How to submit fee-for-service and Medicare Advantage claims?
Table 1: How to submit Fee-for-Service and Medicare Advantage claims For beneficiaries enrolled in Original Fee-for-Service ( FFS) Medicare, providers submit claims for services to the appropriate MAC for covered Medicare Part A and Part B services. Contact your MAC if you have any questions about the Medicare Program.
Can a provider charge for filing a Medicare claim?
Medicare requires health care professionals or suppliers who furnish covered services to submit claims and cannot charge beneficiaries for completing or filing a Medicare claim. Table 1: How to submit Fee-for-Service and Medicare Advantage claims
How do I file a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How does Medicare define a claim?
Medicare defines a claim as a request for payment for benefits or services received by a beneficiary. Medicare requires health care professionals or suppliers who furnish covered services to submit claims and cannot charge beneficiaries for completing or filing a Medicare claim. Table 1: How to submit Fee-for-Service and Medicare Advantage claims

What is a GZ modifier for Medicare?
The GZ modifier indicates that an Advance Beneficiary Notice (ABN) was not issued to the beneficiary and signifies that the provider expects denial due to a lack of medical necessity based on an informed knowledge of Medicare policy.
How do Medicare crossover claims work?
1. What is meant by the crossover payment? When Medicaid providers submit claims to Medicare for Medicare/Medicaid beneficiaries, Medicare will pay the claim, apply a deductible/coinsurance or co-pay amount and then automatically forward the claim to Medicaid.
How do I file a claim with Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I bill Medicare tertiary claims?
Tertiary Claims can be submitted through the Fiscal Intermediary Standard System (FISS) Direct Data Entry (DDE) or by paper utilizing the UB-04 form. At this time, tertiary claims cannot be submitted to Novitas electronically.
When would you do a crossover claim?
A crossover claim is a claim for a recipient who is eligible for both Medicare and Medicaid, where Medicare pays a portion of the claim, and Medicaid is billed for any remaining deductible and/or coinsurance.
What is the Medicare crossover code?
CODE INDICATING THAT THE ELIGIBLE IS COVERED BY MEDICARE (KNOWN AS DUAL OR MEDICARE ELIGIBILITY), ACCORDING TO MEDICAID (MSIS), MEDICARE (EDB) OR BOTH IN THE CALENDAR YEAR.
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
What goes in box 33 on a HCFA?
Box 33 is used to indicate the name and address of the Billing Provider that is requesting to be paid for the services rendered. Enter the name, address, city, state, and ZIP code. P.O. Boxes are not allowed for electronic claims.
What are secondary and tertiary claims?
Secondary and Tertiary Claims If a secondary claim is submitted on paper the claim is printed onto a cms form and a copy of the explanation of benefits (eob) is attached. Tertiary Claims – Tertiary claims are submitted if the patient has a third insurance provider and if there is a balance left.
How do I submit Medicare Part as secondary?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
What is Field 11 in CMS 1500 claim form?
The street address, area, state, ZIP code, and telephone number are included. Box 11: This field requires the insured's policy or group number to be filled.
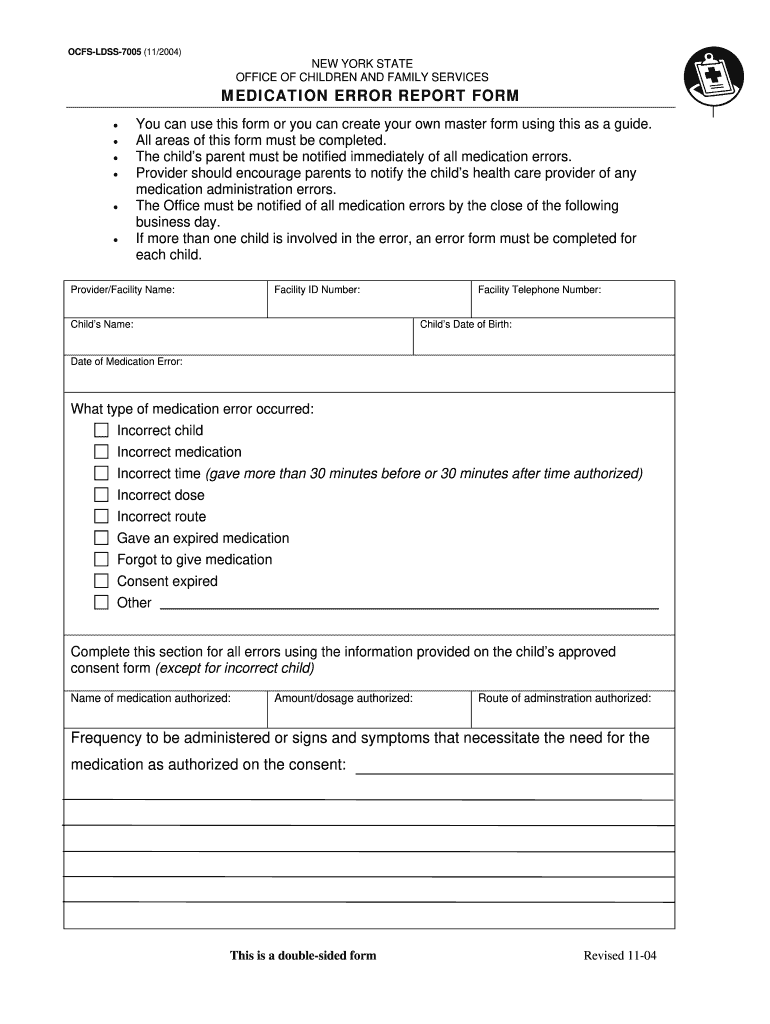
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is the correct HIC number?
