
Full Answer
Can I appeal a Medicare SNF claim?
Jan 19, 2020 · Medicare only covers 100 days of continuous skilled nursing, so just be aware that appealing for time beyond the 100 days is generally a lost cause. If her stay is under 100 days and your appeal is that the therapy is required to return her to normal or at least to the state that she was in before, then there is a better chance for that – try to document if you can that the …
What is a fast appeal for Medicare?
Feb 12, 2013 · A Medicare SNF claim suitable for appeal should meet the following criteria: The patient must have been hospitalized as an inpatient for at least three days (not including day of discharge), and, in most cases, must have been admitted to the SNF within 30 days of hospital discharge. A physician must certify that the patient needs SNF care.
How do I appeal a decision about a skilled nursing facility?
Jan 21, 2021 · To file an appeal against an original Medicare decision, a person can complete a Redetermination Request Form and mail it to the company listed in the Appeals Information part of the MSN. Another...
How do I appeal a Medicare decision?
Request care and ask the SNF or HHA to bill Medicare ( demand bill ). If Medicare denies coverage, you have the right to file an appeal. If your appeal is unsuccessful, you may be responsible for the cost of care. A SNF or HHA may refuse to demand bill. Request care but agree to pay for the care out of pocket. Turn down care.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
How do I fight Medicare denial?
If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
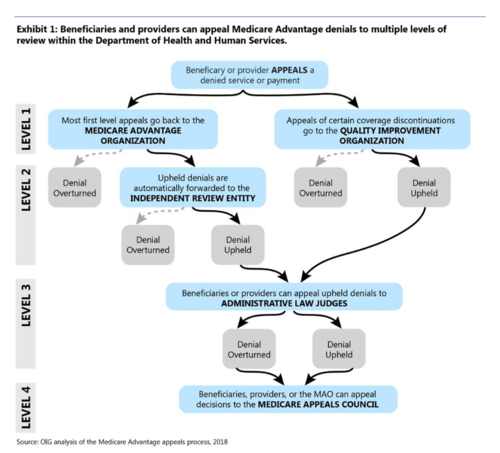
What are the five levels of appeal for Medicare claims processing?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What is the highest level of Medicare appeal?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
Who pays if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
What is first level appeal?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination.Dec 1, 2021
What happens when Medicare denies a claim?
If Medicare refuses to pay for something, they send you a “denial” letter. The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
What is the first level of the Medicare appeals process?
redeterminationAppeal the claims decision. The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
What are Medicare appeals?
If you disagree with a Medicare coverage or payment decision, you can appeal the decision. This is called a redetermination. Medicare contracts with the MACs to review your appeal request and make a decision.
How long does Maximus take to review an appeal?
Workers Compensation Appeals With the introduction of IMR, disputes are resolved in 2 weeks on average - down from nearly 12 months under the cumbersome court system it replaced.
Why is Medicare denied?
In particular, beneficiaries are often denied coverage because they have certain chronic conditions such as Alzheimer's disease, Parkinson's disease, and Multiple Sclerosis, or because they need nursing or therapy “only” to maintain their condition. Again, these are not legitimate reasons for Medicare denials.
What is Medicare Advocacy?
Medicare is the national health insurance program to which many disabled individuals and most older people are entitled under the Social Security Act.
How long is SNF coverage?
The SNF benefit is available for a short time at best – for up to 100 days during each Medicare benefit period, known as the “ spell of illness .” 42 USC §1395d (a) (2) (A). If Medicare coverage requirements are met, the patient is entitled to full coverage of the first 20 days of SNF care.
What happens if an ALJ issues a favorable decision?
If the ALJ issues an unfavorable decision, you will remain financially responsible for the continued care unless you successfully appeal to the next step, the Medicare Appeals Council. The ALJ’s decision will tell you how to do so.
Does Medicare cover skilled nursing?
Medicare is available for skilled care necessary to maintain an individual’s condition. The question to ask is “does the patient meet the qualifying criteria listed above and need skilled nursing and/or therapy on a daily basis” – NOT “does the patient have a particular disease or will she recover.”
What is Medicare agent?
An agent of the federal government, often an insurance company, which makes Part A Medicare claim determinations for skilled nursing facility and home health coverage, and issues payments to providers.
Does Medicare cover chronic conditions?
Coverage can be available for items and services needed to maintain the person's condition or to arrest or retard further deterioration. Medicare coverage is often erroneously denied for individuals with chronic conditions, for people who are not improving, or who are in need of services to maintain their condition.
What is an appeal in Medicare?
Other program appeals. Winning an appeal. Summary. A person may appeal when Medicare makes a decision that denies coverage of any service. They may have a better chance of winning an appeal if they gather and include supporting information from a doctor or healthcare provider. The appeal process involves five levels.
How long does it take for Medicare to notify you of an appeal?
In all other cases, a person is usually informed of the decision within 60 days of the appeal date. If Medicare decides to cover the service, it will appear on the individual’s next MSN.
How often does Medicare get a summary notice?
