Electronic process:
- Corrected claims can be submitted electronically as an EDI 837 transaction with the appropriate frequency code. ...
- Check Claims on Link to resubmit corrected claims that have been paid or denied.
- If you received a letter asking for additional information, submit it using Claims on Link.
Full Answer
How to resubmit rejected claims?
10 - Reopenings and Revisions of Claim Determinations and Decisions - General . 10.1 - Authority to Conduct a Reopening . 10.2 - Refusal to Reopen is Not an Initial Determination . 10.3 - Reopening of Denials Based on an Unanswered ADR Request . 10.4 - Reopenings Based on Clerical or Minor Errors and Omissions . 10.4.1 - Providers Submitting Adjustments
Does Medicare accept corrected claim?
Apr 13, 2021 · Attach a cover letter Circle or highlight any part of the claim form (for providers who are eligible to submit a paper claim form) Make any extraneous statements such as “corrected,” “second request,” etc. on the claim or documentation (this includes EDI submissions; do not add extraneous statements in the narrative)
What if Medicare denies my claim?
to submit paper request or phone calls Quickest route to correct claim(s) that contained errors and faster way of receiving reimbursements 14 Part B TRU Changes Adding or changing order/referring/supervising physician Add/change rendering provider Assignment of claims (contractor errors only) CLIA certification denials
What to do if Medicare denies your medical claim?
May 15, 2021 · Check your local Medicare provider website they will explain how to send for a correction of claim. I recommend you register for online access to your Medicare provider portal. This will allow you to submit all information and or request on line skiboi SharonCollachi True Blue Messages 2,173 Location Clovis, CA Best answers 3 May 14, 2021 #3
How do I submit a corrected claim to Medicare?
To submit a corrected claim to Medicare make the correction and resubmit as a regular claim (Claim Type is Default) and Medicare will process it.Hover over Billing and choose Live Claims Feed.Enter the patient's name or chart ID in the Patient field and click Update Filter.More items...•Jan 5, 2022
What is the timely filing for corrected claim for Medicare?
12 monthsMedicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.Jan 6, 2022
What is the submission code for a corrected claim?
7Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.Apr 8, 2015
How far back can you file Medicare claims?
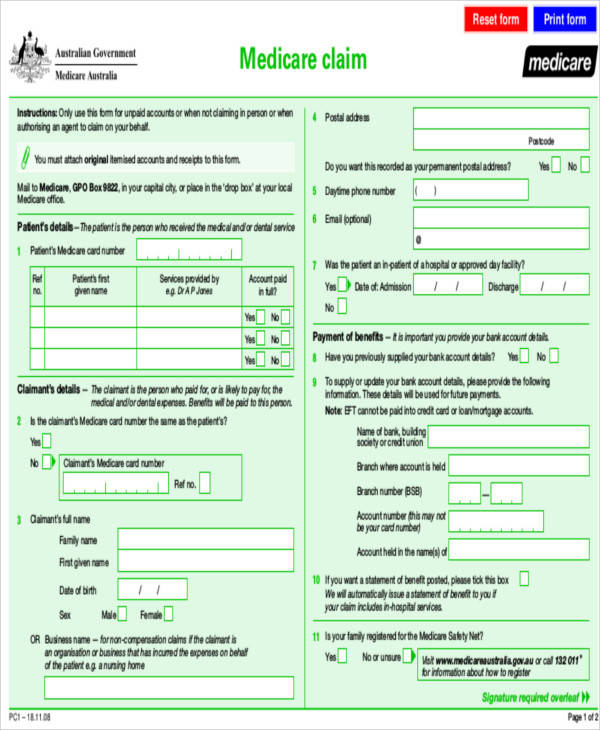
A time limit of two years applies to the lodgement of claims with Medicare under the direct billing (assignment of benefit) arrangements. This means that Medicare benefits are not payable for any service where the service was rendered more than two years earlier than the date the claim was lodged with Medicare.
What is timely filing limit?
Denials for “Timely Filing” In medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
Can I submit a paper claim to Medicare?
Claims may be filed to electronically (this applies to most Medicare providers) or on paper (if certain conditions or exceptions exist).May 26, 2021
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How do I fill out a CMS 1500 form for Medicare?
14:5319:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the categoryMoreField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the category of insurance that the policy falls into. It can be left blank.
What is a corrected claim?
A request made from a contracting provider to change a claim, (e.g., changing information on the service line, modifier addition, diagnosis correction, etc.) that has previously processed is considered a corrected claim. The submission of a corrected claim must be received by BCBSKS within the 15-month timely filing deadline. Claims denied requesting additional information (e.g. by letter or adjustment reason code) should never be marked "corrected claim" when resubmitted. Instead, providers should submit a new claim with the requested information.
Can a claim be corrected if denied?
Claims denied requesting additional information (e.g. by letter or adjustment reason code) should never be marked "corrected claim" when resubmitted. Instead, providers should submit a new claim with the requested information.
Does Tufts accept paper claims?
Tufts Health Plan accepts both electronic and paper corrected claims, in accordance with guidelines of the National Uniform Claim Committee (NUCC), the Medicare Managed Care Manual, and HIPAA EDI standards for Tufts Medicare Preferred HMO claims. Electronic Submissions. To submit a corrected facility or professional claim electronically:
What is a redetermination in Medicare?
A redetermination is a written request, for a first level appeal, to the Medicare administrative contractor to review claim data when you are dissatisfied with the original claim determination. The redetermination is an independent process to re-evaluate the claim.
What happens if you request a redetermination?
If the request for a redetermination is not approved or unfavorable, you will receive a letter notifying you of the decision. Requesting a redetermination.
What is general inquiry?
A general inquiry is a written correspondence initiated by you that includes questions related to Medicare billing, processing or payments. There may be times that a redetermination cannot be accepted and the request will be forwarded to the general inquires department for a response to you.
Can you file a redetermination over the phone?
Requests for redeterminations may not be filed over the telephone. All written redeterminations must contain the following items: The beneficiary name. The beneficiary Medicare number. The specific service (s) and/or item (s) for which the redetermination is being requested. The specific date (s) of service.
How long does it take to process a J15 claim?
Otherwise, you may contact the J15 Part A Provider Contact Center at (866) 590-6703 if the claim has not moved to a finalized location (XB9997) after 30 days (new claim) or 60 days (adjusted claim). The claim is missing information necessary to process the claim. The claim can be corrected or resubmitted.
When a claim is submitted to the Fiscal Intermediary Shared System (FISS), multiple editing processes are applied
When a claim is submitted to the Fiscal Intermediary Shared System (FISS), multiple editing processes are applied to identify possible errors. The chart below summarizes what happens to a claim that is subject to an edit and the appropriate process available to make claim corrections. Additional information about each claim correction process follows.
What is the redetermination process?
The redetermination process is the first level of appeal and applies to a claim or line item that receives a full or partial denial (identified as a claim in location DB9997 or a claim/line level reason code that begins with the number five or seven).
What is corrected claim?
A corrected claim is a claim that has already been processed, whether paid or denied, and is resubmitted with additional charges, different procedure or diagnosis codes or any information that would change the way the claim originally processed.
Can BCBSF appeal a corrected claim?
Note: BCBSF does not consider a corrected claim to be an appeal. When submitting a paper corrected claim, follow these steps: • Submit a copy of the remittance advice with the correction clearly noted.
