- You must be under the care of a doctor, and you must be getting services under a plan of care created and reviewed regularly by a doctor.
- You must need, and a doctor must certify that you need, one or more of these: ...
- You must be homebound, and a doctor must certify that you're.
Does Medicare pay for help around the house?
What types of healthcare services can be provided in a patient's home?
- Doctor care. A doctor may visit a patient at home to diagnose and treat the illness(es). ...
- Nursing care. ...
- Physical, occupational, and/or speech therapy. ...
- Medical social services. ...
- Care from home health aides. ...
- Homemaker or basic assistance care.
How Long Will Medicare pay for home health care?
What is the difference between home care and home health care?
What Is Home Health Care?
Home health care can involve a wide range of services you may need when you’re ill or recovering from an illness or surgery. In some cases it can i...
In-Home Care: Medical and Non-Medical
Depending on what is available in your community, home care can include: 1. Health care – skilled nursing care; physical, speech, occupational and...
Does Medicare Cover Home Health Care?
Medicare Part A and/or Part B may help pay for your home health care if these conditions apply to you: 1. You’re under the care of a doctor who acc...
Home Health Care and Medicare Supplement Insurance
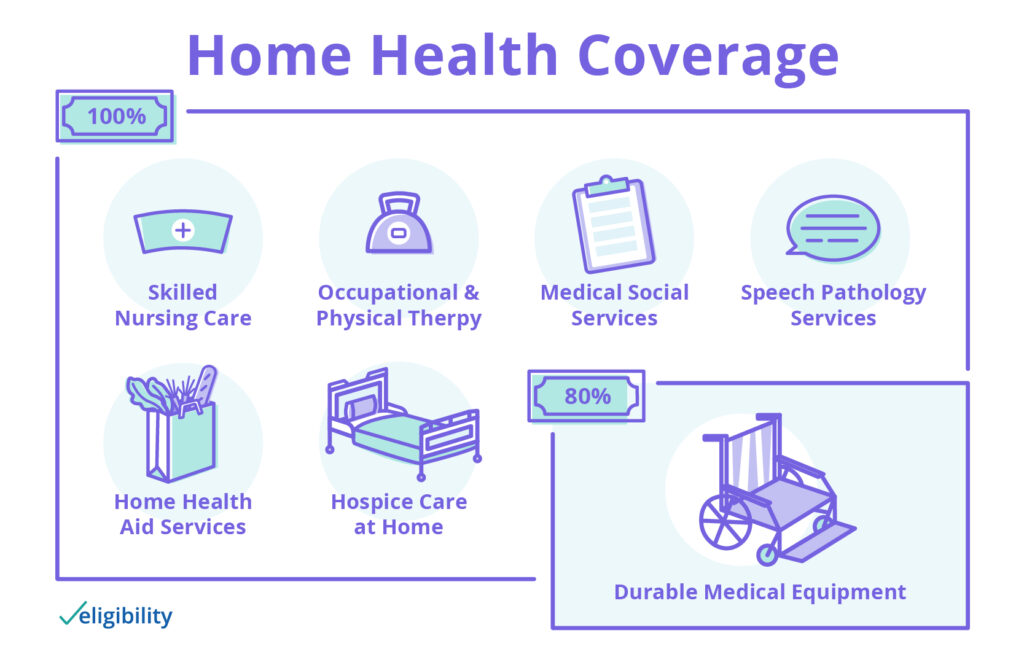
You might have to pay a coinsurance amount in some cases; for example, under Medicare Part B, you usually pay 20% of durable medical equipment cost...
Not All Home Health Care Agencies Are Created Equal
Home health agencies vary in the services they offer, and not every agency is certified by Medicare. You may want to match your needs with the serv...
How many days can you have home health care?
care. You can have more than one 30-day period of care. Payment for each 30-day period is based on your condition and care needs. Getting treatment from a home health agency that’s Medicare-certified can reduce your out-of-pocket costs. A Medicare-certified home health
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
How many days can you be on Medicare?
Fewer than 7 days each week. ■ Daily for less than 8 hours each day for up to 21 days. In some cases, Medicare may extend the three week limit if your
What is the ABN for home health?
The home health agency must give you a notice called the “Advance Beneficiary Notice of Noncoverage” (ABN) in these situations. See the next page.
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is homemaker service?
Homemaker services, like shopping, cleaning, and laundry ■ Custodial or personal care like bathing, dressing, and using the bathroom when this is the only care you need
What is home health aide?
Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom. Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
What services are not covered by Medicare?
Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
Does Medicare cover home health?
Medicare might cover some in-home health care in some situations – but not all. Let’s get into the details.
Does Medicare Advantage cover Part A?
Medicare Advantage plans provide your Medicare Part A and Part B coverage. Instead of getting Part A and Part B through the federal government directly, you get them through a private insurance company that contracts with Medicare.
Do doctors have to certify in-home care?
Your doctor has to certify that you need certain kinds of in-home care, such as:
Do in home health agencies have to be Medicare approved?
The in-home health agency must be Medicare-approved.
Do you have to pay Medicare Part B premium?
Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending. You’ll need to keep paying your Medicare Part B premium (along with any premium the plan may charge) when you have a Medicare Advantage plan.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
Is home health agency approved by Medicare?
