
If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay. If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare.
When to enroll in Medicare Part A and Part B?
A. Congratulations. You are asking the right questions at the right time. The answers will help you prepare for a smooth entry into Medicare. Most people enroll in Medicare Part A (hospital insurance) and Part B (doctor visits and other outpatient services) during their seven-month initial enrollment period (IEP) around the time they turn 65.
Do I need Medicare Part B If I have other insurance?
Do I Need Medicare Part B if I Have Other Insurance? Many people ask if they should sign up for Medicare Part B when they have other insurance or private insurance. At a large employer with 20 or more employees, your employer plan is primary. Medicare is secondary, so you can delay Part B until you retired if you want to.
When should I enroll in Medicare supplement plans?
For example, if you know you will be retiring on June 30 th, you should enroll in Medicare Parts A and/or B to begin on July 1 st. When you activate your Part B, you will activate your 6-month Medicare supplement open enrollment window. This is your one opportunity to enroll into any Medigap plan without health questions.
Do you have to pay for Medicare if you have group health?
You'll have to pay any costs Medicare or the group health plan doesn't cover. Employers with 20 or more employees must offer current employees 65 and older the same health benefits, under the same conditions, that they offer employees under 65.
Is Part B mandatory on Medicare?
Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary. Part B also covers some preventive services like exams, lab tests, and screening shots to help prevent, find, or manage a medical problem. Cost: If you have Part B, you pay a Part B premium each month.
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Can Medicare Part B be added at any time?
Special Enrollment Period If you are eligible for the Part B SEP, you can enroll in Medicare without penalty at any time while you have job-based insurance and for eight months after you lose your job-based insurance or you (or your spouse) stop working, whichever comes first.
Can I choose the start date for Medicare Part B?
You can't always pick the date you want to start Part B coverage because the start date depends on what type of enrollment period you sign up in and when during the enrollment period you apply.
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
How do I decline Medicare Part B?
To disenroll, you're required to submit a form (CMS-1763) that must be completed either during a personal interview at a Social Security office or on the phone with a Social Security representative. For an interview, call the Social Security Administration at 1-800-772-1213, or your local office.
Do you have to enroll in Medicare Part B every year?
Do You Need to Renew Medicare Part B every year? As long as you pay the Medicare Part B medical insurance premiums, you'll continue to have the coverage. The premium is subtracted monthly from most people's Social Security payments. If you don't get Social Security, you'll get a bill.
Why was my Medicare Part B Cancelled?
Depending on the type of Medicare plan you are enrolled in, you could potentially lose your benefits for a number of reasons, such as: You no longer have a qualifying disability. You fail to pay your plan premiums. You move outside your plan's coverage area.
Can I drop Part B and add it later?
If you drop Part B coverage while covered by an employer's plan, you can sign up for Part B again during your Special Enrollment Period (SEP). You can enroll in Part B anytime that you're working (or your spouse is working) and covered by the employer – or union-based health insurance plan.
How do I add Part B to my Medicare online?
You can apply online (at Social Security) - select “Already Enrolled in Medicare” from the menu. Or, fax or mail your forms to your local Social Security office.
Does Medicare Part B have to start on the first of the month?
Part B (Medical Insurance) Generally, you're first eligible to sign up for Part A and Part B starting 3 months before you turn 65 and ending 3 months after the month you turn 65. (You may be eligible for Medicare earlier, if you get disability benefits from Social Security or the Railroad Retirement Board.)
Does Medicare B backdate coverage?
If you enroll in Social Security retirement benefits or Medicare benefits for the first time, and you're beyond your Initial Enrollment Period (IEP) in Medicare, your Part A benefits will be backdated up to 6 months from the month you initiate the enrollment, and you might incur tax penalties associated with excess HSA ...
You Always Need Part B If Medicare Is Primary
Once you retire and have no access to other health coverage, Medicare becomes your primary insurance. While Part A pays for your room and board in...
You Need Part B to Be Eligible For Supplemental Coverage
Medigap plans do not replace Part B. They pay secondary to Part B.Part B works together with your Medigap plan to provide you full coverage. This m...
Do I Need Medicare Part B If I Have Other Insurance?
Many people ask if they should sign up for Medicare Part B when they have other insurance. At a large employer with 20 or more employees, your empl...
