
How to confirm patient details
- Select the find a patient tile.
- Select Medicare card details from the use dropdown menu.
- Enter patient details using Medicare data.
- By accessing this service you’re confirming that you’ve obtained the patient’s consent to search for or confirm their Medicare card details for claiming purposes only. ...
Full Answer
When should I verify patient eligibility?
You can use all online tools and services to get eligibility information. Enter your patient’s: Medicare Beneficiary Identifier (MBI) First and last name Date of birth (MM/DD/YYYY) When the information matches a Medicare record, we’ll return information like: For a Medicare Advantage enrollee, the eligibility response shows the patient’s Medicare Advantage plan, plan
How to check for patient eligibility?
Mar 28, 2022 · Information Needed To Check Medicare Eligibility. One must provide identification, and this includes a full name, address, date of birth, and Social Security number. Some questions may involve the work history of the spouse or partner to see if one or both may be eligible for Social Security benefits and Medicare.
How to check Medicare eligibility as a provider?
Ask your patients for their current member ID card. If they don’t have one, you can verify their eligibility using their full first and last name and date of birth. In addition, you can print an electronic copy of a patient’s ID card, if needed. Make sure that eligibility details match the patient’s information.
Where to check Medicare eligibility?
With Medicare Advantage Recursive Medicare Verification, pVerify will first verify a patient’s full Medicare Coverage (with Medicare MBI or SSN/HICN by including the Medicare MBI Lookup Feature). If a Medicare Advantage Payer is present pVerify will verify the Medicare Advantage Plan using human-enabled AI, machine learning, and our proprietary methods.
How do you verify a patient is eligible for Medicare?
The best way to check eligibility and enroll in Medicare online is to use the Social Security or Medicare websites. They are government portals for signing up for Medicare, and they offer free information about eligibility.
What is Medicare verification?
The Covered CA application, known as CalHEERS, will now electronically verify an applicant's Medicare eligibility and enrollment. Previously, when the question on the application asked if you are currently enrolled in Medicare or receiving Medicare benefits, it would allow you to self-attest your answer.Sep 1, 2016
How do I check my Medicare status?
How Do I Check the Status of My Medicare Enrollment? The status of your medical enrollment can be checked online through your My Social Security or MyMedicare.gov accounts. You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office.
Does Medicare call you to verify information?
Medicare will never call you to update your information or give you a new ID card. If anyone calls to collect your information, don't provide it to them. A phone call like this is a scam.
Self-Batch Eligibility
pVerify now offers a Self-Batch Eligibility Feature for all Premium clients. Created to report extensive Medicare patient benefits, all information available in a single patient verification is available in the batch processing. With no volume limit, verify Medicare patients in mass and view in the color-coded Excel file.
Contact us to create your account today!
Meet with a pVerify Representative to access your current Medicare Patient Eligibility Verification Solution to determine the best combination of pVerify’s Eligibility Solutions for your needs.
Create your own Hybrid Solutions Combination
pVerify is the only company to offer hybrid combinations of Online Portal Features, First-Class Batch Processing, White-labeled API Integrations, and more.
More Medicare Solutions
pVerify’s Same or Similar allows users to review a patient’s 5-year Claim History in near real-time with interpretation flags for easy and actionable decisions.
Eligibility Benefits
This inquiry allows users to view a beneficiary's Medicare eligibility: Part A, Part B, Health Maintenance Organization (HMO) and Managed Care Organization (MCO), Medicare Secondary Payer (MSP), Home Health, Hospice, End Stage Renal Disease (ESRD), Preventive Services and Medicare Diabetes Prevention Program (MDPP).
Response
If the beneficiary is enrolled as a Qualified Medicare Beneficiary (QMB), a green banner will display letting the user know that the beneficiary is a QMB enrollee for one or more Part B Benefit Periods.
What is Medicare entitlement?
Medicare is a Health Insurance Program for people age 65 or older, certain qualified disabled people under age 65, and people of all ages with end-stage renal disease (ESRD) (permanent kidney failure treated with dialysis or a transplant).
What is a CWF?
Common Working File (CWF) is a system that contains all Medicare beneficiary information as well as claim transactions, which includes Medicare Part A, Part B and Durable Medical Equipment. The Fiscal Intermediary Standard System and Multi-Carrier System processing systems interface with CWF to process claims.
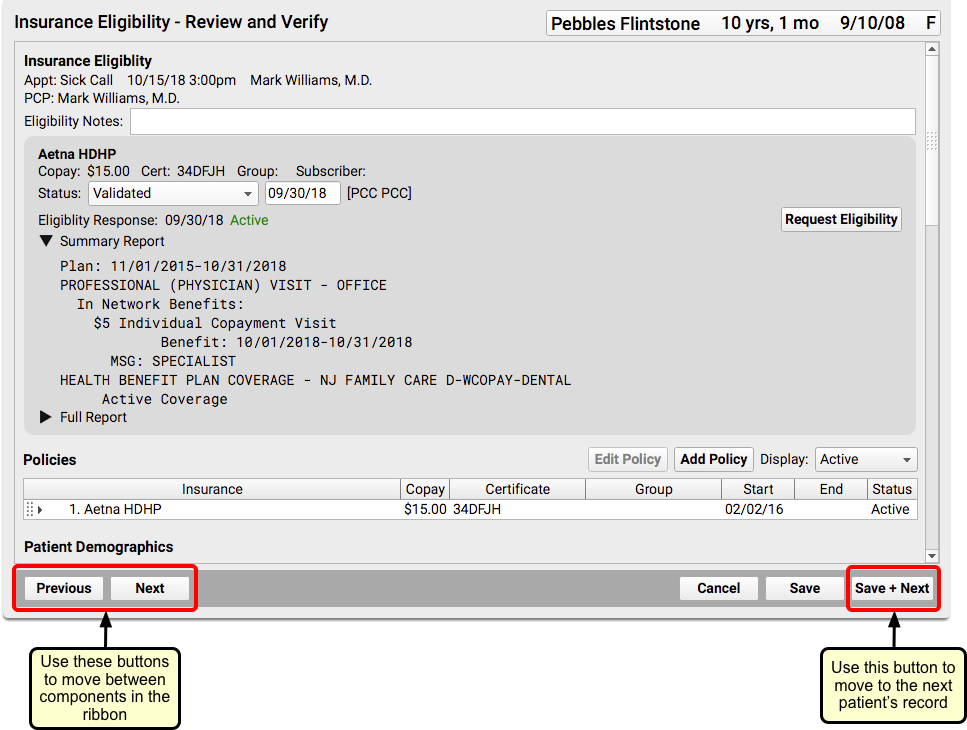
How to Verify Patient Eligibility
Medicare requires providers use self-service technology for inquiries regarding patient eligibility. Our call center staff is not able to respond to these inquiries. Providers can use the WPS Government Health Administrators Portal or our Interactive Voice Response (IVR) system to verify patient eligibility.
Checking Eligibility for Qualified Medicare Beneficiaries (QMB)
When using the portal or IVR to check eligibility, you will not receive information regarding Medicare applied deductible or coinsurance for patients in the QMB program. The portal will return information explaining the patient is part of the QMB program. For more information on the QMB program, see Qualified Medicare Beneficiary (QMB) Program.
Medicare Secondary Payer (MSP) and Eligibility
Although we process Medicare Secondary Payer (MSP) claims, we do not maintain MSP records. The Benefits Coordination & Recovery Center (BCRC) is responsible for establishing MSP occurrence records on the Common Working File (CWF).
