How to Use Medicare Milestones Issues Most Effectively
- Determine a schedule of clients that will turn 65 over the next 12 month period.
- Use the following suggested mailing schedule:
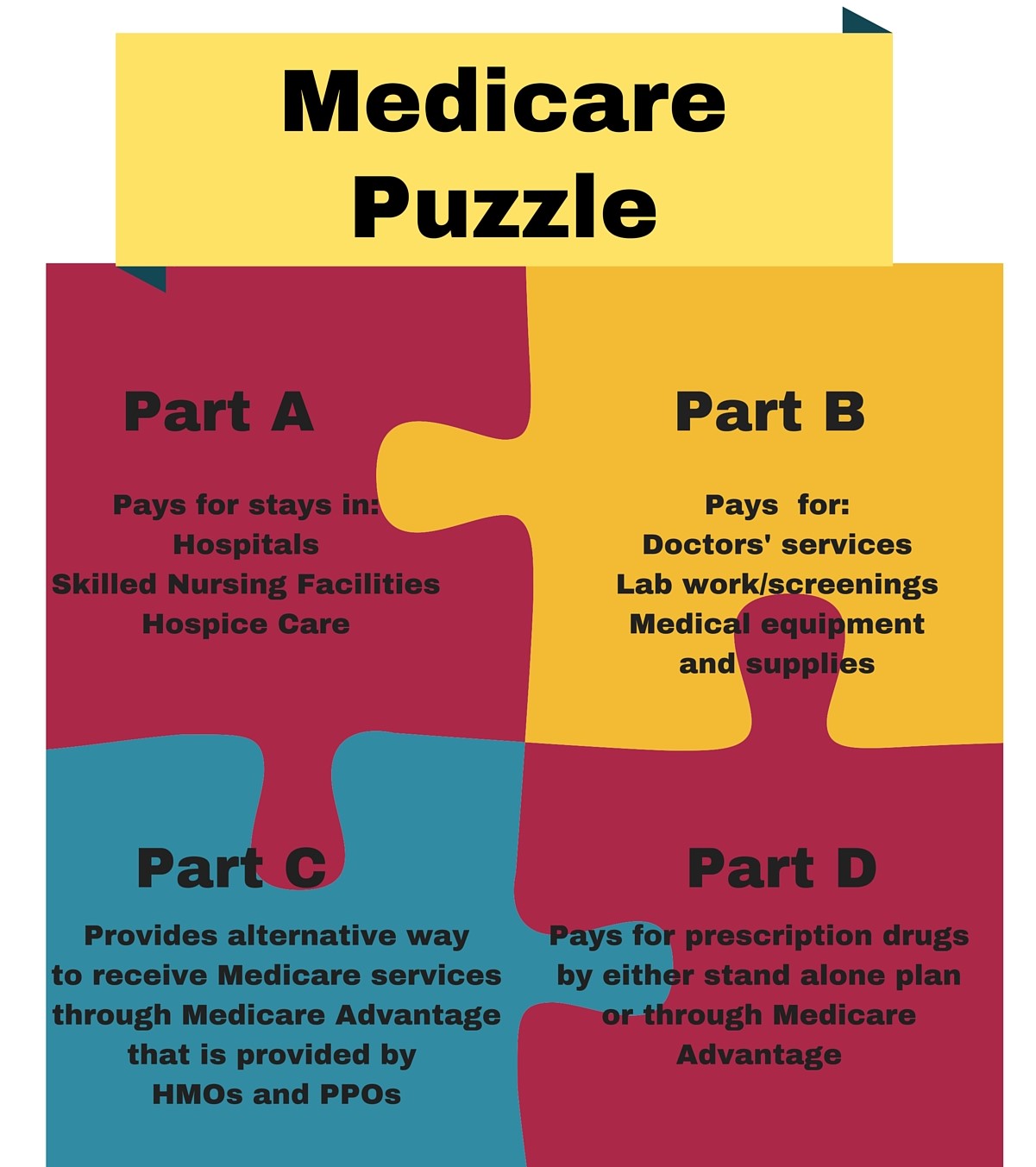
- When your client is about to turn 64, send issue
- 1,"Turning 65: The Parts of Medicare," (See illustration 1) along with...
- Four months after your client's 64th birthday, send issue
- 2,...
Full Answer
How do I start Medicare?
First, find out when your plan becomes effective. Then find your plan’s formulary, or list of covered drugs, and pharmacy network. Work out any issues with prescription coverage, like getting drugs that are not on the formulary, switching to generics to save money, or appealing decisions regarding coverage.
How to get started on Medicare?
Medicare offers different options for you to get health care coverage. Start here to get the basics and find out how Medicare works before you look at your coverage options. Parts of Medicare
How can you tell if someone has Medicare?
Get started with Medicare. Medicare is health insurance for people 65 or older. You’re first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig’s disease). Follow these steps to learn about Medicare ...
How do I decide on which Medicare plan to use?
With Original Medicare, you can: Go to any doctor or hospital that takes Medicare, anywhere in the U.S. Find providers that work with Medicare. Join a separate Medicare drug plan (Part D) to get drug coverage. Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.

How do I get the best out of Medicare?
- Shop around each and every year. Original Medicare, which consists of Part A (hospital insurance) and Part B (outpatient services) is pretty straightforward. ...
- Consider a Medicare Advantage plan. ...
- Consider buying supplemental insurance if you have a chronic illness. ...
