Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048.
Full Answer
Who can use the UB-04 form for billing medical claims?
Any institutional provider can use the UB-04 for billing medical claims. This includes: To fill out the form accurately and completely, be sure to do the following: Check with each insurance payer to determine what data is required. Ensure that all data is entered correctly and accurately in the correct fields.
When do benefits exhaust and no payment bills need to be submitted?
Benefits Exhaust and No-Payment Billing. A SNF is required to submit a claim to Medicare when the beneficiary: Has exhausted his/her 100 covered days under the Medicare SNF benefit (benefits exhaust); or No longer needs a Medicare covered level of care (no-payment bills).
Does Medicare require SNFS to submit monthly billings?
In addition to the “Benefit Exhaust” and “No Pay” Claims needing to be billed Monthly there is one other type of bill that Medicare now requires SNFs to submit. If you accept and bill for Managed Care Replacement Plans CMS requires your facility to submit Managed Care “Informational” Claims to Medicare on a monthly basis.
What is a Medicare no-payment claim?
No-payment claims are submitted for beneficiaries who previously dropped to non-skilled care and who continue to reside in the Medicare-certified area of the facility. No-payment billing starts the day following the date that active care ended. There are two options for billing: Patient previously dropped to non-skilled care within the month.

Does Medicare accept ub04?
The CMS-1450 form (aka UB-04 at present) can be used by an institutional provider to bill a Medicare fiscal intermediary (FI) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of claims.
How do I file a Medicare void claim?
You might want to cancel a Medicare claim if you believe you made an error. The fastest way to cancel a claim is to call Medicare at 800-MEDICARE (800-633-4227). Tell the representative you need to cancel a claim you filed yourself.
Can I submit paper claims to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
What is Medicare no pay?
A No Pay Bill is a bill you submit in a situation where you will not receive any money from Medicare. No pay bills are not new, but, in 2006, CMS clarified their policy and issued instructions that all providers and fiscal intermediaries must follow.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.
How do I submit a void claim?
These are the steps you can take to void/cancel a claim: Contact the payer and advise that a claim was submitted in error. Ask if this claim should be voided/cancelled, so that you can submit a claim with the correct information. Some payers will allow you to void/cancel the claim over the phone.
Does Medicare accept handwritten claims?
Medicare to Reject Handwritten Claims. Providers who wish to continue to submit paper claims may do so as long as they are printed and as long as the only handwriting included in the claim is in a signature field. Software programs are available that will allow providers to print information into a CMS 1500 form.
Does Medicare accept secondary paper claims?
If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.
What form is used to send claims to Medicare?
Form CMS-1500Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
When should I submit a rap?
RAPs are submitted at the beginning of each 30-day period. Home health agencies (HHAs) newly enrolled in Medicare on or after January 1, 2019, shall submit a no-pay RAP at the beginning of each 30-day period.
Can we bill Medicare patients for non covered services?
Under Medicare rules, it may be possible for a physician to bill the patient for services that Medicare does not cover. If a patient requests a service that Medicare does not consider medically reasonable and necessary, the payer's website should be checked for coverage information on the service.
Can you bill a Medicare patient without an ABN?
The patient will be personally responsible for full payment if Medicare denies payment for a specific procedure or treatment. The ABN must be given to the patient prior to any provided service or procedure. If there is no signed ABN then you cannot bill the patient and it must be written off if denied by Medicare.
What is NUBC billing?
The National United Billing Committee (NUBC) is a voluntary and multidisciplinary committee that develops data elements for claims and transactions. The NUBC is responsible for the design and printing of the UB-04 form. 1.
How many fields are there on a UB-04?
There are 81 fields or lines on a UB-04. They're referred to as form locators or "FL.". Each form locator has a unique purpose: Form locator 1: Billing provider name, street address, city, state, zip, telephone, fax, and country code.
What is UB-04 form?
The UB-04 uniform medical billing form is the standard claim form that any institutional provider can use for the billing of inpatient or outpatient medical and mental health claims. It is a paper claim form printed with red ink on white standard paper. Although developed by the Centers for Medicare ...
What is the difference between UB-04 and CMS 1500?
What is the difference between the UB-04 and the CMS 1500 forms? The UB-04 form is used by institutional providers, such as nursing homes and hospitals, while the CMS-1500 form is the standard claim form used by a non-institutional provider or supplier, such as a physician or a provider of durable medical equipment. 2.
How to fill out a CPT form?
To fill out the form accurately and completely, be sure to do the following: 1 Check with each insurance payer to determine what data is required. 2 Ensure that all data is entered correctly and accurately in the correct fields. 3 Enter insurance information including the patient's name exactly as it appears on the insurance card. 4 Use correct diagnosis codes ( ICD-10) and procedure codes (CPT/HCPCS) using modifiers when required. 5 Use only the physical address for the service facility location field. 6 Include National Provider Identifier (NPI) information where indicated.
What is a claim form?
It is a paper claim form printed with red ink on white standard paper. Although developed by the Centers for Medicare and Medicaid Services (CMS), the form has become the standard form used by all insurance carriers. 1. Hero Images / Getty Images.
What bill type is used for SNF?
