To submit all claims that have the three checkmarks without selecting each patient, select “Generate All Completed” and the user will be taken to a screen that shows three options: Submit Electronically – If claims are submitted through Axxess (the agency must have Axxess DDE to submit Medicare Claims electronically).
Full Answer
Where can I find more information about Medicare claims processing?
For more information please contact your local MAC or refer to the Medicare Claims Processing Manual (IOM Pub.100-04), Chapter 24.
How does electronic claims submission (ECS) work?
How Electronic Claims Submission Works: The claim is electronically transmitted from the provider's computer to the MAC. The MACs initial edits are to determine if the claims meet the basic requirements of the HIPAA standard. If errors are detected at this level, the entire batch of claims would be rejected for correction and resubmission.
Can providers that Bill institutional claims submit claims electronically?
Providers that bill institutional claims are also permitted to submit claims electronically via direct data entry (DDE) screens. How Electronic Claims Submission Works: The claim is electronically transmitted from the provider's computer to the MAC.
How do I submit a Medicare claim electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & ...
Do Medicare claims have to be submitted electronically?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
How do you put a claim into Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is the electronic payer ID for Medicare?
01112Medicare claim address, phone numbers, payor id – revised listStatePayer IDCaliforniaCA01112ColoradoCO04112ConnecticutCT13102DelawareDE1210246 more rows
How are electronic claims submitted?
Electronic claims may be transmitted by: Dial-up method, which uses a telephone line or digital subscriber line for claims submission. (Clearinghouses typically supply the physician practice with the software required for communication between the physician practice's computer and the clearinghouse's system.)
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Can I make a Medicare claim over the phone?
You can make a claim with the Express Plus Medicare mobile app on your mobile phone. Don't submit a claim if your doctor has done it for you.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What is the difference between manual and electronic claims submission?
An “electronic claim" is a paperless patient claim form generated by computer software that is transmitted electronically over the telephone or computer connected to a health insurer or other third-party payer (payer) for processing and payment, while A “manual claim” is a paper claim form that refers to either the ...
Which is an electronic format supported for healthcare claims transactions?
The transaction standard for health care claims or equivalent encounter data, professional, is the ASC X12N 837 format.
Where do I send Medicare Part B claims?
Mailing AddressesWho to WriteAddresses and Additional InformationAppealsClaimsJ15 — Part B/HHH Claims CGS Administrators, LLC PO Box 20019 Nashville, TN 37202Congressional InquiriesCGS Administrators, LLC J15 Part A/B Correspondence PO Box 20018 Nashville, TN 3720212 more rows
What does it mean to submit a claim directly to the payer?
Submitting claims directly at the payer’s website means manually keying transaction data repeatedly. Missing a value code, FIPS or CBSA code, setting up the payer under the incorrect Source of Payment and Insurance/Payer Type can cause a claim rejection or denial also.
Where are 837 claims sent?
Once a file is created as an 837I or 837P the claims are sent either directly to the payer or through a clearinghouse. A clearinghouse is the “central hub” where all claims are sorted and directed onward to all the various payers. Once the claim has been received, some clearinghouses will scrub the claims for errors before sending them to the appropriate parties. This is not the case with all clearinghouses, so it is important to know if claim validation services are included.
What happens if a provider is not credentialed?
If the provider is not credentialed with the payer, the enrollment will be rejected, and no EDI transactions can take place. If the enrollment is completed incorrectly or is not completed fully, this will cause a delay in the ability to submit claims electronically, again resulting in delay of payment.
What is EDI enrollment?
An Electronic Data Interchange (EDI) enrollment form must be completed prior to submitting claims electronically if the payer requires enrollment prior to EDI submission. This agreement must be approved by all parties; the healthcare provider, the clearinghouse and the payer. If the provider is not credentialed with the payer, the enrollment will be rejected, and no EDI transactions can take place. If the enrollment is completed incorrectly or is not completed fully, this will cause a delay in the ability to submit claims electronically, again resulting in delay of payment.
What is paperless claim?
Paperless patient claims or “electronic claims” are generated and transmitted electronically to a health insurer or third-party payer for processing and payment.
Can a per visit claim be electronic?
While per visit claims can have an electronic bill type of “professional” and a paper claim on a HCFA-1500 or “institutional” bill type with a paper claim on a UB-04.
Does Axxess pay faster?
With a direct connection to many payers, including Medicare, electronic claims submitted through Axxess software are paid faster than using traditional clearinghouse services. Using automation and electronic claims submission, providers will be able to be paid for the care they provide much faster and increase cash flow to grow business. Tweet.