A person enrolled in original Medicare — parts A and B — gets a Medicare Summary Notice (MSN) form every 3 months. The MSN lists the services or items that providers billed to Medicare and the amount Medicare paid for each.
What is DME in medical terms?
to cover or pay for a piece of durable medical equipment (DME), healthcare service, or medication. to change the fee that an individual must pay for DME, healthcare service, or medication. A person may also appeal if the decision by Medicare, a health plan, or a drug plan stops payment for all or part of DME, healthcare service, or medication.
What is a fast appeal?
This appeal covers categories that include services from a home health agency, a hospital, a skilled nursing facility, a comprehensive outpatient rehabilitation facility, or a hospice.
How long does it take to appeal a Medicare denial?
The deadline for filing is 60 days from the denial date. They should include the same information required for an original Medicare appeal.
What is a Medicare redetermination?
the individual’s name, address, and Medicare number. the specific service or item, along with the date, in which someone is requesting the redetermination. an explanation of why the person is requesting coverage. any supporting information that may help the case.
Advance Beneficiary Notice Requirements
Mrs. Cleaver did not receive valid notice that could result in the proper termination of services. [NOTE: Dear readers . I am putting some legal citations in here for the benefit of my lawyer and nursing home readers.
How to Make an Expedited Appeal
Had Mrs. Cleaver received a valid written notice of proposed Medicare nursing home discharge, it would have told her that she had until noon the day following her receipt of the notice to lodge an expedited appeal of Medicare termination. 42 CFR § 405.1202 (b) (1). She could fax, or even telephone her appeal, to the number shown on the notice.
What if Mrs. Cleaver disagrees with the QIO?
Mrs. Cleaver can appeal the proposed Medicare nursing home discharge to the Qualified Independent Contractor or “QIC” having oversight authority with respect to QIO decisions. The QIC for the eastern US (which includes both Georgia and North Carolina) is Maximus Federal Services based in Pittsford, New York
What if Mrs. Cleaver Disagrees with the QIC?
The QIC decision will describe what further steps may be taken. At this point, things begin to slow down, and Mrs. Cleaver is no “on the hook” for payments to Mossy Mountain, unless Ward can qualify for Medicaid. There is still some hope.
What happens if Medicare denies coverage?
If Medicare denies coverage, you have the right to file an appeal. If your appeal is unsuccessful, you may be responsible for the cost of care. A SNF or HHA may refuse to demand bill. Request care but agree to pay for the care out of pocket. Turn down care.
What is a SNF notice?
This notice is often called a Skilled Nursing Facility Advance Beneficiary Notice (SNFABN). If you are receiving care from an HHA, you should receive a Home Health Advance Beneficiary Notice (HHABN). Each notice will ask you to choose one of the following three options:
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What is an ABN form?
You may receive a form called an Advance Beneficiary Notice of Noncoverage (ABN). This form usually comes from your healthcare provider and lets you know that you — not Medicare — are responsible for paying for a service or equipment. This notice may have another name, depending on the type of provider it comes from.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take to get a response from Medicare?
You should have a response from the qualified independent contractor within 60 days. If they didn’t decide in your favor, you can ask for a hearing before an administrative law judge or an attorney adjudicator at the Office of Medicare Hearings and Appeals.
Can you appeal a Medicare decision?
You have rights and protections when it comes to Medicare. If you don’t agree with a decision made by original Medicare, your Medicare Advantage plan, or your Medicare Part D prescription drug plan, you can appeal.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if your appeal is denied?
If your appeal is denied, you can make additional appeals. While your first appeal is decided by the same organization that processed the original claim, other appeals are heard by third parties involved in the initial decision. There are five levels of appeals.
How many claims does Medicare process?
Medicare processes more than a billion claims every year, and there will inevitably be mistakes and oversights. Knowing your Medicare rights and protections can help you navigate the health program more easily.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.

Advance Beneficiary Notice Requirements
How to Make An Expedited Appeal
- Had Mrs. Cleaver received a valid written notice of proposed Medicare nursing home discharge, it would have told her that she had until noon the day following her receipt of the notice to lodge an expedited appeal of Medicare termination. 42 CFR § 405.1202(b)(1). She could fax, or even telephone her appeal, to the number shown on the notice. The appeal is given to something calle…
What If Mrs. Cleaver Disagrees with The Qio?
- Mrs. Cleaver can appeal the proposed Medicare nursing home discharge to the Qualified Independent Contractor or “QIC” having oversight authority with respect to QIO decisions. The QIC for the eastern US (which includes both Georgia and North Carolina) is Maximus Federal Services based in Pittsford, New York If Mrs. Cleaver wants to take it to the next step (which I advise if yo…
What If Mrs. Cleaver Disagrees with The QIC?
- The QIC decision will describe what further steps may be taken. At this point, things begin to slow down, and Mrs. Cleaver is no “on the hook” for payments to Mossy Mountain, unless Ward can qualify for Medicaid. There is still some hope. The next appeal level is to an administrative law judge (ALJ). The Bad News: These appeals take much longer and Mrs. Cleaver should probably …