
How do I submit Medicare Part D pharmacy claims?
Jul 24, 2021 · If you have to submit your own Medigap claim, you’ll need to at least send the insurer a Medicare summary notice (MSN) showing the payment Medicare made, and you may need to provide other documentation, such as an invoice or receipt. You don’t have to submit an MSN when filing claims for Medigap services that aren’t covered by Original Medicare (e.g. …
How do I file a Medicare claim for my doctor?
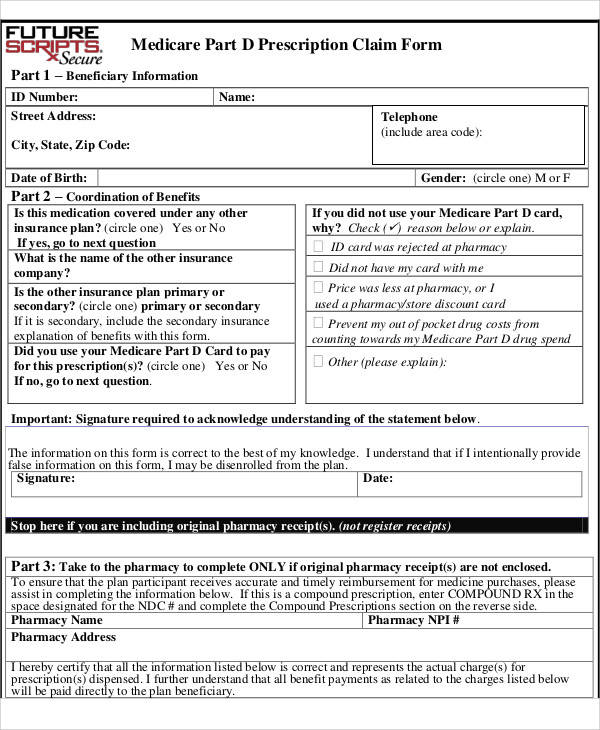
May 01, 2014 · To submit claims, beneficiaries should call their Part D plan and request an out-of-network pharmacy claim form as soon as they are able, and should check their Part D Evidence of Coverage for any applicable deadlines. The Centers for Medicare and Medicaid Services has provided Part D plans with a model claim form for this purpose.
Can I submit my own Medicare claims?
Here's how: Download and fill out a claim form. You’ll need to pick the form that goes with your plan. You’ll see separate forms for medical services and prescription drugs. Attach your original receipts to the claim form. Each form will have specific instructions about what your receipts should include and how to attach them to the form.
How do I request a Medicare redetermination from a company?
Feb 08, 2022 · To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor. What the Medicare Provider Bill Must Include the date you received service the place you received service
Can you submit your own claims to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
How does Medicare Part D reimbursement work?
The monthly premium paid by enrollees is set to cover 25.5% of the cost of standard drug coverage. Medicare subsidizes the remaining 74.5%, based on bids submitted by plans for their expected benefit payments.Oct 13, 2021
Can claims be mailed to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form.Jan 1, 2022
What form is used to send claims to Medicare?
CMS-1500Claim Form (CMS-1500) and Instructions The CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
How are Medicare Part D premiums paid?
No. To be enrolled on Part D, you must enroll through one of the prescription drug companies that offers the Medicare Part D plan or directly through Medicare at www.Medicare.gov. You can pay premiums directly to the company, set up a bank draft, or have the monthly premium deducted from your Social Security check.
What is the cost of Medicare Part D for 2021?
Premiums vary by plan and by geographic region (and the state where you live can also affect your Part D costs) but the average monthly cost of a stand-alone prescription drug plan (PDP) with enhanced benefits is about $44/month in 2021, while the average cost of a basic benefit PDP is about $32/month.
What is the mailing address for Medicare claims?
State Specific ExceptionsCorrespondenceUSPSMedical Review (Including Requested Post Pay Claims)Noridian JE Part B Attn: Medical Review PO Box 6783 Fargo ND 58108-6783PWK (paperwork)Noridian JE Part B Attn: PWK PO Box 6783 Fargo ND 58108-6783RefundsNoridian JE Part B Attn: Refunds PO Box 511381 Los Angeles CA 90051-79369 more rows•Jan 7, 2022
How do I submit a claim to paper?
When you have to submit a claim on paper, follow these guidelines:Use only original claim forms (the ones printed in red). ... If you need to write on the claim for any reason, use blue or black ink. ... Do not submit totally handwritten claims.Make sure that the print on the claims is dark.More items...•Mar 26, 2016
Who submits Medicare Part A claims?
Overview. Your Medicare Part A and B claims are submitted directly to Medicare by your providers (doctors, hospitals, labs, suppliers, etc.). Medicare takes approximately 30 days to process each claim.
What is the first step in processing the claim?
Your insurance claim, step-by-stepConnect with your broker. Your broker is your primary contact when it comes to your insurance policy – they should understand your situation and how to proceed. ... Claim investigation begins. ... Your policy is reviewed. ... Damage evaluation is conducted. ... Payment is arranged.
What is the first step in completing a claim form?