Bill Type – Use TOB 211 or 214 for SNF and 181 or 184 for Swing Bed. Note: Do not use TOBs 210 or 180 for benefits exhaust claim. Covered Days and Charges - Submit all covered days and charges as if the beneficiary had days available until the date of discharge.
What does CMS do for Medicare?
CMS keeps a record of all inpatient services for each beneficiary, including those which are not covered by Medicare. The information from the claims is used for national healthcare planning and also helps CMS keep track of each beneficiary's benefit period.
When is a SNF required?
A SNF is required to submit a claim to Medicare when the beneficiary: Has exhausted his/her 100 covered days under the Medicare SNF benefit (benefits exhaust); or. No longer needs a Medicare covered level of care (no-payment bills).
Do SNFs have to submit exhaust claims?
A SNF must submit a benefits exhaust claim on a monthly basis for their patients who continue to receive skilled care and when there is a change in the patient's level of care. These claims are required so that the beneficiary's applicable benefit period posted in the Common Working File (CWF) can be extended.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.

Who Can Bill Claims Using The UB-04?
Tips For Preparing The UB-04
- To fill out the form accurately and completely, be sure to do the following: 1. Check with each insurance payer to determine what data is required. 2. Ensure that all data is entered correctly and accurately in the correct fields. 3. Enter insurance information including the patient's name exactly as it appears on the insurance card. 4. Use correct...
Fields of The UB-04
- There are 81 fields or lines on a UB-04. They're referred to as form locators or "FL." Each form locator has a unique purpose: 1. Form locator 1: Billing provider name, street address, city, state, zip, telephone, fax, and country code 2. Form locator 2: Billing provider's pay-to name, address, city, state, zip, and ID if it's different from field 1 3. Form locator 3: Patient control number and th…
A Word from Verywell
- While the UB-04 form is intended mainly for institutional providers to billinsurance companies, it's never a bad idea to inform yourself about what goes into medical claims. If you see something you don't understand, ask your insurer or provider to explain it to you.
Frequently Asked Questions
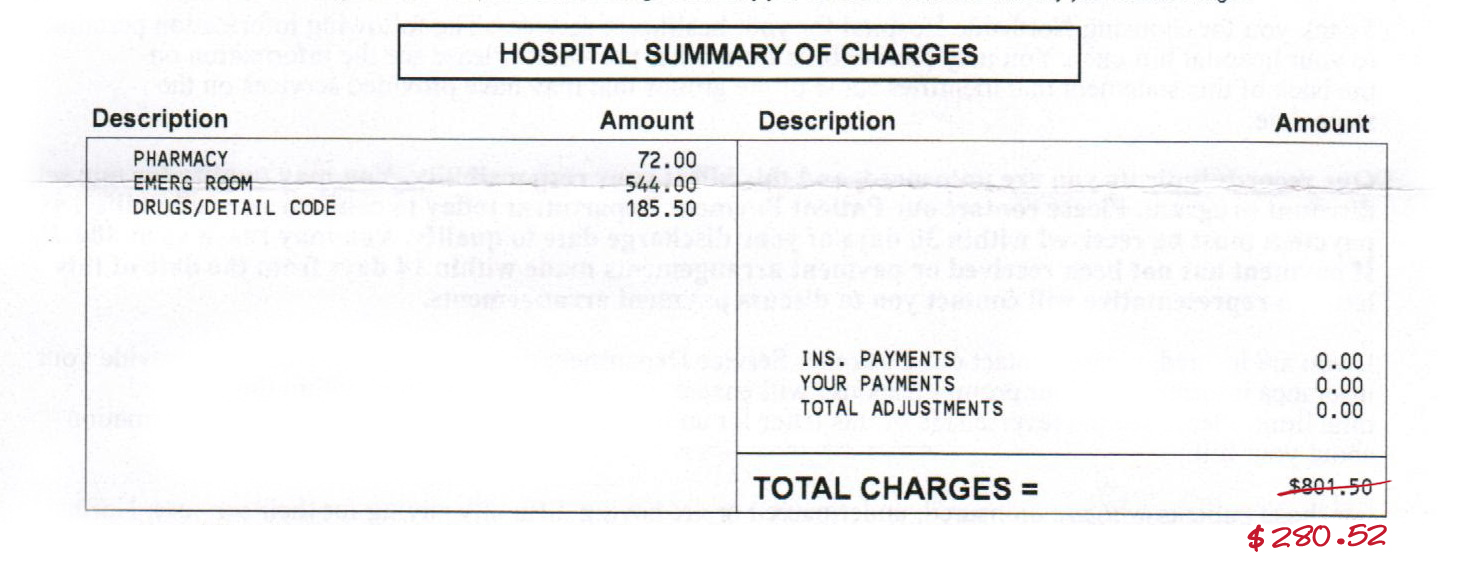
- Is there a difference between the UB-04 and an itemized bill?
An itemized medical billlists in detail all the services that were provided during a visit or stay—such as a blood test or physical therapy—and may be sent to the patient directly. The UB-O4 form is used by institutions to bill Medicare or Medicaid and other insurance companies. - What is the difference between the UB-04 and the CMS 1500 forms?
The UB-04 form is used by institutional providers, such as nursing homes and hospitals, while the CMS-1500 form is the standard claim form used by a non-institutional provider or supplier, such as a physician or a provider of durable medical equipment.2