3. The home health agency caring for you is approved by Medicare.
Do parents have rights to health care?
You also may be comforted by the fact that your parents have rights as far as their health care is concerned. These include having their property treated with respect; to be told, in advance what care they’ll be getting and when their plan of care is going to change; to participate in their care planning and treatment.
Does Medicare cover home aides?
Medicare also covers continuous health care but on a different level. It only covers a percentage of the cost. Unfortunately, home aides that help with housework, bathing, dressing and meal preparations are not covered by Medicare.
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
What are some examples of Medicare Advantage Plans?
Examples of Medicare Advantage Plans include health maintenance organization (HMO) or a preferred provider organization (PPO). If you have these plan types, you’ll likely need to get your home health services from an agency your plan specifically contracts with.
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
What education do you need to be a home health aide?
According to the U.S. Bureau of Labor Statistics, the typical educational level for a home health aide is a high school diploma or equivalent. Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist.
What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
What is the fee Medicare sets for a covered medical service?
The fee Medicare sets for a coveredmedical service. This is the amount adoctor or supplier is paid by you andMedicare for a service or supply. It maybe less than the actual amount chargedby a doctor or supplier. The approvedamount is sometimes called the“Approved Charge.”
What is an appeal in Medicare?
An appeal is a special kind of complaintyou make if you disagree with a decision todeny a request for health care services, orpayment for services you already received.You may also make a complaint if youdisagree with a decision to stop servicesthat you are receiving. For example, youmay ask for an appeal if Medicare doesn’tpay for an item or service you think youshould be able to get. There is a specificprocess that your Medicare health plan orthe Original Medicare Plan must use whenyou ask for an appeal.
How many measures are there for improving mental health?
four measures related to improvement in getting around, four measures related to activities of daily living, two measures related to patient medical emergencies, and one measure related to improvement in mental health.
What does quality care mean?
Quality care means doing the right thing, at the right time, in theright way, for the right person, and having the best possible results.Home health agenciesare certified to make sure they meet certainFederal health and safety requirements. To find out how home healthagencies compare in quality, look at www.medicare.gov on the web.Select “Home Health Compare.”
What is a pay per visit plan?
pay-per-visit health plan that lets yougo to any doctor, hospital, or otherhealth care provider who acceptsMedicare. You must pay the deductible.Medicare pays its share of the Medicare-approved amount, and you pay yourshare (coinsurance). The OriginalMedicare Plan has two parts: Part A(hospital insurance) and Part B (medical insurance).
What to do if you have no HHA?
If no HHA in your area can provide you with care, speak to your doctor about other options for receiving care. If you need information about the costs and coverage rules for home health care, or if you are experiencing problems, contact your Medicare Advantage Plan.
Does Medicare Advantage cover home health?
All Medicare Advantage Plans must provide at least the same level of home health care coverage as Original Medicare, but they may impose different rules, restrictions, and costs. Depending on your plan, you may need to: Get care from a home health agency (HHA) that contracts with your plan.
How long does it take for a home health aide to be certified?
After a physician or allowed practitioner prescribes a home health plan of care, the HHA assesses the patient's condition and determines the skilled nursing care, therapy, medical social services and home health aide service needs, at the beginning of the 60-day certification period. The assessment must be done for each subsequent 60-day certification. A nurse or therapist from the HHA uses the Outcome and Assessment Information Set (OASIS) instrument to assess the patient's condition. (All HHAs have been using OASIS since July 19, 1999.)
When did the Home Health PPS rule become effective?
Effective October 1, 2000, the home health PPS (HH PPS) replaced the IPS for all home health agencies (HHAs). The PPS proposed rule was published on October 28, 1999, with a 60-day public comment period, and the final rule was published on July 3, 2000. Beginning in October 2000, HHAs were paid under the HH PPS for 60-day episodes ...
How are HHAs paid?
Beginning on January 1 2020, HHAs are paid a national, standardized 30-day period payment rate if a period of care meets a certain threshold of home health visits. This payment rate is adjusted for case-mix and geographic differences in wages. 30-day periods of care that do not meet the visit threshold are paid a per-visit payment rate for the discipline providing care. While the unit of payment for home health services is currently a 30-day period payment rate, there are no changes to timeframes for re-certifying eligibility and reviewing the home health plan of care, both of which will occur every 60-days (or in the case of updates to the plan of care, more often as the patient’s condition warrants).
What is included in the HH PPS?
For individuals under a home health plan of care, payment for all services (nursing, therapy, home health aides and medical social services) and routine and non-routine medical supplies, with the exception of certain injectable osteoporosis drugs, DME, and furnishing negative pressure wound therapy (NPWT) using a disposable device is included in the HH PPS base payment rates. HHAs must provide the covered home health services (except DME) either directly or under arrangement, and must bill for such covered home health services.
What is PPS in home health?
The Balanced Budget Act (BBA) of 1997, as amended by the Omnibus Consolidated and Emergency Supplemental Appropriations Act (OCESAA) of 1999, called for the development and implementation of a prospective payment system (PPS) for Medicare home health services.
Is telecommunications technology included in a home health plan?
In response CMS amended § 409.43 (a), allowing the use of telecommunications technology to be included as part of the home health plan of care, as long as the use of such technology does not substitute for an in-person visit ordered on the plan of care.