- You can use the enrollment check at Medicare.gov
- You can check the status online at http://www.mymedicare.gov
- You can call Medicare at 1-800-633-4227
- Members can visit a local office to review the coverage in person
How do I Check my Medicare benefits?
Your Medicare Benefits The information in “Your Medicare Benefits” describes the Medicare Program at the time it was printed. Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. “Your Medicare Benefits” isn’t a legal document.
How can providers verify Medicare eligibility?
- Medicare ID number (known as the Medicare Beneficiary Identifier (MBI))
- Last Name
- First Name
- Gender (M/F)
- Date of Birth (MMDDCCYY format)
- Eligibility From date / date of service (MMDDCCYY format)
- Eligibility Thru date / date of service or current date (MMDDCCYY format)
How do you check out your Medicare coverage?
- You can use the enrollment check at Medicare.gov
- You can check the status online at http://www.mymedicare.gov
- You can call Medicare at 1-800-633-4227
- Members can visit a local office to review the coverage in person
How do you verify Medicare coverage?
Medicare coverage could do better by removing financial barriers to ... Medicare can cover a range of healthcare services like hospital stays, preventive check-ups, and prescription drugs. “We really need to prioritize mental health,” Gunja added ...
How do I verify my Medicare coverage?
Checking the BasicsYou can use the enrollment check at Medicare.gov.You can call Medicare at 1-800-633-4227.Members can visit a local office to review the coverage in person.
How do I get proof of Medicare payments?
The easiest receipt for you to use as proof of eligible expenses is the annual statement you receive from Social Security for the upcoming calendar year.
How do I know if my Medicare deductible has been met?
Deductibles for Original Medicare You can find out if you've met your Medicare Part A or Part B deductible for the year at MyMedicare.gov.
What is Medicare proof?
Evidence of Coverage (EOC) is a notice you receive from your Medicare Advantage or Part D plan in late September. It lists the plan's costs and benefits that will take effect on January 1 of the upcoming year. Review the EOC to see if the plan will meet your health care needs in the next year.
How do you find evidence of coverage?
Go to the Benefits and coverage plan resources page to view and download your EOC/COI (not available to all members). Contact your Human Resource department for a copy if you have health care through your company. Contact Us and request that a copy be mailed to you.
Can I get my Medicare Summary Notice Online?
Yes, Medicare summary notices are available online — but you must sign up to receive them electronically. If you opt for electronic notices, you'll stop receiving printed copies of your MSNs in the mail. Instead, you'll get an email every month from your online My Medicare Account.
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
What is the deductible for Medicare 2021?
The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Did I meet my deductible?
For example, if you have a $2,000 health care deductible, you're responsible for paying for all of your health and medical expenses until you reach that $2,000 mark. When you hit that mark, you've met your deductible.
Do you get a 1095 for Medicare?
If you were enrolled in Medicare: For the entire year, your insurance provider will not send a 1095 form. Retirees that are age 65 and older, and who are on Medicare, may receive instructions from Medicare about how to report their health insurance coverage.
What can be used as proof of health insurance?
Insurance cards. Explanation of benefits. W-2 or payroll statements that show insurance deductions. Records or advance payments of the premium tax credit and other statements indicating that the taxpayer or a member of his or her family had health coverage.
What is evidence of coverage for health insurance?
What is Evidence of Coverage? A. The Evidence of Coverage (EOC) is a document that describes in detail the health care benefits covered by the health plan. It provides documentation of what that plan covers and how it works, including how much you pay.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
What is a benefit verification letter?
The Benefit Verification letter, sometimes called a "budget letter," a "benefits letter," a "proof of income letter," or a "proof of award letter," serves as proof of your retirement, disability, Supplemental Security Income (SSI), or Medicare benefits.
How to get a Social Security verification letter?
If you have questions or need help understanding how to request your benefit verification letter online, call our toll-free number at 1-800-772-1213 or visit your Social Security office. If you are deaf or hard of hearing, call our toll-free TTY number, 1-800-325-0778, between 8:00 a.m. and 5:30 p.m. Monday through Friday.
What can I use my Social Security letter for?
You may use your letter for loans, housing assistance, mortgage, and for other income verification purposes. You can also use it to prove that you don't receive benefits, have applied for benefits, or that you have never received Social Security benefits or SSI.
How long does it take to create a Social Security account?
Creating a free my Social Security account takes less than 10 minutes, lets you download or print your benefit verification letter, and gives you access to many other online services.
What are the benefits of Medicare Advantage?
Most Medicare Advantage plans offer additional benefits not covered by Original Medicare, such as dental, vision and prescription drug coverage. Medicare Part D provides coverage for prescription medications, which is something not typically covered by Original Medicare.
What is Medicare Part A?
Medicare Part A provides coverage for inpatient hospital stays. Every Medicare beneficiary will typically have Part A.
How long does Medicare AEP last?
