How do I submit an authorization to Medicare?
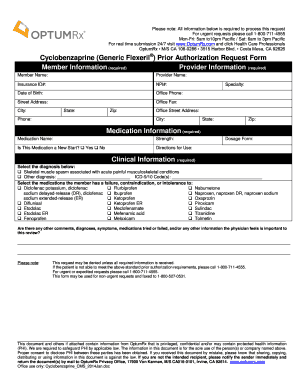
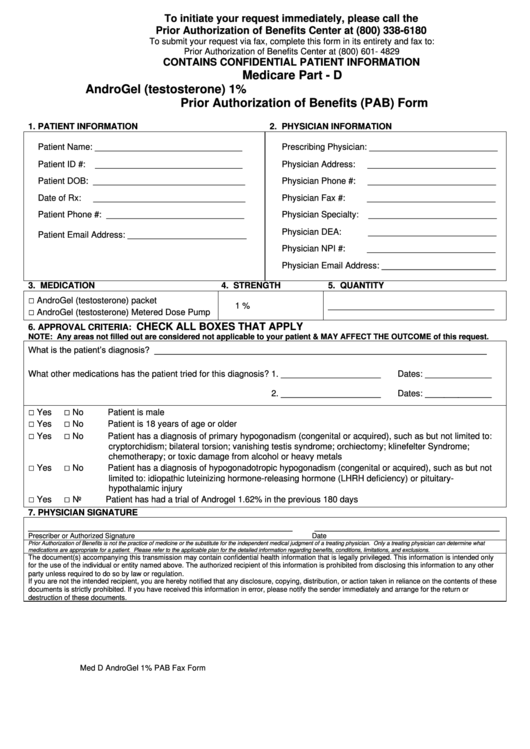
To do so, you can print out and complete this Medicare Part D prior authorization form, known as a Coverage Determination Request Form, and mail or fax it to your plan's office. You should get assistance from your doctor when filling out the form, and be sure to get their required signature on the form.Nov 24, 2021
How do I submit a pre authorization?
Take an active role and work closely with your doctor or the contact at your doctor's office to ensure they have the needed information. They will also need key dates for submitting the requests, so be sure to share that information as well. Identify who at your doctor's office handles prior authorizations.
What is Medicare prior authorization?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Is preauthorization required for Medicare?
Traditional Medicare, in contrast, does not require prior authorization for the vast majority of services, except under limited circumstances, although some think expanding use of prior authorization could help traditional Medicare reduce inappropriate service use and related costs.Oct 24, 2018
What is prior authorization process?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
How long does pre-authorization take?
around 5 daysA pre-authorization (also “pre-auth” or “authorization hold”) is a temporary hold on a customer's credit card that typically lasts around 5 days, or until the post-authorization (or “settlement”) comes through.Oct 18, 2021
How long does it take for Medicare to approve a procedure?
Medicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
Does Medicare require prior auth for MRI?
FAQs. Does Medicare require prior authorization for MRI? If the purpose of the MRI is to treat a medical issue, and all providers involved accept Medicare assignment, Part B would cover the inpatient procedure. An Advantage beneficiary might need prior authorization to visit a specialist such as a radiologist.
Who is responsible for obtaining prior authorizations?
Who is responsible for obtaining prior authorization? The healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patient's insurance provider.
What should you do with the authorization number once you have prior approval?
What should you do with the authorization number once you have prior approval? Document it in the financial record and on all forms associated with the procedure.
What is the difference between pre authorization and precertification?
Pre-authorization is step two for non-urgent or elective services. Unlike pre-certification, pre-authorization requires medical records and physician documentation to prove why a particular procedure was chosen, to determine if it is medically necessary and whether the procedure is covered.Apr 8, 2016
What is CMS approval?
CMS approvals are issued at a local level by the Medicare Administrative Contractor (MAC) or are reviewed an approved through a centralized process by CMS. Studies approved through the centralized process are listed here.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
What is prior authorization in Medicare?
Medicare Prior Authorization. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Do Medicare Advantage plans require prior authorization?
Private, for-profit plans often require Prior Authorization. Medicare Advantage (MA) plans also often require prior authorization to see specialists, get out-of-network care, get non-emergency hospital care, and more.
What Are The Negative Effects Of Prior Authorization
Perhaps the most significant negative effect is that prior authorization delays patient access to care. It adds a speed bump to the patient journey, and can lead some patients to forgo treatment.
Adhere To The Guideline Provided For Submission
Your prior authorization request may not get approved if you fail to follow the plans instruction. Accordingly, you must meet the criteria specified in the plans policy before attempting to submit the PA form. In that regard, check to see that you tick every box before they take the form for submission.
Does Medicare Require Prior Authorizations
Beneficiaries with Original Medicare generally do not need to obtain a prior authorization form for most Medicare services, such as doctors visits, hospitalizations, diagnostic studies or treatments.
Submit Thorough And Accurate Info
When you submit a prior authorization request, make sure the information you submit is totally accurate and is thorough. Prior authorization requests can be denied or delayed because of seemingly mundane mistakes.
Medicare Part D Prior Authorization
Often, even top Part D prescription drug plans need prior authorization for coverage on specific drugs. Different policies have varying rules, so youll need to contact the carrier directly to confirm coverage.
When Claims Are Denied For No Authorization
Even as billers work diligently to reduce claims denials, payers are expanding the number of visit types and procedures that require prior authorization leading to an upswing in denials for some practices. It is estimated that 80% of denied claims have to do with no authorization being obtained, or authorizations being requested improperly.
