If you choose coverage under the employer group health plan and are still working, Medicare will be the secondary payer, which means the employer plan pays first. If the employer group health plan does not pay all the patients expenses, Medicare may pay the entire balance, a portion, or nothing.
Full Answer
What is the best secondary insurance with Medicare?
- Vision: Your medical plan will not cover you for vision care. ...
- Dental: A dental plan can cover you for preventive care such as routine teeth cleanings and some X-rays. ...
- Disability: Short- and long-term disability plans are a type of secondary insurance coverage. ...
Does Medicare automatically Bill secondary insurance?
Medicare usually covers most of your healthcare costs, but if you have other insurance coverage, it can act as a secondary payer for some of the costs.
How does Medicare work when it is a secondary insurance?
- You will always have the choice of keeping your employer health insurance when you are eligible for Medicare if you work for a large company
- Depending on the size of your company, Medicare may be your primary or secondary insurance
- Medicare also works with COBRA, TRICARE, VA benefits, and HRAs
Is Medicare ever used as a secondary insurance carrier?
You can still get Medicare if you’re insured by a private company, but there are some occasions when Medicare becomes the secondary payer for your benefits. Being a “secondary payer” means that Medicare is second-in-line to paying your healthcare claims.
Is Medicare Part A primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Can you have double coverage with Medicare?
Some people who continue to work past age 65 may also have group health plan benefits through their employer. Because of this, it's possible to have both Medicare and a group health plan after age 65.
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Does Medicare pay deductible as a secondary insurance?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
Will Medicare pay secondary if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
Does Medicare Secondary cover primary copays?
Medicare is often the primary payer when working with other insurance plans. A primary payer is the insurer that pays a healthcare bill first. A secondary payer covers remaining costs, such as coinsurances or copayments.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Can my employer pay for my Medicare premiums?
Can my employer pay my Medicare premiums? Employers can't pay employees' Medicare premiums directly. However, they can designate funds for workers to apply for health insurance coverage and premium payments with a Section 105 plan.
How do deductibles work with two insurances?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
What is Medicare Secondary Payer Rule?
Generally the Medicare Secondary Payer rules prohibit employers with 20 or more employees from in any way incentivizing an active employee age 65 or older to elect Medicare instead of the group health plan, which includes offering a financial incentive.
How does Medicare Secondary Payer work?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
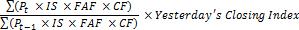
How much is Medicare fee schedule?
The Medicare fee schedule amount is $185, and no Medicare benefits are payable. The patient can be billed for the remaining $110, and $185 would go toward the Part B deductible. A patient has a $185 deductible, which he or she has paid $50 toward. He or she incurred $100 in charges, which the primary payer paid in full.
Do you have to ship a claim off to the primary payer?
Similar to any other scenario involving primary and secondary payers, you’ll need to ship the claim off to the primary payer first. Only once you’ve received an Explanation of Benefits (EOB) from the primary insurance can you attempt to bill Medicare.
Does Medicare cover the cost of a service?
That said, according to CMS, if the primary payer does not provide prompt payment (and you can provide evidence of this), Medicare will temporarily cover the cost of any service the primary insurance would typically reimburse.
Does Medicare credit deductibles?
In other words, Medicare will credit any amount paid by the primary insurance up to the amount allowed by the Medicare fee schedule toward the deductible. Here are a couple of examples: Say a patient’s deductible is $185, which he or she has not yet met.
Can Medicare and other insurances work together?
And for Medicare patients with other health insurance providers, few things are better than when Medicare and their private payers work together cooperatively. However, Medicare has a lot of unique rules, which means providers should tread carefully when their patients have Medicare and a second insurance. To that end, here’s a rundown of all the things PTs, OTs, and SLPs need to know about Medicare as a secondary payer:
Is Medicare a secondary insurance?
This first part is often where things go awry: Medicare functions differently depending on the other types of insurance benefits the patient receive s (i.e., Medicare always functions as the secondary in some instances).
Do Medicare patients have to pay deductibles?