Where are 837 claims sent?
Once a file is created as an 837I or 837P the claims are sent either directly to the payer or through a clearinghouse. A clearinghouse is the “central hub” where all claims are sorted and directed onward to all the various payers. Once the claim has been received, some clearinghouses will scrub the claims for errors before sending them to the appropriate parties. This is not the case with all clearinghouses, so it is important to know if claim validation services are included.
What is paperless claims?
Paperless patient claims or “electronic claims” are generated and transmitted electronically to a health insurer or third-party payer for processing and payment. This transaction reduces unnecessary administrative strain, reduces claim denials and lessens the expense involved with processing and submitting manual claims. Though this type of transaction comes with many benefits, there are some things to consider that require diligence so they do not cause issues for providers in the future.
What is EDI enrollment?
An Electronic Data Interchange (EDI) enrollment form must be completed prior to submitting claims electronically if the payer requires enrollment prior to EDI submission. This agreement must be approved by all parties; the healthcare provider, the clearinghouse and the payer. If the provider is not credentialed with the payer, the enrollment will be rejected, and no EDI transactions can take place. If the enrollment is completed incorrectly or is not completed fully, this will cause a delay in the ability to submit claims electronically, again resulting in delay of payment.
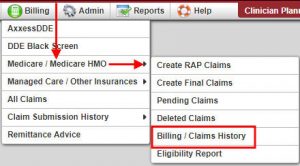
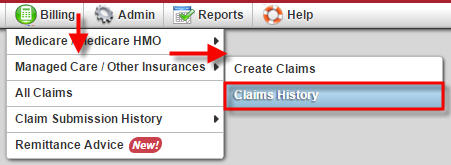
New Claim
Clicking on the New Claim button in the top right allows you to directly enter a claim and Save or Save and Submit to Medicare.
Saved Claims
Saved claims are found in the Outbox tab at the top of the claims page.
Cancel Claims
To Cancel a claim, click on the Claims tab then filter the claims data to Paid Status. Select Search.
View Claim
To view the Status Reason Code, simply hover over the status. A box will appear with the description of the reason code or status code for suspended claims. The Status location codes provide information about what is happening to the claim.
Copy Claim
When in the claim details, click Copy on the top right. This will make a copy of the claim that may be either edited and saved or saved and submitted as a new claim.
Edit Claim
To edit the claim, when in the claim detail, click on Edit at the top right corner of the page.
Must I use the Home Health solution to transmit billing requests to Medicare or can I utilize my existing process?
If you are currently downloading your claim files, You may continue to do so. Sending the claims directly from the Home Health solution to your clearinghouse or Medicare fiscal intermediary is a lot easier.
What insurance can I bill with the software?
You can bill any insurance company. You can find more information in the Insurance / Payor Information tutorial. However, in short to add a new insurance:
Can I submit a batch of claims?
You can submit a batch of claims. To do so, complete the RAP/final (EOE) verification process and select Generate all Completed. A list of all verified claims will appear, then select Submit Electronically.
When do I submit a RAP?
You can submit a RAP after the OASIS SOC or Recertification OASIS and the first billable visit has been completed.
Do I need to resubmit a RAP after making changes to the OASIS Assessment?
If the changes made affect the date or the HHRG, then you will need to submit those changes so that they reflect on the RAP.
Does the Home Health solution utilize HHRG (Home Health Resource Groups) groupers?
Yes, HHRG groupers are used to calculate the prospective payment for the episode.
What are HIPPS codes?
HIPPS is a Medicare acronym for Health Insurance Prospective Payment System (HIPPS). A HIPPS code is generated after an OASIS assessment is completed. The HIPPS code determines the prospective payment for the episode.
How to become an in network provider?
Healthcare providers enroll to become in-network providers by submitting an application to the payer (insurance company). Once the application is approved, the health insurance network will send reimbursements to the in-network provider for patient services.
What is Axxess RCM?
Our Axxess RCM team makes phone calls, emails clients, and schedules necessary meetings to ensure our clients have a full understanding of our enrollment process and involvement. Along with submitting provider information to start the enrollment process, we keep track of the enrollment status and deadline on behalf of our clients, allowing them the freedom to provide exceptional care and receive reimbursements without delays.
Why do insurance companies require EDI?
Some health insurance payers require EDI enrollment in order to submit claims electronically to avoid claim rejections. If a provider’s credentials or identification numbers are not found in the submitted payer’s database, claims will be rejected. With EDI enrollment, claims cannot reach the payer without providers’ credentials being certified.