Enrolling Into Part B on A Delayed Basis
If you have delayed Part B while you were still working at a large employer, you’ll still need to enroll in Part B eventually. When you retire and...
Do I Need Medicare Part B If I’M A Veteran?
Some people have 2 different coverages that they can choose independent of one another. Federal employees who can opt to use their FEHB instead of...
Most Common Mistakes Regarding Part B
The most common mistake we see is from people who confuse Part B and Medigap. Just this week, a reader on our Facebook page commented that she was...
What is the Medicare Part B special enrollment period (SEP)?
The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 month...
Do I qualify for the Medicare Part B special enrollment period?
You qualify for the Part B SEP if: you are eligible for Medicare because of your age or because you collect disability benefits. (People who have E...
How do I use the Part B SEP?
To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS...
What if an employer gives me money to buy my own health plan?
A note about individual coverage: you’ll qualify for an SEP if you delayed Part B because you had employer-sponsored coverage through a group healt...
How long do you have to enroll in Part B if you retire?
When you retire and lose your employer coverage, you’ll be given a 8-month Special Enrollment Period to enroll in Part B without any late penalty.
How much is Part B insurance?
Most people delay Part B in this scenario. Your employer plan likely already provides good outpatient coverage. Part B costs at least $148.50/month for new enrollees in 2020.
How much does Medicare pay for outpatients?
Your healthcare providers will bill Medicare, and Part B will then pay 80% of your outpatient expenses after your small deductible. Medicare then sends the remainder of that bill to your Medigap plan to pay the other 20%. The same goes for Medicare Advantage plans.
What happens if you opt out of Part B?
Be aware that if you opt out of Part B and then later decide to join, you will pay a Part B late penalty. You’ll also need to wait until the next General Enrollment Period to enroll, which means there could be a delay before your coverage becomes active. In my opinion, most Veterans should sign up for Part B.
Does Medigap replace Part B?
Medigap plans do not replace Part B. They pay secondary to Part B. Part B works together with your Medigap plan to provide you full coverage. This means you must be enrolled in Part B before you are even eligible to apply for a Medicare supplement.
Do you have to be enrolled in Part B for Medicaid?
When you are 65 or older and enrolled in Medicaid. All of these scenarios require you to be enrolled in Part B. Without it, you would be responsible for the first 80% of all outpatient charges. Even worse, your secondary coverage may not pay at all if you are not actively enrolled in Part B as your primary coverage.
Do all veterans qualify for VA?
Not all veterans qualify for VA coverage. Your length of military service and your discharge characterization affect your eligibility. If you plan to use VA healthcare coverage as your only coverage, be sure that you apply for VA coverage before your initial enrollment window for Medicare expires.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
What to do if your Social Security enrollment is denied?
If your enrollment request is denied, you’ll have the chance to appeal.
How long do you have to enroll in Part B?
There are two main times when you can enroll in part B when you are over 65 and covered by your employer’s insurance: 1 While your work coverage is still active 2 During the eight month period after your employer-based coverage ends or the employment ends, whichever occurs first.
What is the phone number for Medicare?
If you have an urgent matter or need enrollment assistance, call us at 800-930-7956. By submitting your question here, you agree that a licensed sales representative may respond to you about Medicare Advantage, Prescription Drug, and Medicare Supplement Insurance plans.
Can seniors over 65 delay Medicare?
Senior65 generally recommends those over 65 delay enrolling in Medicare Part B if they are offered coverage through work (including spouse’s work). We all want to stay clear of paying Medicare late-enrollment penalties while avoiding gaps in coverage. This is where Senior65 comes in to make sense of it all.
Does Medicare Part B start at the same time?
That way you can time it that when your work coverage ends, your Medicare Part B (and any supplemental or drug coverage you may purchase) all start at the same time. You should not have a gap when your work coverage has ended but your Medicare has yet to begin.
When do you get Part A and Part B?
You will automatically get Part A and Part B starting the first day of the month you turn 65. (If your birthday is on the first day of the month, Part A and Part B will start the first day of the prior month.)
What happens if you don't get Part B?
NOTE: If you don’t get Part B when you are first eligible, you may have to pay a lifetime late enrollment penalty. However, you may not pay a penalty if you delay Part B because you have coverage based on your (or your spouse’s) current employment.
What is the individual health insurance marketplace?
