
Medicare Part A is hospital insurance and is part of original Medicare. Generally speaking, you’re eligible for Part A if you’re age 65 or older, have a disability, or have ESRD or ALS. Some people will be automatically enrolled in Part A, while others will have to sign up.
What do Medicare Parts A, B, C, D mean?
Medicare parts A and B together are known as original Medicare. Medicare Part C plans cover everything that original Medicare does and often include additional coverage options. Medicare Part D is prescription drug coverage.
What does part a cover in Medicare?
- You are 65 or older and meet the citizenship or residency requirements.
- You are under age 65, disabled, and your premium-free Medicare Part A coverage ended because you returned to work.
- You have not paid Medicare taxes through your employment or have not worked the required time to qualify for premium-free Part A.
How do I know what Medicare plan I have?
- Review your Medicare plan coverage options. It’s a good idea to review your Medicare coverage every year to make sure the benefits of your Medicare plan remain aligned with your ...
- Make changes to your Medicare plan coverage during the right time of year. ...
- Find out what Medicare plan may fit your needs. ...
What is covered with Medicare?
Medicare provides benefits for:
- consultation fees for doctors, including specialists;
- tests and examinations by doctors needed to treat illnesses, such as x-rays and pathology tests;
- eye tests performed by optometrists;
- most surgical and other therapeutic procedures performed by doctors;
- some surgical procedures performed by approved dentists;
What makes a person eligible for Medicare Part B?
If you have a disability and are receiving Social Security or Railroad Retirement Board disability payments, you're eligible to enroll in Medicare Part B, regardless of your age.
How do you get Medicare Part C?
To be eligible for a Medicare Part C (Medicare Advantage) plan:You must be enrolled in original Medicare (Medicare parts A and B).You must live in the service area of a Medicare Advantage insurance provider that's offering the coverage/price you want and that's accepting new users during your enrollment period.
Can you have both Medicare Part A and B?
However, if you want to buy Medicare coverage and you want Part A, you also have to buy Part B. If you buy Part A and/or Part B (you must pay a premium for both), you must sign up during your Initial Enrollment Period, during a General Enrollment Period, or a Special Enrollment Period (see pages 11–13).
Do I have to pay for Medicare Part B?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Why do I need Medicare Part D?
If you're in the end stages of a life-threatening disease and under Medicare hospice care, Medicare Part A covers medications related to the terminal condition. If you need medications for anything not related to that condition, you will need to purchase Part D coverage.
What's the difference between Medicare Part C and D?
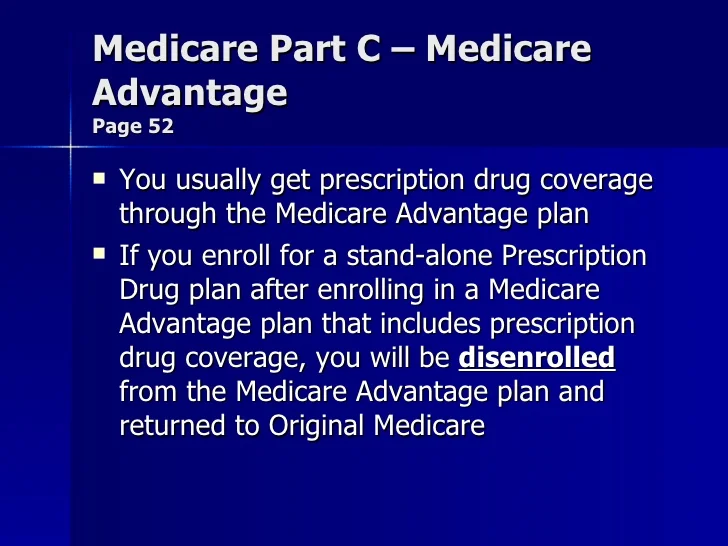
Medicare Part C is an alternative to original Medicare. It must offer the same basic benefits as original Medicare, but some plans also offer additional benefits, such as vision and dental care. Medicare Part D, on the other hand, is a plan that people can enroll in to receive prescription drug coverage.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
What is covered by Medicare Part C?
Medicare Part C outpatient coveragedoctor's appointments, including specialists.emergency ambulance transportation.durable medical equipment like wheelchairs and home oxygen equipment.emergency room care.laboratory testing, such as blood tests and urinalysis.occupational, physical, and speech therapy.More items...
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
How much does Social Security take out for Medicare each month?
In 2021, based on the average social security benefit of $1,514, a beneficiary paid around 9.8 percent of their income for the Part B premium. Next year, that figure will increase to 10.6 percent.
Does Medicare Part A cover 100 percent?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
Is Medicare deducted from your Social Security check?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
Why does Part A end?
There are special rules for when premium-free Part A ends for people with ESRD. Premium Part A and Part B coverage can be voluntarily terminated because premium payments are required. Premium Part A and Part B coverage ends due to: Voluntary disenrollment request (coverage ends prospectively); Failure to pay premiums;
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What is Medicare Part A?
Medicare Part A is hospital insurance and is part of original Medicare. Generally speaking, you’re eligible for Part A if you’re age 65 or older, have a disability, or have ESRD or ALS.