- Enroll on time.
What is the 21 day rule for Medicare?
What is the 60 day rule for Medicare?
How do you use Medicare?
Go to any doctor or hospital that takes Medicare, anywhere in the U.S. Find providers that work with Medicare. Join a separate Medicare drug plan (Part D) to get drug coverage. Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.
Why do doctors not like Medicare Advantage plans?
Which type of care is not covered by Medicare?
Does Medicare cover ICU costs?
What happens when Medicare runs out?
Does Medicare have a maximum lifetime benefit?
What are the 4 types of Medicare?
- Part A provides inpatient/hospital coverage.
- Part B provides outpatient/medical coverage.
- Part C offers an alternate way to receive your Medicare benefits (see below for more information).
- Part D provides prescription drug coverage.
Does Medicare cover eye exams?
Medicare doesn't cover eye exams (sometimes called “eye refractions”) for eyeglasses or contact lenses. You pay 100% for eye exams for eyeglasses or contact lenses.
How long before you turn 65 do you apply for Medicare?
It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
Parts of Medicare
Learn the parts of Medicare and what they cover. Get familiar with other terms and the difference between Medicare and Medicaid.
General costs
Discover what cost words mean and what you’ll pay for each part of Medicare.
How Medicare works
Follow 2 steps to set up your Medicare coverage. Find out how Original Medicare and Medicare Advantage work.
Working past 65
Find out what to do if you’re still working & how to get Medicare when you retire.
Medicare basics
Start here. Learn the parts of Medicare, how it works, and what it costs.
Sign up
First, you’ll sign up for Parts A and B. Find out when and how to sign up, and when coverage starts.
What is Medicare Advantage?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Why buy Medicare Supplement Insurance?
Buy a Medicare Supplement Insurance (Medigap) policy to help lower your share of costs for services you get.
Is Medicare a private insurance?
Medicare is different from private insurance — it doesn’t offer plans for couples or families. You don’t have to make the same choice as your spouse.
Do you have to have original Medicare if you have Medicare Advantage?
You’ll have Original Medicare unless you join a Medicare Advantage Plan.
Does Medicare cover urgent care?
Plans must cover all emergency and urgent care, and almost all medically necessary services Original Medicare covers. Some plans tailor their benefit packages to offer additional benefits to treat specific conditions.
Get started with Medicare
Get basics on how Medicare works, sign up, and review your options for more coverage. Learn about it at your own pace.
Medicare costs
Learn about Medicare costs, how to pay premiums, and cost-saving programs.
Identity theft & fraud: Protect yourself
Find out how to protect your personal information, including your Medicare Number, and how to spot and stop scams and fraud.
How many people are covered by Medicare?
Medicare has undoubtedly helped millions of seniors and disabled adults receive health coverage since being signed into law in 1965. Today, Medicare covers 55 million beneficiaries across the US. In the coming decades though, Medicare faces a complex multitude of competing environmental pressures. First, the sheer size of the Medicare-eligible population is projected to increase significantly: according to the US census, by 2029 all the baby boomers will be 65 or older which will account for 20 percent of the US population. Adding to that increased pressure is the trends showing this population will be living with more disabilities and living longer than previous generations.
What is fragmented prescribing of opioids?
Fragmented prescribing-whereby no specific physician is solely responsible for a patient’s needs for opioid prescription-or intentional doctor shopping by patients, lead to adverse health outcomes. We found that Medicare patients who received prescription opioids from four or more unique providers had twice the annual rate of hospital admission than those who received prescription opioids from only one provider.#N#STRATEGIES IN ACTION:
How does medical technology impact healthcare?
Policymakers acknowledge that new medical technologies can improve patient care. Yet they often focus on how these new products and services put fiscal strain on government budgets rather than their benefit to society. Recently, the Medicare Payment Advisory Commission cited medical technology as having the greatest impact on health care spending. Nevertheless, medical innovations can provide health benefits that outweigh their additional costs. By applying a framework for the quality-adjusted cost of care, which takes into account both value and direct financial costs, policymakers can gain more complete insight into the value of investments from Medicare into new medical technologies that better takes into account patients’ health outcomes.
What are the four evidence-based recommendations that would measurably improve the delivery of services?
Through this research four evidence-based recommendations which would measurably improve the delivery of services have been found: 1. Help people pick the right Medicare plans for them. Center experts found that when Medicare beneficiaries choose a prescription drug plan, poor plan choices result in extra costs and reduced access to necessary drugs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
When is Medicare paid first?
When you’re eligible for or entitled to Medicare because you have End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, the group health plan or retiree coverage pays first and Medicare pays second. You can have group health plan coverage or retiree coverage based on your employment or through a family member.
When to ask Medicare patients for their cards?
Ask your Medicare patients for their Medicare cards when they come for care. If they don’t bring it with them when they come for care, give them the Get Your New Medicare Card flyer in
What is a COBA in Medicare?
Medicare' s Coordination of Benefits Agreement (COBA) trading partners (supplemental insurers, Medigap plans, Medicaid, etc.) must submit the MBI to get Medicare crossover claims. Exceptions on use of HICN on outbound Medicare crossover claims will apply.
Can you look up MBIs for Medicare?
You can look up MBIs for your Medicare patients when they don’t or can’t give them. Sign up for the Portal to use the tool. Even if your patients are in a Medicare Advantage Plan, you can look up their MBIs to bill for things like indirect medical education.