
- Submit an online request for Part D prior authorization.
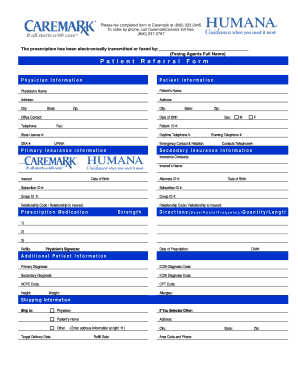
- Download, fill out and fax one of the following forms to 877-486-2621: Request for Medicare Prescription Drug Coverage Determination – English. ...
- Call 800-555-CLIN (2546), Monday – Friday, 8 a.m. – 8 p.m., local time.
See more
Does Medicare do prior authorization?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Is Auth required for Humana?
Not obtaining prior authorization for a service could result in financial penalties for the practice and reduced benefits for the patient, based on the healthcare provider's contract and the patient's Certificate of Coverage.
How do I check my Humana authorization?
Prior authorization for pharmacy drugsElectronic requests: CoverMyMeds® is a free service that allows prescribers to submit and check the status of prior authorization requests electronically for any Humana plan. ... Phone requests: Call 1-800-555-CLIN (2546), Monday – Friday, 8 a.m. – 8 p.m., local time.More items...
What is the prior authorization process?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
How do I submit a prior authorization to Humana?
You can complete your own request in 3 ways:Submit an online request for Part D prior authorization.Download, fill out and fax one of the following forms to 877-486-2621: Request for Medicare Prescription Drug Coverage Determination – English. ... Call 800-555-CLIN (2546), Monday – Friday, 8 a.m. – 8 p.m., local time.
Does Humana Medicare Advantage PPO require referrals?
Unlike an HMO, a PPO offers you the freedom to receive care from any provider—in or out of your network. This means you can see any doctor or specialist, or use any hospital. In addition, PPO plans do not require you to choose a primary care physician (PCP) and do not require referrals.
How can I contact Humana?
(844) 330-7799Humana / Customer service
Does Humana use availity?
Humana uses Availity as its clearinghouse for transacting with health care providers. And, as a payer-owner, Humana continues to collaborate with Availity to develop and improve online tools for health care providers.
Does Medicare require prior authorization for MRI?
Does Medicare require prior authorization for MRI? If the purpose of the MRI is to treat a medical issue, and all providers involved accept Medicare assignment, Part B would cover the inpatient procedure. An Advantage beneficiary might need prior authorization to visit a specialist such as a radiologist.
What happens if you don't get prior authorization?
If you're facing a prior-authorization requirement, also known as a pre-authorization requirement, you must get your health plan's permission before you receive the healthcare service or drug that requires it. If you don't get permission from your health plan, your health insurance won't pay for the service.
What does it mean when a prescription needs prior authorization?
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
Why is prior authorization needed?
Prior Authorizations Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. Prior authorization is usually required if you need a complex treatment or prescription. Coverage will not happen without it.
How to get Humana approval?
How to receive approval. You can start a prior authorization request or ask your doctor to contact Humana Clinical Pharmacy Review (HCPR) for approval. Here are the ways your doctor can request approval: Go to CoverMyMeds to submit a prior authorization request. Call 1-800-555-CLIN (2546), Monday – Friday, 8 a.m. – 8 p.m., local time.
What happens if you fill a prescription without authorization?
Note if your medication requires prior authorization and you fill your prescription without getting approval, you may be responsible for all expenses associated with the medication.
Do you need prior authorization for Humana?
We want to make sure you have the right treatment for your condition, so there may be times when it is necessary to get appro val from Humana before getting a prescription filled. This is called “prior authorization.”
Can you appeal Humana?
You may be able to appeal Humana’s decision if your medication is not approved. To file an appeal, please download and complete the grievance and appeal request form and return it to us.
Can Humana reimburse you for out of pocket expenses?
If you filled a prescription that required prior authorization but did not receive approval from Humana in advance, you may be eligible for reimbursement for your out-of-pocket expense, less any cost share. For reimbursement, please download and complete the Prescription Drug Claim Form and send it to us.
What is a Colorado authorization form?
Colorado authorization form. The use of this form is mandated for prior authorization requests concerning commercial fully insured members: Who reside in the state of Colorado and/or. Whose prescription drug coverage was sold in the state of Colorado. Uniform pharmacy prior authorization request form.
What is a Universal Form for State Mandates?
The use of this form is mandated for prior authorization requests concerning commercial fully insured members: Who reside in Arkansas, Mississippi or Oklahoma and/or. Whose prescription drug coverage was sold in a state listed above. State-specific prior authorization request form.
Can you submit a Humana request electronically?
Prescribers can submit their requests to Humana Clinical Pharmacy Review (HCPR) in the following ways: Electronic requests: CoverMyMeds® is a free service that allows prescribers to submit and check the status of prior authorization requests electronically for any Humana plan.
Does this service require preauthorization?
For certain medical procedures, services, or medications, your doctor or hospital needs advanced approval before your plan covers any of the costs. Visit the Preauthorization and notifications list online. Contact us with questions about “preauthorization” or “notification,” and find out if the services you need are covered in your Humana plan.
Medicare members
Call the number on the back of your Humana member ID card to determine what services and medications require authorization.
How it works
For select services on Humana’s preauthorization list, physicians or their staff now have the option to get faster approvals by answering a few clinical questions online. If all necessary criteria are met, Humana will deliver an instant approval.
Why I should use it
By choosing to complete the short questionnaire, you can streamline the authorization process for patients’ medical services. Even if an online approval is not provided immediately, the information given on the questionnaire will help Humana complete the review more quickly.
Answers that need to be provided
To save time when submitting the authorization, have on hand the relevant clinical information from the patient’s chart, including:
Using this feature
Sign in to the Availity web portal , opens new window and create an authorization request as usual.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