NOTE: The Individual Health Insurance Marketplace is a place where people can go to compare and enroll in health insurance. In some states the Marketplace is run by the state and in other states it is run by the federal government. The Health Insurance Marketplace was set up through the Affordable Care Act, also known as Obamacare.
Do you have to pay a penalty if you don't get Part A?
NOTE: If you don’t get Part A and Part B when you are first eligible, you may have to pay a lifetime late enrollment penalty. However, you may not pay a penalty if you delay Part A and Part B because you have coverage based on your (or your spouse’s) current employment.
When do you have to enroll in Medicare?
If you work for a smaller employer, you must enroll in Part A and Part B when you turn 65, and then Medicare pays claims first and your employer plan becomes your secondary insurance. Medicare has strict enrollment rules that affect people differently according to their circumstances.
When does the eight month special enrollment period start?
The eight-month special enrollment period starts at the end of the month in which you stop working or lose your employer insurance, whichever is first. Generally, people eligible for Social Security benefits do not pay for Part A.
How much does a premium increase for a 12 month period?
If you don't sign up within your initial enrollment period or a special enrollment period (whichever is appropriate to you), your monthly premium will permanently increase 10 percent for each 12-month period you were eligible but did not enroll.
When does the IEP start?
The seven-month initial enrollment period begins three months before the month of your 65th birthday and ends three months after that month. (So for example, if you turn 65 in April, your IEP begins Jan. 1 and ends July 31.)
Signing up for Medicare might make sense even if you have private insurance
Jeffrey M. Green has over 40 years of experience in the financial industry. He has written dozens of articles on investing, stocks, ETFs, asset management, cryptocurrency, insurance, and more.
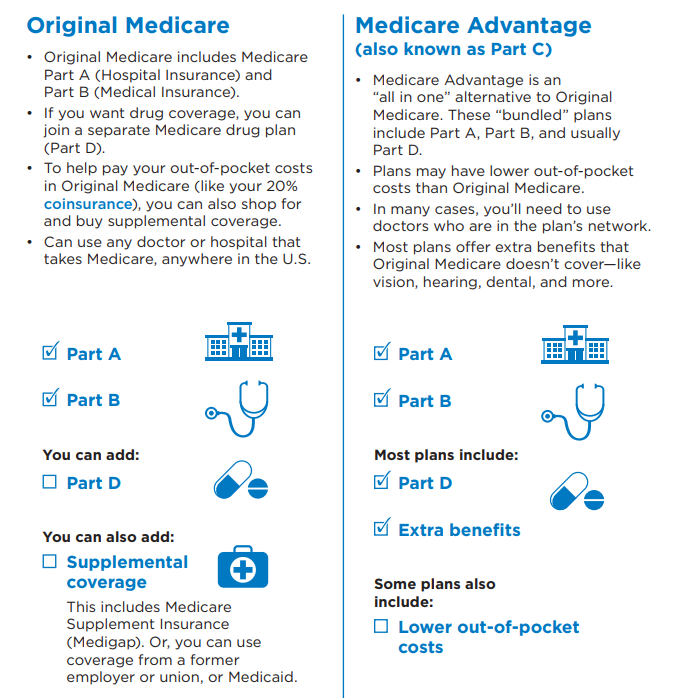
How Medicare Works
Before diving into how Medicare works with your existing health coverage, it’s helpful to understand how it works on its own. Medicare has four main parts: A, B, C, and D. You can also purchase Medicare supplement insurance, known as Medigap.
Medicare Enrollment Periods
Medicare has a few enrollment periods, but the initial enrollment period may be the most important. This is when you first become eligible for Medicare. And if you miss the deadline to sign up for Parts B and D, you could face expensive penalties .
How Medicare Works If You Have Private Insurance
If you have private insurance, you may want to sign up for Parts A, B, D—and possibly a Medicare Advantage plan (Part C) and Medigap, once you become eligible. Or not. There are reasons both for and against. Consider how the following types of coverage work with Medicare to help you decide.
Primary and Secondary Payers
Your Medicare and private insurance benefits are coordinated, which means they work together. Typically, a primary payer will pay insurance claims first (up to plan limits) and a secondary payer will only kick in for costs not covered by the primary payer.
Frequently Asked Questions (FAQs)
No, you can delay signing up for Medicare without penalty, as long as you are covered by another type of private insurance. Generally, if you are eligible for premium-free Part A, you should still sign up for it, even if you have additional private insurance coverage. 18
