
To file a Medicare appeal or a “redetermination,” here's what you do:
- Look over the notice and circle the items in question and note the reason for the denia.
- Write down the specific service or benefit you are appealing and the reason you believe the benefit or service should be approved, either on the notice or on a separate ...
- Sign it and write down your telephone number and Medicare number. Make a copy.
- Send a copy to the Medicare contractor's address listed on the Medicare Summary Notice.
- Include any other documentation that supports your appeal.
How to properly compose Medicare appeal letter and its sample?
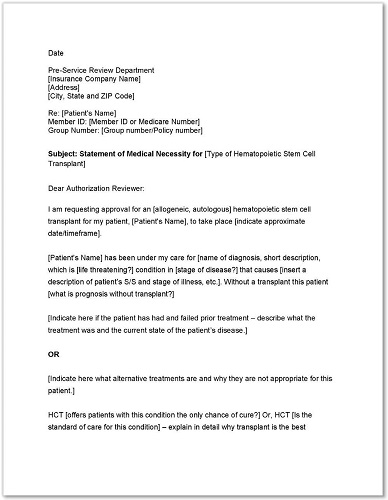
Sample Appeal Letter A. Please accept this letter as [patient's name] appeal to [insurance company name] decision to deny coverage for [state the name of the specific procedure denied]. It is my understanding based on your letter of denial dated [insert date] that this procedure has been denied because: [quote the specific reason for the denial ...
How do you write an insurance appeal letter?
Writing a Health Insurance Appeal Letter (Free Sample)
- Many Procedures are Not covered by insurance. Most people expect everything to be covered after they pay the deductible, but many medical procedures are not covered by insurance.
- Customer Service. ...
- Insurance Company Rules. ...
- certified mail. ...
- Sample Health Insurance Appeal Letter. ...
How to get help when you have problems with Medicare?
What To Do If There Is A Medicare Billing Error, Or You Suspect One Occurred
- It could be an accident. Accidents happen—even with billion-dollar government programs. ...
- Make sure you’re not being scammed. On the other hand, an “accident” could disguise itself as fraud. ...
- Check with Social Security. ...
- Fill out the right form. ...
- Know who is billing you. ...
How do I file an appeal?
You must do all of the following:
- Legibly write or type why you are appealing to the Review Board.
- Sign your name and indicate whether you are the claimant or the employer.
- Be sure to include the case number, your mailing address and your telephone number on all correspondence that you send. ...
How do I write a Medicare appeal letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
How do I win a Medicare appeal?
Appeals with the best chances of winning are those where something was miscoded by a doctor or hospital, or where there is clear evidence that a doctor advised something and the patient followed that advice and then Medicare didn't agree with the doctor's recommendation.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
Can I appeal a Medicare decision?
The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
What are the chances of winning a Medicare appeal?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is Medicare appeal process?
If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim. Level 2: An Independent Organization. If you disagree with the decision in Level 1, you may request a reconsideration by an independent organization. Level 3: Office of Medicare Hearings and Appeals (OMHA).
Which of the following are reasons a claim may be denied?
Here are the top 5 reasons why claims are denied, and how you can avoid these situations.Pre-certification or Authorization Was Required, but Not Obtained. ... Claim Form Errors: Patient Data or Diagnosis / Procedure Codes. ... Claim Was Filed After Insurer's Deadline. ... Insufficient Medical Necessity. ... Use of Out-of-Network Provider.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
How do you handle Medicare denials?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
What is appeal process?
Appeals are decided by panels of three judges working together. The appellant presents legal arguments to the panel, in writing, in a document called a "brief." In the brief, the appellant tries to persuade the judges that the trial court made an error, and that its decision should be reversed.
How many levels of appeal does Medicare have?
Overview - Standard Appeals Process There are five levels in the Medicare Part A and Part B appeals process. The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC)
Who can help you file an appeal for Medicare?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
What is an appeal for home health?
Home Health Care Appeals. Beneficiaries in traditional Medicare have a legal right to an Expedited Appeal when home health providers plan to discharge them or discontinue Medicare-covered skilled care . This right is triggered when the home health agency plans to stop providing skilled therapy and/or nursing.
How to appeal Medicare non coverage?
There are several levels of appeal. The process begins when you receive the “Notice of Medicare Provider Non-Coverage” or “Generic Notice” from your home health agency. 1. Review the “Quick Screen” included in this packet to determine whether the care you need is covered by Medicare. 2. (1st Appeal Level) After you receive the “Notice ...
How to keep Medicare covered?
The best way to keep Medicare covered home health care in place is to exercise your expedited appeal rights. You are most likely to succeed if you have the support of your physician.
What is Medicare agent?
An agent of the federal government, often an insurance company, which makes Part A Medicare claim determinations for skilled nursing facility and home health coverage, and issues payments to providers.
What is Medicare Advocacy?
Medicare is the national health insurance program to which many disabled individuals and most older people are entitled under the Social Security Act.
What is skilled care in home health?
Skilled care is care that must be provided or supervised by a skilled professional in order to be safe and effective.
Is Medicare coverage for home health long term?
Medicare coverage for home health care can be a long-term benefit if the individual meets the qualifying criteria. Unfortunately, however, coverage is often erroneously denied for individuals with chronic conditions, for people who are not improving, who need services for a long time and/or to maintain their condition.