As CMS explains in the Medicare Secondary Payer Manual, patients will likely still have to make payments toward their deductibles, which “are credited to those deductibles even if the expenses are reimbursed by a [group health plan].”.
How does Medicare work with insurance carriers?
Generally, a Medicare recipient’s health care providers and health insurance carriers work together to coordinate benefits and coverage rules with Medicare. However, it’s important to understand when Medicare acts as the secondary payer if there are choices made on your part that can change how this coordination happens.
Who is responsible for making sure their primary payer reimburses Medicare?
Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment. Medicare recipients are also responsible for responding to any claims communications from Medicare in order to ensure their coordination of benefits proceeds seamlessly.
What is ESRD covered by?
Diagnosed with End-Stage Renal Disease (ESRD) and covered by a group health plan or COBRA plan; Medicare becomes the primary payer after a 30-day coordination period.
What does a primary payer do?
In the simplest of terms, a primary payer will cover the cost of a health care bill according to its policy rules and up to the limit established therein.
How old do you have to be to be covered by a group health plan?
Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 20 employees between them.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Who is covered by an employment-related group health plan?
Disabled and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 100 employees between them.
How does secondary insurance work?
How Secondary Insurance Works. When you have two insurance policies that cover the same kinds of risks, one of them is primary and the other is secondary. For example, suppose you have Medicare along with Medigap Plan G. Medicare will be your primary health insurance, and the Medigap plan is secondary. If you go to the doctor, Plan G will cover the ...
Why does Medicare not cover everything?
Because Medicare doesn’t cover everything, these policies are available to fill in the gaps. This helps reduce costs. Most states offer 12 different plan options, with varying levels of coverage. Each plan is subject to federal regulations, ensuring that the benefits are the same regardless of the carrier.
Why do you need a supplement insurance policy?
Because Medicare pays first, it is primary. But , Medicare doesn’t pay for everything. So, a Supplemental policy is beneficial to have in place to protect you from unexpected medical costs. If you’re looking for the best secondary insurance with Medicare, it’s wise to become familiar with what each Medigap plan includes.
What is supplemental insurance?
Supplemental insurance is available for what doesn’t get coverage. For example, Part D is drug coverage, which is supplemental insurance. Dental, vision, and hearing policies are also available for purchase to supplement your existing coverage. Yet, these policies stand on their own and are not primary or secondary insurance.
Is Medigap a secondary insurance?
Medigap is not the only type of insurance that can be secondary to Medicare. For example, those with TRICARE For Life have TFL as their secondary plan. A series of rules known as the coordination of benefits decides the order of payment in each case. Sometimes, although rarely, there can be up to three payers.
Is Medicare a primary or secondary plan?
Primary vs. Secondary Medicare Plans. Medicare is primary to a Supplement plan because it pays first. After reaching the limit, your Medigap plan will pay second. Often, secondary insurance will not pay if the primary insurance doesn’t pay. Medigap is not the only type of insurance that can be secondary to Medicare.
Is Medicare secondary to employer?
What is Secondary Insurance to Employer Coverage. Medicare recipients who are still working might have a large employer group health plan. In this case, Medicare is secondary to the employer plan. It’s also possible to delay Part B if you reach age 65 and have creditable coverage through your employer.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What are the responsibilities of an employer under MSP?
As an employer, you must: Ensure that your plans identify those individuals to whom the MSP requirement applies; Ensure that your plans provide for proper primary payments whereby law Medicare is the secondary payer; and.
What is the purpose of MSP?
The MSP provisions have protected Medicare Trust Funds by ensuring that Medicare does not pay for items and services that certain health insurance or coverage is primarily responsible for paying. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage.
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
How to check if Medicare is your primary or secondary policy?
If you’re not sure whether Medicare is your primary or secondary policy, you can check in with your private insurer, or call Medicare’s Benefits Coordination & Recovery Center (BRCR) at 1-855-798-2627 (TTY: 1-855-797-2627 ).
When do you have to buy Medicare?
If you get health insurance through an employer (either yours or your spouse’s) that has fewer than 20 workers, you’ll have to purchase Medicare when you turn 65, and that will be your primary coverage.
What factors affect your decision to keep or drop private insurance?
