If you are covered under workers’ compensation due to a job-related injury or illness and are entitled to Medicare benefits, the workers’ compensation insurance provider will be the primary payer. There typically is no secondary payer in such cases, but Medicare may make a payment in certain situations.
Full Answer
How does Medicare work with my employer’s insurance?
If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways.
Can I get Medicare coverage if I’m still working?
You can get Medicare coverage if you’re still working. If you or your spouse work for a large employer that provides insurance, you can often put off enrollment without penalty. If you work for a company that has fewer than 20 employees, you must sign up for Medicare as soon as you are eligible.
Can I choose employer health benefits instead of Medicare?
Here are the rules for choosing employer health benefits instead of Medicare: If your employer has fewer than 20 employees, you must sign up for Medicare when you’re eligible or you may face a late enrollment penalty for Part B when you sign up later.
What happens if you have Medicare and workers comp?
Workers’ compensation and Medicare. If you have Medicare and file for workers’ compensation, workers’ compensation pays primary for any care related to your accident or injury. If workers’ compensation does not make a decision about paying your health care bills within 120 days, Medicare may make conditional payments.
Can you have employer coverage and Medicare at the same time?
Can I have Medicare and employer coverage at the same time? Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is Medicare primary or secondary to employer coverage?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Do employers pay for Medicare?
While your employer can't pay your Medicare premiums in the true sense, you'll be glad to know that they may reimburse you for your premium costs! To compensate you, your employer will need to create a Section 105 Medical Reimbursement Plan.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Can I keep my private insurance and Medicare?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Will Medicare pay my primary insurance deductible?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
Why is Medicare taken out of my paycheck?
If you see a Medicare deduction on your paycheck, it means that your employer is fulfilling its payroll responsibilities. This Medicare Hospital Insurance tax is a required payroll deduction and provides health care to seniors and people with disabilities.
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
How does working affect Medicare?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work. Generally, if you have job-based health insurance through your (or your spouse's) current job, you don't have to sign up for Medicare while you (or your spouse) are still working.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Who pays for Medicaid?
The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP).
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
Does Cobra pay for primary?
The only exception to this rule is if you have End-Stage Renal Disease and COBRA will pay primary. Your COBRA coverage typically ends once you enroll in Medicare. However, you could potentially get an extension of the COBRA if Medicare doesn’t cover everything the COBRA plan does like dental or vision insurance.
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
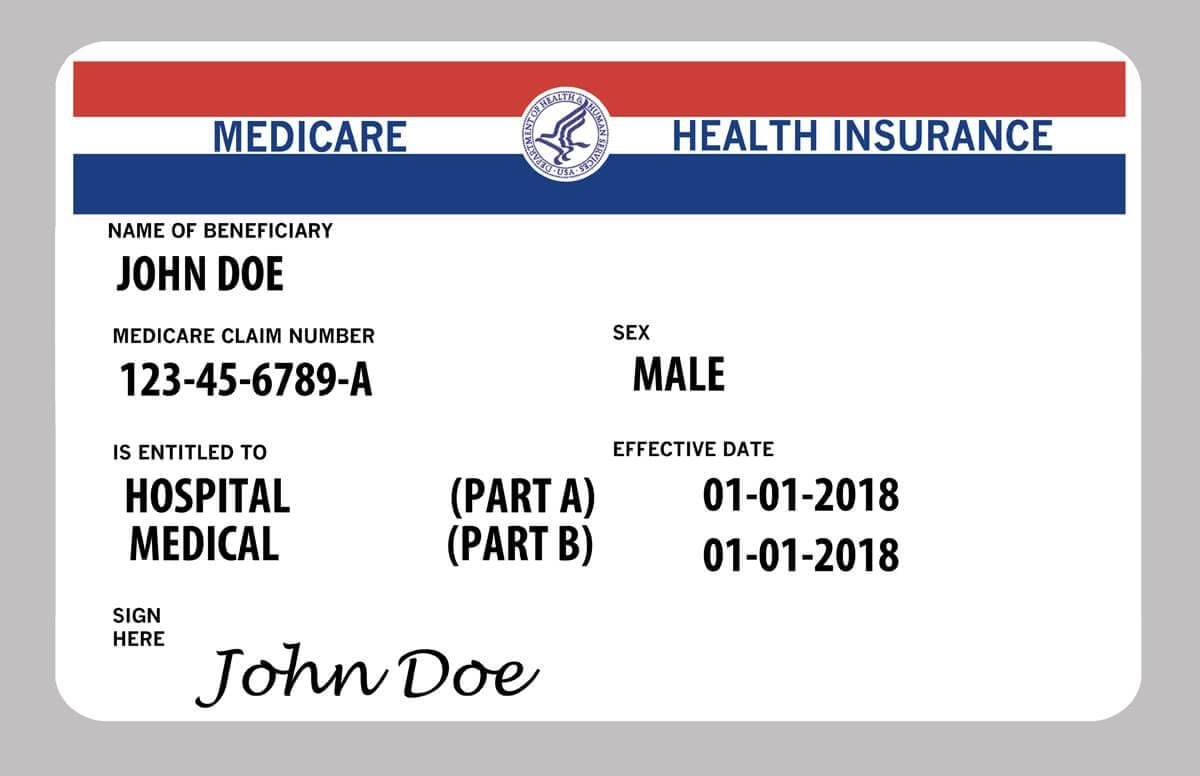
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
Is Medicaid a dual payer?