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
What happens if my Medicare plan doesn't decide in my favor?
Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
What to do if Medicare Advantage decision is not in your favor?
In addition, Medicare Advantage companies must give patients a way to report grievances about the plan and the quality of care they receive from providers in the plan.
What happens if you disagree with a Medicare decision?
If you disagree with a decision about one of your Medicare claims, you have the right to challenge that decision and file an appeal. Situations in which you can appeal include: Denials for health care services, supplies or prescriptions that you have already received. For example: During a medical visit your doctor conducts a test.
How to report Medicare not paying?
If you still have questions about a claim you think Medicare should not have paid, report your concerns to the Medicare at 1-800-MEDICARE. Make copies for your records of everything you are submitting. Send the MSN and any additional information to the address listed at the bottom on the last page of your MSN.
Why does Medicare reject my doctor's recommendation?
For example: Your Medicare Part D drug plan rejects your doctor’s recommendation that you receive a discount on an expensive medication because the available lower-cost drugs are not effective for your condition.
When a doctor submits a claim to be reimbursed for that test, what does Medicare determine?
When the doctor submits a claim to be reimbursed for that test, Medicare determines it was not medically necessary and denies payment of the claim. Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition.
Where do third level appeals take place?
Although such third-level appeals usually take place in a conference room and not a courtroom, briefs are filed, evidence is presented and witnesses are called. If the appeal is denied at the third level, it can still be presented to the Medicare Appeals Council, a department within the U.S. Department of Health and Human Services.
What is a fast appeal?
A fast appeal only covers the decision to end services. You may need to start a separate appeals process for any items or services you may have received after the decision to end services. For more information, view the booklet Medicare Appeals . You may be able to stay in the hospital (. coinsurance.
What is your right to be involved in a hospital decision?
Your right to be involved in any decisions that the hospital, your doctor, or anyone else makes about your hospital services and to know who will pay for them. Your right to get the services you need after you leave the hospital. Your right to appeal a discharge decision and the steps for appealing the decision.
What is BCMP in Medicare?
The Beneficiary Care Management Program (BCMP) is a CMS Person and Family Engagement initiative supporting Medicare Fee-for-Service beneficiaries undergoing a discharge appeal, who are experiencing chronic medical conditions requiring lifelong care management. It serves as an enhancement to the existing beneficiary appeals process. This program is not only a resource for Medicare beneficiaries, but extends support for their family members, caregivers and providers as active participants in the provision of health care delivery.
Does Medicare cover hospital admissions?
Medicare will continue to cover your hospital stay as long as medically necessary (except for applicable coinsurance or deductibles) if your plan previously authorized coverage of the inpatient admission, or the inpatient admission was for emergency or urgently needed care.
How long do you have to appeal a medical insurance decision?
Insurance companies are now required to explain the exact reasons they denied your claim. They must also allow you six months to appeal.
What to do if your insurance denied you a medical procedure?
If your health insurance provider has denied payment for a medical procedure, you can write a medical claim appeal letter to ask them to reconsider it. First, call your insurance company and ask them why your coverage was denied.
How to keep notes when speaking to insurance company?
When speaking to your insurance company, keep detailed notes for future use. Write a short summary of the conversation, and keep your notes in the same file as your documentation. Make note of the name of the person you spoke with, his or her job title, and the date and time of the call.
What to do if you aren't sure about your insurance?
If you aren't sure, you may need to verify this with your doctor, your insurance provider, or both. Check your doctor's name and information against your policy to make sure that your insurance company has approved your doctor for coverage. Make sure everything is spelled correctly.
How to identify a case?
Supply your identifying details. Start with your name, address, policy number, claim number, and any other reference numbers you may have collected (through letters or over the phone) that identify your case.
What happens if your insurance company denies a claim?
If your insurance company denied a claim for a procedure that your health care provider deemed necessary, there may be a discrepancy between the wording of your doctor's statement and the wording of your insurance policy's guidelines. Take a copy of your insurance company's guidelines to your doctor's office. ...
What is a medical letter of appeal?
It is the responsibility of a health insurance company to cover for a patient’s medical claim as long as that patient’s coverage is still active. In some cases, however, an insurance company may deny a medical claim and give reasons for doing so.
Can a health insurance company deny a claim?
In the event that a health insurance company denies a medical claim by declaring the claim as not medically necessary, it is your responsibility to write a letter of appeal on behalf of the patient.
Can insurance deny a claim?
A health insurance company may deny a medical claim, making it hard for an insured patient to access medical care. If this ever happens, you will need to write a professional letter to appeal the claim. Here are some examples of medical appeal letter templates that you can download and use.
Can insurance companies deny medical claims?
However, the law requires insurance companies to give an objective reason for denying a medical claim. If the reasons provided are not clear, or less convincing, a patient or their physician can write a professional letter to appeal the decision by the insurance company.
Can an insurance company deny a claim without a reason?
Since the Affordable Care Act increases patients’ rights to appeals, an insurance company cannot deny a claim without providing concrete reasons. Once you understand why the health insurance company denied the claim, it becomes easy to write the medical appeal letter. 5. Printable Medical Letter of Appeal Template PDF.