Submit New Prior Authorization Request
Part A users may submit a request for a new Prior Authorization request by completing and uploading the Prior Authorization coversheet. As of June 17, 2020, Prior Authorizations are only required for certain Hospital Outpatient Department services.
Why do we need prior authorization?
Prior authorization can help protect a beneficiary’s rights to covered Medicare benefits, and it can also act as a means of reducing improper billing, waste and fraud within the Medicare system . It also helps to cut down on over-utilization of unnecessary care.
Do you need prior authorization for Medicare Part C?
It’s not uncommon, however, for beneficiaries of Medicare Advantage (Medicare Part C) plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care. Prior authorization is most common for getting certain prescription drugs covered by your plan.
Submit New Prior Authorization Request
Part A users may submit a request for a new Prior Authorization request by completing and uploading the Prior Authorization coversheet. As of June 17, 2020, Prior Authorizations are only required for certain Hospital Outpatient Department (OPD) services.
Prior Authorization Request Status
Part A users may check the status of Prior Authorization requests, view the reviewer notes, and add/view related documents.
Response
The response page provides a summary of the provider information that was used in the search.
What is prior authorization?
A: Prior authorization is a process through which a request for provisional affirmation of coverage is submitted for review before the service is rendered to a beneficiary and before a claim is submitted for payment. The prior authorization program for certain hospital OPD services ensures that Medicare beneficiaries continue to receive medically necessary care while protecting the Medicare Trust Funds from unnecessary increases in the volume of covered services and improper payments. The prior authorization process does not alter existing medical necessity documentation requirements. Prior authorization helps to make sure that applicable coverage, payment, and coding requirements are met before services are rendered while ensuring access to and quality of care.
What services are required prior authorization?
required prior authorization for the following services: blepharoplasty, botulinum toxin injections, panniculectomy, rhinoplasty, and vein ablation. As part of the Calendar Year 2021 OPPS/ASC Final Rule (CMS-1736-FC), CMS will require prior authorization for two additional services: cervical fusion with disc removal and implanted spinal neurostimulators. The Final List of Outpatient Services that Require Prior Authorization is located here.
What is an ABN in Medicare?
A: An ABN may be issued if the provider advises the beneficiary in advance that they expect payment for a service to be denied by Medicare under the statutory exclusion for cosmetic services. The provider should submit the claim with a GX modifier. The ABN is voluntary, and is not required to bill the patient for the service if it is denied under the cosmetic services exclusion. However, we encourage providers to issue an ABN in this situation to inform the beneficiary of the likelihood of financial liability.
What is a resubmitted request?
A: A resubmitted request is a subsequent prior authorization review request submitted after the initial review request was submitted, reviewed, and a non- affirmation decision was made. A request that is resubmitted with no additional documentation or information will likely receive a non-affirmation decision.
How long is a provisional affirmation valid?
A: A provisional affirmation is valid for 120 days from the date the decision was made. If the date of service is not within 120 days of the decision date, the provider will need to submit a new prior authorization request.
Why is CPT 63685 removed?
A: CMS is temporarily removing CPTs 63685 and 63688 to streamline requirements for the intial implementation of prior authorization for implanted spinal neurostimulators. CMS will monitor prior authorization for CPT 63650 to determine if it is effective in reducing the volume of unnecessary implanted spinal neurostimulator services.
Does Medicare have a prior authorization?
A: Yes. The CMS believes this prior authorization program will both help protect the Medicare Trust Funds from improper payments and make sure beneficiaries are not hindered from accessing necessary services when they need them. Prior authorization allows CMS to make sure items and services frequently subject to unnecessary utilization are furnished or provided in compliance with applicable Medicare coverage, coding, and payment rules before they are furnished or provided. It also allows the beneficiary to be notified if the item or service would be covered by Medicare and any potential financial implications earlier in the payment process. Access is preserved by having set timeframes for contractors to complete any prior authorization request decisions, and an expedited process is available in cases where delays may jeopardize the life or health of beneficiaries.
What is a prior authorization form for Medicare?
Medicare Prior (Rx) Authorization Form. Medicare members who have prescription drug coverage (Part D) will be covered for almost all their medication costs. Original Medicare members most likely have chosen to join a Medicare Prescription Drug Plan (PDP) for an additional premium.
How to get a fax number for a Medicare plan?
Step 1 – Enter the name, phone number, and fax number of the member’s plan. Step 2 – In the “Patient Information” section, provide the patient’s name, ID number, address, phone number, gender, and date of birth.
How long does it take for a health insurance plan to respond?
Call your plan or check on their website to look up the proper mailing address or fax number. Plans must respond within 72 hours of receiving your request form. If the physician feels the request is an emergency situation, an expedited review of 24 hours should take place.
When will the new Medicare authorization program be available?
The Centers for Medicare & Medicaid Services is implementing a prior authorization program for certain hospital outpatient department services for dates of service on or after July 1, 2020.
What is prior authorization?
Prior authorization is a process through which coverage is determined prior to providing or billing the service. This process allows the provider to submit documentation prior to providing or billing the service. The contractor will then alert the submitter of any potential issues with the submitted information.
What is an expedited prior authorization request?
Expedited Prior Authorization Request Hospital Outpatient Procedures Medicare Part A Fax/Mail Coversheet - Allowable if it is determined that a delay could seriously jeopardize the beneficiary’s life, health, or ability to regain maximum function.
When is prior authorization for outpatient services?
CMS is implementing a prior authorization program for certain hospital outpatient department services for dates of service on or after July 1, 2020. Review the fax coversheet needed for submission.
What is MACRA in Medicare?
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) expands the repetitive scheduled non-emergent ambulance transport prior authorization model to all states if the program meets certain requirements. [CR9940]