You are “dual-eligible” ( entitled to both Medicare and Medicaid ). Medicaid becomes the secondary payer after Medicare pays first. You are age 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has fewer than 20 employees.
How to determine if Medicare is primary or secondary?
Here’s how to know who the primary and secondary payers are in your situation: 1 Medicare is generally the primary payer if the company you work for has fewer than 20 employees. But Medicare becomes the secondary payer if your employer is part of a group health plan with other employers who have more than 20 employees. 2 Medicare is typically the secondary payer if the company you work for has 20 or more employees. In this case, your group health plan is the primary payer and Medicare pays out only after your employer’s plan has paid their portion.
What is the number to call Medicare?
If you’re not sure whether Medicare will be the primary or secondary payer in your situation, you can call 855-798-2627 to speak to someone at Medicare’s Benefits Coordination & Recovery Center.
How long do you have to enroll in Medicare after you retire?
Once you retire and give up your employer health benefits, you will have a special enrollment period of 8 months to enroll in Part A and Part B, if you haven’t enrolled already. This special enrollment period begins the month after your employment or group health plan ends. There is no late enrollment penalty for enrolling in original Medicare ...
How old do you have to be to get Medicare?
Although retirement age usually ranges from 66 to 67 years old, Medicare eligibility for most individuals begins at age 65. Some people who continue to work past age 65 may also have group health plan benefits through their employer. Because of this, it’s possible to have both Medicare and a group health plan after age 65.
What is the primary payer?
When you receive medical services, your primary insurance pays out first. This insurance is known as the primary payer. If there’s anything that your primary insurance didn’t cover, your secondary insurance pays out next. This insurance is known as the secondary payer.
Does Medicare cover dependents?
Medicare is individual health insurance coverage, which means that it doesn’t include coverage for spouses or dependents. Most group health plans, on the other hand, do include some sort of coverage option for dependents and spouses.
Does Medicare work with employer benefits?
Instead, they can work in conjunction. Medicare is meant to work together with employer benefits to cover your healthcare needs and help pay for most, if not all, of your medical expenses.
What factors affect your Medicare enrollment status if you are working?
Medicare is the federal health insurance program that covers people age 65 and older as well as some younger people with disabilities or specific health conditions. If you’re still working at 65 and covered by your employer plan, several factors will affect your Medicare enrollment status:
Is Medicare enrollment required for people who are still working?
It depends. As mentioned above, if you work for a company with fewer than 20 people, you’ll be expected to sign up for Medicare ( including Part D) as soon as your initial enrollment period rolls around. That period begins 3 months before your 65th birthday and continues for 3 months after the month you turn 65.
What are the benefits of getting Medicare while I am working?
If you’re unhappy with your current insurance, you might prefer the Medicare coverage. For example, your private health insurance may restrict you to a small network of doctors, while 99% of nonpediatric physicians accept Medicare. Switching to Medicare may also save you money on out-of-pocket costs versus your existing plan.
What are the drawbacks of getting Medicare while still working?
While Medicare Part A is free, Medicare Part B — which covers doctor visits and outpatient medical supplies — requires you to pay a monthly premium (in 2021, the premium is $148.50 per month for most enrollees; high earners may pay more).
How do I decide which approach is the most cost-effective for me?