HIC Format – A correct HIC number consists of 9 numbers immediately followed by an alpha suffix. Take special care when entering the HIC number for members of the same family who are Medicare beneficiaries. A husband and wife may have a HIC number that share the same Social Security numerics.
Do husband and wife have the same Social Security number?
A husband and wife may have a HIC number that share the same Social Security numerics. However, every individual has their own alpha suffix at the end of the HIC number. In order to ensure proper claim payment, it is essential that the correct alpha suffix is appended to each HIC. No hyphens or dashes should be used.
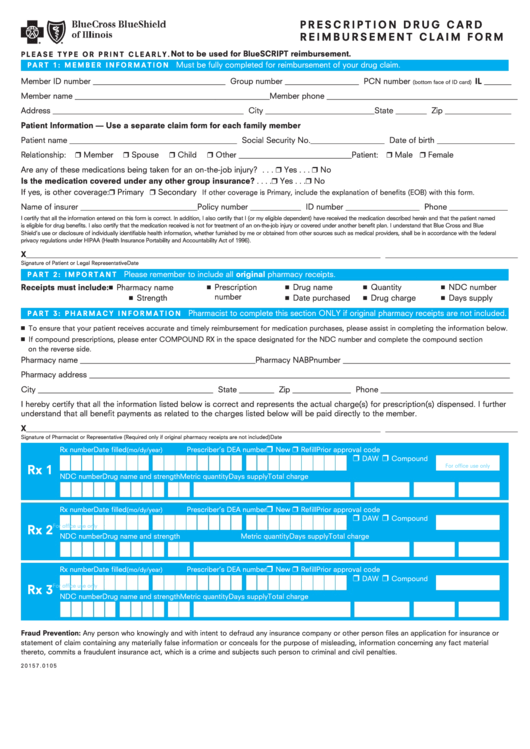
What is the alpha prefix on a BCBS card?
Most BCBS-branded ID cards display a three-character alpha prefix in the first three positions of the member’s ID number. However, there are some exceptions. ID cards for the following products and programs do not have an alpha prefix:
What is the BCBS prefix?
Every user of BCBS health insurance is assigned an alpha prefix that contains three letters. This prefix is the part of the distinctive identification number. If you are aware about the bcbs alpha prefix of your health insurance, then you can get the desired support on time for claiming the insurance.
What is the fax number for BCBS?
However, fax submission is allowed at the ollowing fax numbers: 866-365-5504 or 303-764- 7123 for BCBS OF CA AND BCBS OF CO. EMPIRE BCBS Decides the pre certification requirements based on the prefix id. Every user of BCBS health insurance is assigned an alpha prefix that contains three letters.
Why do you need an alpha prefix?
The alpha prefix is critical for inquiries regarding the member, including eligibility and benefits, and is necessary for proper claim filing. ** When filing a claim, always enter the ID number, including the alpha prefix, exactly as it appears on the member’s card. ** Always include the member’s ID number, including the alpha prefix, ...
Does Empire HMO have precertification?
Precertification remains the responsibility of the provider for all Empire HMO network members. HMO products include BlueChoice HMO, Direct Connection HMO, Child Health Plus, BlueChoice HMO/POS and Direct POS. Please refer to the member’s ID card to determine if he/she has one of these products.
Who is the only payer we work with who cares about the physical address on the claim forms when the claims are submitted
Magellan is the only payer we work with who cares about the physical address on the claim forms when the claims are submitted electronically. They have a few different P.O. Boxes they use and they want you to send your claims to a specific address based on the client's plan and location.
What is the payer ID for Quartz Health Solutions?
If you are filing claims to Quartz Health Solutions or Unity Health Insurance, payer ID 66705, please know that all claims should have the relationship to the insured marked as Self or Client. This is because the two digit suffix on a partner's or dependent's member ID acts as a unique member ID and this payer does not accept any claims which do not have the primary insured marked as Self.
What is the ID number for MVP Health Plan?
If you are filing claims to MVP Health Plan of New York, payer ID 14165, please know that all claims should have the relationship to the insured marked as Self or Client. This is because the two digit suffix on a partner's or dependent's member ID acts as a unique member ID and this payer does not accept any claims which do not have the primary insured marked as Self.
Can Medicare use billing NPI?
If Medicare has 2 NPI numbers on file for you ( a billing NPI and a provider NPI), be sure to use your billing NPI when filing CMS claim forms. See this guide for details: Populate your billing NPI to CMS claim forms.
Does Michigan have multiple BCBS payer IDs?
Some states like Michigan will have multiple BCBS payer IDs within SimplePractice. If you are located in Michigan, please follow these guidelines to ensure you are filing to the correct payer ID based on the client's benefits:
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…