These factors include whether your spouse has employer coverage and whether you have “creditable drug coverage” — prescription drug coverage that meets Medicare’s minimum standards. Below, we break down what you need to know about how Medicare can work with other insurance plans and how to get the most out of a combination of insurance payers.
How long does it take to sign up for Medicare after you end your health insurance?
Once you end your private health insurance, you’ll enter Medicare’s 8-month special enrollment period, and you’ll have to sign up promptly to avoid penalties.
Does Medicare pay first if you work for a small company?
However, if you work for a small company or get health insurance from a former employer, Medicare pays first.
Is Medicare a primary or secondary insurance?
Typically, whether Medicare is primary or secondary to your existing insurance will depend on how you get your other insurance policy. If you work for a large employer (more than 20 employees), your workplace insurance is your primary policy. The same rule applies if you get insurance through your spouse’s large employer. Similarly, if you’re on active-duty military and get insurance through Tricare, Medicare will be secondary.
Is private insurance primary or secondary to Medicare?
If you have health insurance in addition to Medicare, your private policy is either the primary payer or it is secondary to Medicare.
What is secondary insurance?
A separate plan that offers additional benefits is called secondary insurance. Your secondary health insurance can be another medical plan, such as through your spouse. More often, it’s a different type of plan you’ve purchased to extend your coverage. In that case, you may hear it referred to as voluntary or supplemental coverage .
What is hospital indemnity insurance?
Hospital indemnity insurance provides cash payments to help you manage the costs of a hospital stay, from your deductible to everyday expenses like daycare. If an injury or illness prevents you from working, disability insurance provides you with income on a weekly or monthly basis so you can still pay for your day-to-day expenses.
Does primary insurance cover lab tests?
As you probably know , your primary health insurance covers your basic medical expenses like doctors’ visits, lab tests and prescription drugs ― as well as some great perks . But your medical plan can’t cover everything. A separate plan that offers additional benefits is called secondary insurance. Your secondary health insurance can be another ...
Does my medical plan cover everything?
Your medical plan will cover many expenses, but it won't cover everything. So, you may want special policies to help cover those extra costs.
Do different people need different supplemental plans?
Different people need different supplemental plans, depending on their circumstances . Below, you’ll read how Peggy, Cecilia, DeWayne and Kevin use special policies to prepare for the unexpected financial and health challenges life sends their way.
What is a dual eligible Medicare beneficiary?
Dual-eligible beneficiaries are often automatically enrolled in a Medicare Savings Program (MSP), which covers the Medicare Part B premium and may offer additional services.
What type of insurance is ordered to pay for care before Medicaid?
Some of the coverage types that may be ordered to pay for care before Medicaid include: Group health plans. Self-insured plans. Managed care organizations. Pharmacy benefit managers. Medicare. Court-ordered health coverage. Settlements from a liability insurer. Workers’ compensation.
What is third party liability?
Third party liability. Under federal law, all other sources of health care coverage must pay claims first before Medicaid will pick up any share of the cost of care. This is referred to as “third party liability” (TPL), which means the primary payment for care is the responsibility of any available third-party resources and not that of Medicaid.
What is a D-SNP?
There are certain types of Medicare Advantage plans known as Dual-eligible Special Needs Plans (D-SNP) that are custom built to accommodate the specific needs of those on both Medicare and Medicaid.
Can you be on Medicare and Medicaid at the same time?
Some people are eligible for both Medicare and Medicaid and can be enrolled in both programs at the same time. These beneficiaries are described as being “dual eligible.”.
Is medicaid a primary or secondary insurance?
Medicaid can work as both a primary or secondary insurer. In this Medicaid review, we explore when and how the program works as secondary, or supplemental, insurance that can coordinate with other types of insurance.
Does Medicare pick up coinsurance?
Copayments and coinsurances that are left remaining after Medicare applies its coverage will be picked up by Medicaid. Dual-eligible beneficiaries can expect to pay little to nothing out of their own pocket after Medicaid has picked up its share of the cost.
What does secondary insurance cover?
The secondary health insurance payer covers bills that the primary insurance payer didn’t cover.