What is the first step in completing a claim form? Check for a photocopy of the patient's insurance card. Which carriers will accept physicians' typed name and credentials as an indication of their signature? Which form is also known as the UB- 40 form?
What is a 1500 form?
The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of ...Dec 1, 2021
What is a Medicare claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hos...
Who files Medicare claims?
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nur...
When do I need to file Medicare claim?
Original Medicare has both participating and non-participating providers. Participating providers accept Medicare’s reimbursement plus your coinsur...
How long do I have to file a claim?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for w...
What should I do if my provider doesn’t file my claim?
Before receiving care, ask your provider’s office whether they will submit your bill to Original Medicare. While they aren’t required to do so, som...
Are claim filing requirements different if I have Medicare Advantage or Medigap?
If you have Medicare Advantage, providers in the plan’s network have to bill your insurer for your care. As mentioned above, you may have to submit...
What if I’ve already paid for my care?
You may have already paid in full for your care when you filed your claim. Be sure to note that you’ve paid on your submission, so Medicare or your...
Do I need to file Part D claims?
Medicare Part D plans contract with pharmacies where you can fill your prescriptions. Both preferred and non-preferred pharmacies can bill your Par...
How do I check on my claim to make sure it was processed?
Original Medicare beneficiaries should receive an MSN every three months detailing their recent Medicare claims. Medicare Advantage and Part D enro...
How should I ensure my claims are also filed with Medicaid?
Many Medicare beneficiaries also qualify for Medicaid due to having limited incomes and resources. Medicaid pays for Medicare co-pays, deductibles...
How to file an original Medicare claim?
You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice ...
How long does it take to submit a claim to Medicare?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
What is Medicare claim?
What is a Medicare claim? A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hospital. If you have a Medicare Advantage or Part D plan, your insurer will process claims on Medicare’s behalf.
Do you have to bill your insurance if you have Medicare Advantage?
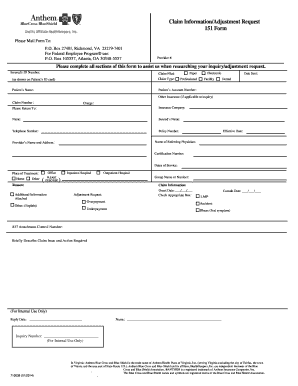
If you have Medicare Advantage, providers in the plan’s network have to bill your insurer for your care. As mentioned above, you may have to submit your own claims if you go out-of-network. If you decide to file a claim yourself, first contact your insurer for its claims mailing address and any forms to include with your claim.
Do you have to give advance beneficiary notice to Medicare?
Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice (ABN), Home Health Advance Beneficiary Notice, or Skilled Nursing Advance Beneficiary Notice if they believe Medicare will not cover your care. Providers normally will not bill Medicare after they issue an ABN.
Do you have to file a claim for hospice?
You should never have to submit claims for Part A services such as hospital, skilled nursing facility (SNF) or hospice care. When it comes to outpatient care, some providers will not file claims. This can happen if you have Original Medicare and see a non-participating provider, or if you have Medicare Advantage and visit an out-of-network doctor.
Do non-participating providers have to file claims with Medicare?
Non-participating providers can charge you up to 115 percent of Medicare’s rate (in most states) and don’t have to file claims with Medicare, although some choose to do so.
What is Medicare Part B?
When a patient is in outpatient observation status at a hospital, Medicare Part B is billed, and pays for, 80% of the hospital services provided (Part A pays for inpatient hospital admissions). However, outpatient prescription drugs received in the hospital while a patient is in observation status are not billed to Part B.
Do individual plans have different forms?
However, individual plans will likely have different forms . Beneficiaries should submit the completed claim form supplied by their plan and include the bill for medications from the hospital as well as a letter explaining that they were in observation status at the hospital and could not get to an in-network pharmacy.
Can you get outpatient drugs from a pharmacy?
In essence, patients in observation status at a hospital cannot be expected to get their outpatient drugs from a pharmacy that contracts with their Part D plan (like a CVS or Walgreens). Rather, they must take the drugs given to them by the hospital, dispensed from the hospital's out-of-network pharmacy. To submit claims, beneficiaries should call ...
How Do I File a Medicare Reimbursement Claim?
To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor.
What To Submit With The Claim
When filling out the form, you must choose the service type then provide the following information:
Where to Send Your Medicare Claim
Each state has a different address to send your claim. There are two places where you can find the address. You can find the address on the claim form on page two, or on your quarterly Medicare Summary Notice.
What if My Healthcare Provider is Not Sending the Claims Promptly?
The first thing you should do is call the provider and ask them to send your claim. If they do not file the claim, call Medicare and find out how much time is left to file the claim. If it’s close to the end of the allowed time and your healthcare provider has not filed the claim, you should go ahead and file the claim.
FAQs
When a claim is submitted to Medicare, it should come straight from the doctor or other provider of services. If for some reason they don’t submit the claim on your behalf, then you can call Medicare and submit it yourself. You can also submit the claim online.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you didn't get your prescription yet?
If you didn't get the prescription yet, you or your prescriber can ask for an expedited (fast) request. Your request will be expedited if your plan determines, or your prescriber tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…