be handled via mail, fax, or the MSPRP. See the “Medicare Secondary Payer Recovery Portal (MSPRP)” section below for additional details. The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
What does BCRC do with conditional payment?
The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
What is a CPL for Medicare?
A CPL provides information on items or services that Medicare paid conditionally and the BCRC has identified as being related to the pending claim. For cases where Medicare is pursuing recovery from the beneficiary, a CPL is automatically sent to the beneficiary within 65 days of issuance of the Rights and Responsibilities letter (a copy of the Rights and Responsibilities letter can be obtained by clicking the Medicare's Recovery Process link). All entities that have a verified Proof of Representation or Consent to Release authorization on file with the BCRC for the case will receive a copy of the CPL. Please refer to the Proof of Representation and Consent to Release page for more information on these topics. The CPL includes a Payment Summary Form that lists all items or services the BCRC has identified as being related to the pending claim. The letter includes the interim total conditional payment amount and explains how to dispute any unrelated claims. The total conditional payment amount is considered interim as Medicare might make additional payments while the beneficiary’s claim is pending.
How long does a CPN take to respond to a judgment?
After the CPN has been issued, the recipient is allowed 30 days to respond.
How long does it take to get a demand letter from a court?
If a response is received within 30 calendar days, the correspondence will be reviewed, and a demand letter will be issued. If a response is not received in 30 calendar days, a demand letter will automatically be issued requesting repayment on all conditional payments related to the case without a proportionate reduction for fees or costs.
What is settlement documentation?
Proof of any items and/or services that are not related to the case , if applicable. All settlement documentation if you are providing proof of any items and/or services not related to the case. Procurement costs and fees paid by the beneficiary. Documentation for any additional or pending settlements, judgments, awards, ...
What happens if Medicare overpayment exceeds regulation?
Medicare overpayment exceeds regulation and statute properly payable amounts. When Medicare identifies an overpayment, the amount becomes a debt you owe the federal government. Federal law requires we recover all identified overpayments.
Where do we refer overpayments to?
We refer the overpayment debt to the Treasury or to a Treasury-designated Debt Collection Center (DCC). Both work through the
What is SSA 1893(f)(2)(A)?
SSA Section 1893(f)(2)(A) outlines Medicare overpayment recoupment limitations. When CMS and MACs get a valid first- or second-level overpayment appeal , subject to certain limitations , we can’t recoup the overpayment until there’s an appeal decision. This affects recoupment timeframes. Get more information about which overpayments we subject to recoupment limitation at
What is reasonable diligence in Medicare?
Through reasonable diligence, you or a staff member identify receipt of an overpayment and quantify the amount. According to SSA Section 1128J(d), you must report and return a self-identified overpayment to Medicare within:
How long does it take to get an ITR letter?
If you fail to pay in full, you get an ITR letter 60–90 days after the initial demand letter. The ITR letter advises you to refund the overpayment or establish an ERS. If you don’t comply, your MAC refers the debt for collection.
What is an overpayment?
An overpayment is a payment made to a provider exceeding amounts due and payable according to existing laws and regulations. Identified overpayments are debts owed to the federal government. Laws and regulations require CMS recover overpayments. This fact sheet describes the overpayment collection process.
When must you file a redetermination?
When requesting a redetermination on an overpayment subject to the Recoupment Limitation provision, you must file the redetermination by Day 30 from the demand letter date to prevent recoupment on Day 41. If you file an appeal after Day 30 and by Day 120, the law requires your MAC to stop recoupment