When you have access to both an employer-based plan and Medicare, deciding on the most cost-effective approach to building insurance coverage takes a bit of work. To start, add up each plan’s out-of-pocket costs, including its premiums, deductibles, copays, and prescription drug costs.
Take our quiz
Navigating Medicare can be challenging, especially since different types of coverage won’t necessarily cover all of your expenses. Choosing to purchase additional coverage may help. Find out which supplemental coverage option is best for you, Medicare Advantage or Original Medicare with Medigap.
The bottom line
You can use Medicare while you’re still working. If you work for a large employer, the decision is typically up to you. To decide on the right approach, you’ll need to consider both plans’ costs and coverage.
Do I need to sign up for Medicare when I turn 65?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work.
How does Medicare work with my job-based health insurance?
Most people qualify to get Part A without paying a monthly premium. If you qualify, you can sign up for Part A coverage starting 3 months before you turn 65 and any time after you turn 65 — Part A coverage starts up to 6 months back from when you sign up or apply to get benefits from Social Security (or the Railroad Retirement Board).
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
How long does it take for Medicare to pay your health care bills?
If workers’ compensation does not make a decision about paying your health care bills within 120 days, Medicare may make conditional payments. A conditional payment is when Medicare temporarily pays in place of workers’ compensation.
What is workers compensation?
Register. Workers’ compensation is a state-administered program that pays for health care and other claims for job-related injuries. If you have Medicare and file for workers’ compensation, workers’ compensation pays primary for any care related to your accident or injury.
What is the number to call for workers compensation?
When you file a claim with your workers’ compensation insurer, you should also call the Medicare coordination of benefits contractor at 800-999-1118 and report the claim. If you plan to settle your workers’ compensation claim, it is important to set aside funds in a special account called a Workers’ Compensation Medicare Set-Aside Agreement.
Does Medicare have to be paid back after a workers compensation claim?
Then, once your workers’ compensation claim is settled or a final decision or award is reached, Medicare must be paid back for payments it made that were for services related to the accident or injury.
Signing up for Medicare might make sense even if you have private insurance
Jeffrey M. Green has over 40 years of experience in the financial industry. He has written dozens of articles on investing, stocks, ETFs, asset management, cryptocurrency, insurance, and more.
How Medicare Works
Before diving into how Medicare works with your existing health coverage, it’s helpful to understand how it works on its own. Medicare has four main parts: A, B, C, and D. You can also purchase Medicare supplement insurance, known as Medigap.
Medicare Enrollment Periods
Medicare has a few enrollment periods, but the initial enrollment period may be the most important. This is when you first become eligible for Medicare. And if you miss the deadline to sign up for Parts B and D, you could face expensive penalties .
How Medicare Works If You Have Private Insurance
If you have private insurance, you may want to sign up for Parts A, B, D—and possibly a Medicare Advantage plan (Part C) and Medigap, once you become eligible. Or not. There are reasons both for and against. Consider how the following types of coverage work with Medicare to help you decide.
Primary and Secondary Payers
Your Medicare and private insurance benefits are coordinated, which means they work together. Typically, a primary payer will pay insurance claims first (up to plan limits) and a secondary payer will only kick in for costs not covered by the primary payer.
Frequently Asked Questions (FAQs)
No, you can delay signing up for Medicare without penalty, as long as you are covered by another type of private insurance. Generally, if you are eligible for premium-free Part A, you should still sign up for it, even if you have additional private insurance coverage. 18
How long do you have to enroll in Medicare after you lose your employer?
NOTE: While you have eight months for Parts A & B, you only get two months after losing the employer coverage or leaving work to re-enroll in a Medicare Part D prescription drug plan or a Medicare Advantage (Part C) plan. If you enroll later, you’ll face late enrollment penalties for Part D.
What happens if you drop Medicare?
If you drop Medicare and don’t have creditable employer coverage, you’ll face penalties when getting Medicare back. Before you decide to drop any part of Medicare, there are some things you’ll want to think about, especially as some choices could end up being costly.
How long do you have to wait to enroll in Medicare after dropping it?
There are rules for re-enrolling in Medicare after you’ve dropped it for an employer-sponsored health plan. You’ll have an 8-month Special Enrollment Period in which to re-enroll in Medicare Part A and Part B. If you miss this window, you’ll have to wait to enroll in the Medicare General Enrollment Period (January 1 – March 31) ...
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.