We strongly encourage use of the CGMA, monthly EMR supplemental files, and/or claims to submit Medicare Quality Incentive Program data. However, if fax is the only option, we require the use of our QIP fax coversheet. Submissions that do not include the QIP fax coversheet will be returned unprocessed.
Full Answer
What are the guidelines for the Medicare quality incentive program?
The following guidelines apply to our Medicare Quality Incentive Program; participation in the program is voluntary. To be eligible for an incentive payment, you must have an active Medicare Advantage provider agreement in good standing at the time of incentive payment.
How do I qualify for a Medicare Advantage incentive payment?
To be eligible for an incentive payment, you must have an active Medicare Advantage provider agreement in good standing at the time of incentive payment. This includes participating in required compliance or Quality Program activities (e.g., timely submission of requested medical records for HEDIS risk adjustment reviews).
What is the quality incentive payment program?
HHSC Budget Rider 97 in the 2016-2017 budget directed HHSC to transition the Minimum Payment Amount Program to the Quality Incentive Payment Program. The QIPP is a Medicaid managed care delivery system and provider payment initiative in which HHSC directs expenditures through its contracts with the STAR+PLUS MCOs.
How do I submit QIPP data for a nursing home?
Quality Incentive Payment Program for Nursing Homes Submit your QIPP data online. Note: Supported browsers for data submission include Google Chrome, Firefox, and Safari. The Quality Incentive Payment Program serves as a resource to help nursing facilities achieve transformation.

How do I report MIPS?
Clinicians who are both MIPS APM participants and who are MIPS eligible at the individual or group level can report to traditional MIPS and/or report to MIPS via the APM Performance Pathway (APP). Qualifying APM Participants (QPs) and Partial QPs who elect not to report to MIPS, aren't required to report to MIPS.
What is Medicare quality Incentive Program?
The Quality Incentive Program (QIP) represents a new pay for-performance program for California's public health care systems that converts funding from previously-existing supplemental payments into a value-based structure, meeting the Managed Care Rule's option that allows payments tied to performance.
How do I check my MIPS score?
You can access your feedback and scores by visiting the Quality Payment Program login page and using your HCQIS Access Role and Profile, or HARP, credentials — they're the same credentials you used to submit your 2019 MIPS data.
How do you report promoting interoperability?
0:373:15Manual Attestation of Promoting Interoperability - YouTubeYouTubeStart of suggested clipEnd of suggested clipContact the qpp.MoreContact the qpp.
What is CMS quality based reporting?
Under the Hospital Inpatient Quality Reporting Program, CMS collects quality data from hospitals paid under the Inpatient Prospective Payment System, with the goal of driving quality improvement through measurement and transparency by publicly displaying data to help consumers make more informed decisions about their ...
What is QIP dialysis?
What is the ESRD QIP? The Centers for Medicare & Medicaid Services (CMS) administers the End-Stage Renal Disease Quality Incentive Program (ESRD QIP) to promote high-quality services in renal dialysis facilities.
What is the deadline for MIPS submission?
There's not much time left to submit your data — or to appeal for a pandemic-related exemption. March 31 is the deadline for MIPS-eligible clinicians who participated in the 2021 performance year of the Quality Payment Program to get their data into CMS and avoid penalties.
Do I need to report MIPS?
The 2022 MIPS quality category has a full-year performance period ranging from January 1, 2022 – December 31, 2022. This year, physicians may choose to report data on quality measures at the individual, group, or Virtual Group level using one reporting mechanism.
What is the minimum MIPS score for 2021?
60 pointsCMS is increasing the minimum threshold to 60 points (up from 45 points in 2020) for the new performance year. This means you must achieve at least 60 MIPS points to avoid a MIPS penalty.
Which program is an incentive program for physicians and eligible clinicians that links payment to quality measures and cost saving goals?
MIPS Overview The Merit-based Incentive Payment System (MIPS) is a program designed to tie payments to quality and cost-efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.
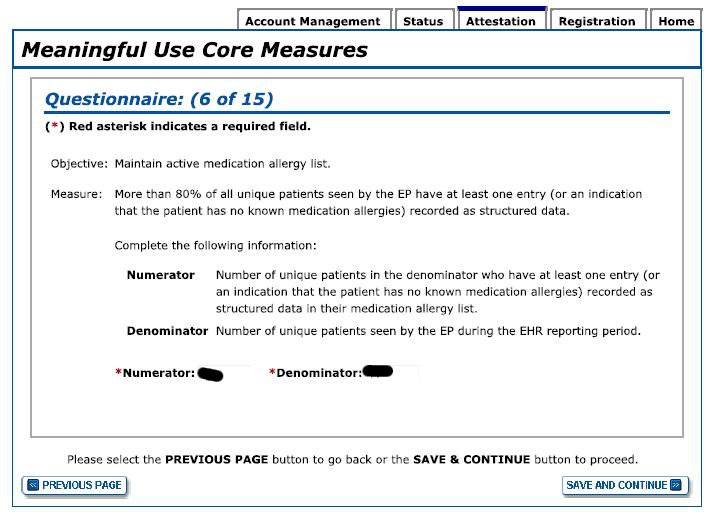
What organization directs the Medicare electronic health record incentive program?