The Medicare AEP lasts from October 15 to December 7 every year. During this time, Medicare beneficiaries may do any of the following: Change from Original Medicare to a Medicare Advantage plan. Change from Medicare Advantage back to Original Medicare. Switch from one Medicare Advantage plan to another.
What is an annual review of Medicare?
An annual review of your Medicare coverage can help you determine if your plan combination is right for your needs. For example, if you’re spending a considerable amount of money on prescription drugs, a Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage may be something to consider.
Can you lose track of Medicare?
With so many different types of Medicare plans available, you could easily lose track of which plan (or plans) you have. So how do you quickly find out what type of Medicare plan you have?
Is Medicare Part A and Part B the same?
Part A and Part B are known together as “Original Medicare.”. Medicare Part C, also known as Medicare Advantage, provides all the same benefits as Medicare Part A and Part B combined into a single plan sold by a private insurance company.
What is the first step in Medicare billing?
Checking Beneficiary Eligibility. To ensure the accuracy and appropriate billing of Medicare covered home health and hospice services, the first vital step is to check a beneficiary's eligibility.
What is myCGS?
myCGS – A CGS web portal that provides eligibility information based on the HIPAA 270/271 transaction.
Is CMS discontinuing CWF?
NOTE: In December 2012, CMS announced plans to discontinue the CWF Beneficiar y eligibility transactions (MLN Matters Special Edition article SE1249 ). In that same article, CMS announced that the HETS would be the single source for this data. If you currently use CWF queries (HIQA, HIQH, ELGA, and ELGH) to obtain Medicare eligibility information, you should begin using HETS.
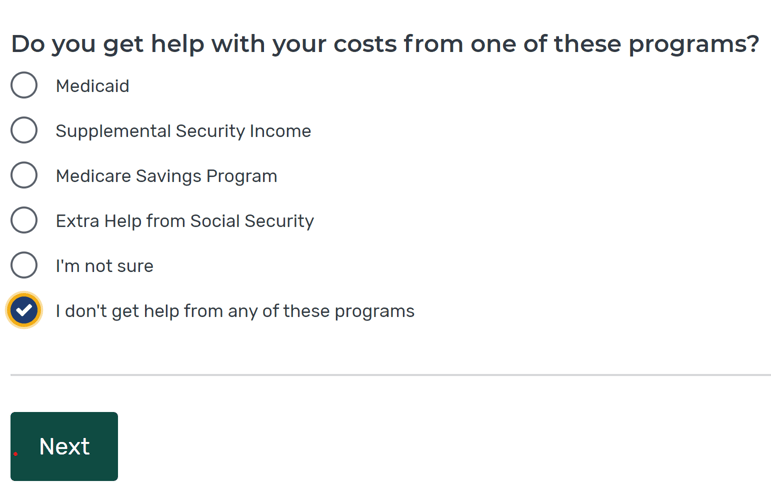
How to check if you are eligible for Medicare?
To check your Medicare eligibility online, go to Medicare.gov at this link and complete the series of questions. It is important that you answer them accurately to find out if you are eligible.
How to check Medicare enrollment status?
To check your Medicare enrollment status online, visit Medicare.gov at this link. Enter your information, then click “continue.” You will need your Medicare card for your Medicare number. You won’t be able to continue until you’ve answered all the questions.
How else can I Check my Benefits?
You can also visit your local Social Security or other government offices to ask about benefits in person.
How to check my medicaid status?
Checking your Medicaid status online isn’t quite as easy as Medicare because Medicaid is different in every state. Your state might have its own application portal where you can track the status of your application and find out more about your benefits. You can also visit your local Medicaid office (usually a Social Security building or another government office) or call to check your application status, but know that it could take a few weeks.
What is benefits checkup?
BenefitsCheckUp is a free financial and healthcare benefits check up tool offered by the National Council on Aging. They scan over 2,500 federal, state, and private benefits programs for eligibility standards to keep their tool up-to-date. When you visit benefitscheckup.org and click on “Find My Benefits,” you’ll get results for all the programs that you might be eligible for based on your:
What if I don't qualify for Social Security?
If you don’t qualify for Social Security retirement benefits, you might instead qualify for SSI, or Social Security Income. To qualify for SSI, you must be either blind, disabled, or over the age of 65, and you must have limited income and resources. Qualifying for SSDI (Social Security Disability Income) is different. SSDI eligibility is based on means, severity, and work. That means you must have low income due to your disability/inability to work substantially, a severe disability, and must be incapable of working and earning a livable income. If you receive SSDI for at least 25 months, you may also qualify for Medicare (even if you re under 65).
How long do you have to work to get Social Security?
Social Security benefits can begin when you retire. To be eligible for Social Security retirement benefits, you must have worked for at least ten years. The longer you’ve worked, the higher your benefit can be. For example, if you wait until you are age 70 to retire, your benefit may be higher than if you retire at age 62.