What are the eligibility requirements for Medicare Part A?
Medicare Part A eligibility requirements. To meet the basic eligibility requirements, you must be a citizen or permanent resident of the United States and also be one of the following: To receive coverage under Part A, you must be admitted as an inpatient at the hospital or other treatment center.
What is covered under Part A?
To receive coverage under Part A, you must be admitted as an inpatient at the hospital or other treatment center. If you’re not formally admitted as an inpatient, the services received will be considered outpatient care, which is covered under Part B.
How old do you have to be to get a Part A?
Typically, many people who enroll in Part A are age 65 and older. However, some specific groups of people younger than 65 years old may also be eligible for Part A. These groups include people with:
What happens if you don't buy Part A?
In this case, your monthly premium can go up by 10 percent. You’ll be subject to this higher premium for double the amount of years that you were eligible but didn’t enroll.
When is Medicare open enrollment?
Open enrollment: October 15 to December 7. During the annual open enrollment period, anyone with Medicare parts A and B can change to a Part C plan or add, switch, or remove a Part D plan. New coverage will begin on January 1.
When do you get Social Security if you are 65?
You’ll be automatically enrolled on the first day of the month you turn age 65 if you’ve been receiving these benefits at least 4 months before your birthday. You’re less than 65 years old and have a disability.
When do you enroll in Medicare Part A?
You’re automatically enrolled in original Medicare — which is made up of parts A and B — starting on the first day of the month you turn 65 years old.
How long do you have to be on Medicare if you are 65?
If you’re under age 65 and receiving Social Security or RRB disability benefits, you’ll automatically be enrolled in Medicare Part A when you’ve been receiving the disability benefits for 24 months. If you’re not automatically enrolled, you can sign up manually through the Social Security Administration.
What is Medicare Part A 2021?
Deductibles and hospital coinsurance. With Medicare Part A, you’ll also pay a deductible and coinsurance costs for each benefit period. In 2021, these costs are: Each day beyond day 90 is considered a lifetime reserve day. You have up to 60 of these days to use in your lifetime.
How much is the Part A premium for 2021?
If you or your spouse worked for 30 to 39 quarters, the standard monthly Part A premium cost is $259 in 2021. If you or your spouse for worked fewer than 30 quarters, the standard monthly Part A premium cost is $471 in 2021.
How old do you have to be to get Social Security?
You’re 65 years old and receive retirement benefits from Social Security or the Railroad Retirement Board (RRB). You’re 65 years old and you or your spouse had Medicare-covered health benefits from a government job. You’re under age 65 and have received Social Security or RRB disability benefits for 24 months.
What is Medicare for people over 65?
Medicare is a government healthcare program that cover s healthcare costs for people ages 65 and over or those with certain disabilities. The Medicare program is split into several sections, or parts. These include:
How long do you have to work to get Medicare?
If you’ve worked for at least 40 quarters — roughly 10 years — and paid Medicare taxes out of your paycheck, you won’t pay a premium for Medicare Part A. If you worked less than that amount of time, you will pay a monthly premium for Part A. Even if you don’t owe a premium, other costs are typically associated with services covered under Part A.
What happens if you don't enroll in Medicare B?
People who don’t enroll in Medicare B when first eligible are charged a late enrollment penalty that amounts to a 10 percent increase in premium for each year they were eligible for Medicare B but not enrolled.
How long does Medicare coverage last?
Medicare coverage begins as soon as your SSDI begins, and Medicare Part A has no premiums as long as you or your spouse (or parent, if you’re a dependent child) worked and paid Medicare taxes for at least 10 years.
How long do you have to pay Medicare taxes if you have end stage renal disease?
You have end-stage renal disease (ESRD) and are receiving dialysis, and either you or your spouse or parent (if you’re a dependent child) worked and paid Medicare taxes for at least 10 years.
How much is Medicare premium for 2020?
These premiums are adjusted annually. Everyone pays for Part B of Original Medicare. In 2020, the standard premium is $144.60/month for those making no more than $87,000 per year ($174,000 per year for married couples filing jointly). For 2020, the threshold for having to pay higher premiums based on income increased.
Do you have to pay Social Security premiums if you are 65?
You may also not have to pay the premium: If you haven’t reached age 65, but you’re disabled and you’ve been receiving Social Security benefits or Railroad Retirement Board disability benefits for two years. You have end-stage renal disease (ESRD) and are receiving dialysis, and either you or your spouse or parent (if you’re a dependent child) ...
Do you have to pay Medicare premiums?
A: Most Medicare-eligible people do not have to pay premiums for Medicare Part A. If you are 65 and you or your spouse has paid Medicare taxes for at least 10 years, you don’t pay a premium for Part A. You may also not have to pay the premium: If you haven’t reached age 65, but you’re disabled and you’ve been receiving Social Security benefits ...
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Does Medicaid cover nursing home care?
Medicaid also pays for nursing home care, and often limited personal care assistance in one’s home. While some states offer long-term care and supports in the home and community thorough their state Medicaid program, many states offer these supports via 1915 (c) Medicaid waivers.