The Centers for Medicare & Medicaid Services (CMS) EHR Incentive Program—also known as Meaningful Use or MU—initially provided incentives to accelerate the adoption of electronic health records (EHRs) to meet program requirements.
What is CMS interoperability?
CMS Interoperability and Prior Authorization Proposed Rule This proposed rule emphasizes the need to improve health information exchange to achieve appropriate and necessary access to complete health records for patients, health care providers, and payers.
Care Gap Management Application (CGMA)
The CGMA allows you to manage diagnosis and medical care gaps for each of your Medicare Advantage members and track your progress toward earning incentives in the Medicare Quality Incentive Program. The application includes all gaps related to the measures identified in these instructions.
Closing diagnosis gaps
All International Classification of Diseases (ICD) codes for existing and chronic conditions should be documented in a face-to-face visit with a Medicare-qualified provider at least once a year. The CGMA and care reminders include members who have at least one diagnosis with a reporting gap in the past two years.
How to contact Medicare EP?
Medicare EPs may contact the Quality Payment Program help desk for assistance at [email protected] or 1 (866) 288-8292. Back to TOP.
What is interoperability guide for medicaid?
The official Medicaid Program Interoperability user guides for Medicaid eligible hospital and EPs provide easy instructions for using CMS’s systems. They provide helpful tips and screenshots to walk the user through the registration process. Also, they provide important information needed to successfully register and attest.
What is CMS in EP?
CMS allows an EP to designate a third party to register and attest on his or her behalf. To do so, users working on behalf of an EP must have an Identity and Access Management System (I&A) web user account (User ID/Password), and be associated with the EPs National Provider Identifier (NPI).
How to contact QualityNet?
Medicare and dually eligible hospitals participating in the Medicare and Medicaid Promoting Interoperability Programs may contact the QualityNet help desk for assistance at 1 (866) 288-8912 or [email protected].
When is the self nomination period for QCDRs?
Self-Nomination Period Is Open for QCDRs and Qualified Registries. Third party intermediaries must self-nominate by September 1, 2021, to become a Qualified Clinical Data Registry (QCDR) or Qualified Registry for MIPS in 2022.
What is CMS reweighting?
CMS is reweighting the cost performance category from 15% to 0% for the 2020 performance period for all MIPS eligible clinicians regardless of participation as an individual, group, virtual group or APM Entity. The 15% cost performance category weight will be redistributed to other performance categories. No action is required.
Health Professional Shortage Area and Physician Scarcity Area Modifiers
The Medicare program provides incentive payments to physicians who render services in a Health Professional Shortage Area (HPSA).
Patient Relationship Categories and Codes
The Medicare Access and CHIP Reauthorization act of 2018 requires the development of PRC codes to help the attribution of patients and episodes to one or more physicians or applicable practitioners (clinicians) for purposes of cost measurement.
Appropriate Use Criteria (AUC)
Effective January 1, 2020 (the start of the AUC program Educational and Operations Testing Period) the modifiers listed in the chart below will be accepted when used to report AUC for Advanced Diagnostic Imaging Services.
What is the Quality Incentive Payment Program?
This performance-based program encourages NFs to improve the quality and innovation of their services through implementation of program-wide improvement processes for which facilities are compensated for meeting or exceeding certain goals. Improvement is based upon several indices of success, including quality metrics that are collected by the Centers for Medicare & Medicaid Services.
What is QIPP in Medicaid?
The QIPP is a Medicaid managed care delivery system and provider payment initiative in which HHSC directs expenditures through its contracts with the STAR+PLUS MCOs. Federal regulatory authority for such directed payments is contained in 42 Code of Federal Regulations §438.6 (c). QIPP Years One and Two.
When will QIPP end?
Performance requirements for MDS-based quality measures were reinstated for the fourth quarter, which ends on August 31, 2021. QIPP Year Five. On December 30, 2020, HHSC proposed changes to the quality metrics for QIPP Year Five (Sept. 1, 2021 to Aug. 31, 2022).