What does it mean to have two health insurance plans?
Having two health plans can help cover normally out-of-pocket medical expenses, but also means you'll likely have to pay two premiums and face two deductibles.
What is the most common example of carrying two health insurance plans?
The most common example of carrying two health insurance plans is Medicare recipients, who also have a supplemental health insurance policy, says David Mordo, former national legislative chair and current regional vice president for the National Association of Health Underwriters.
What are some examples of two insurance plans?
Other examples of when you might have two insurance plans include: An injured worker who qualifies for worker's compensation but also has his or her own insurance coverage. A military veteran who is covered by both Veterans Administration benefits and his or her own health plan. An active member of the military who is covered both by military ...
What is the process of coordinating health insurance?
That way, both health plans pay their fair share without paying more than 100% of the medical costs. This process is called coordination of benefits.
Who pays the medical bill?
The primary insurance payer is the insurance company responsible for paying the claim first. When you receive health care services, the primary payer pays your medical bills up to the coverage limits. The secondary payer then reviews the remaining bill and picks up its portion.
Can a married couple have two health insurance plans?
It’s also possible that a married couple could have two health insurance plans, even if each spouse is covered through a health insurance plan at their workplace. “They’re both covered under their own policies with their companies, but one of the spouses decides to (also) jump on their spouse’s plan,” Mordo says.
What is secondary insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance.
Why combine secondary insurance with cheap insurance?
Combining secondary health insurance with a cheap health insurance plan can help you pay less for broad coverage that would be more expensive if you purchased only one plan.
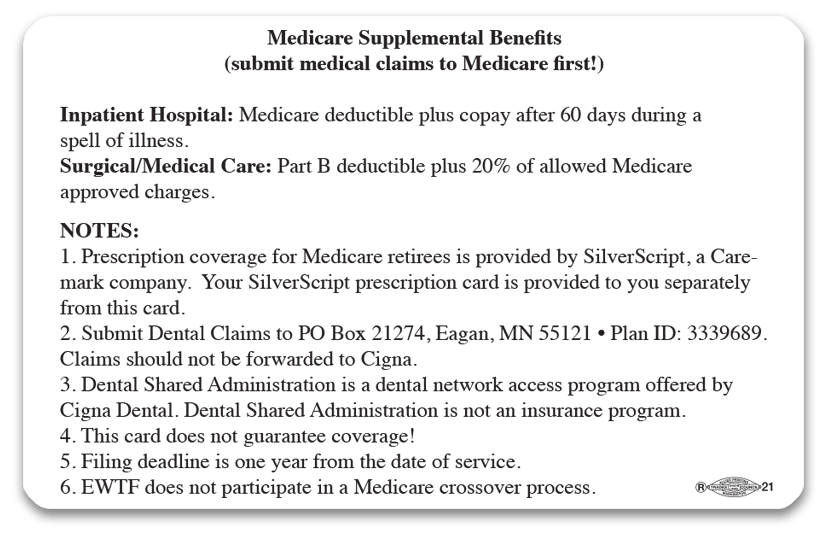
What is Medicare Supplemental Insurance?
Medicare supplemental insurance: Also called Medigap plans, these supplemental plans can help cover services that are not covered by Original Medicare. Plans can also help pay your out-of-pocket costs for deductibles, copayments and coinsurance.
How much does Medicare supplement cost?
The cost of Medicare supplement plans has the biggest range because of the variety of plans and coverage options. Low-cost plans such as Plan K start at just $62 per month, and other choices such as Plan A or Plan B can cost more than $700 per month.
How much does secondary health insurance cost?
Secondary health insurance can cost anywhere from $5 per month to hundreds of dollars per month, depending on the type of coverage and the level of support the plan provides.
What happens if you have multiple insurance policies?
If you have multiple insurance policies, there is a clear order in which the plans will pay for health care services.
What is gap insurance?
Gap health insurance: Sometimes called limited benefits plans, these policies usually give you a lump-sum payment for covered illnesses or injuries, and you can use the payments to offset your out-of-pocket costs such as deductibles or copayments.
