Beginning in 2021, people with End-Stage Renal Disease (ESRD A condition characterized by a gradual loss of kidney function.Chronic Kidney Disease
Full Answer
When do you become eligible for Medicare with end stage renal disease?
Qualifying for Medicare with End-Stage Renal Disease Special consideration has been given to patients diagnosed with end-stage renal disease. You will become eligible for Medicare on the first day of your fourth month of dialysis treatment. However, if you begin a self-dialysis training program you can become Medicare-eligible immediately.
Does Medicare cover end-stage renal disease (ESRD)?
Receive updates about Medicare Interactive and special discounts for MI Pro courses, webinars, and more. Beginning in 2021, people with End-Stage Renal Disease (ESRD) can enroll in Medicare Advantage Plans. Medicare Advantage Plans must cover the same services as Original Medicare but may have different costs and restrictions.
How do you qualify for Medicare if you have kidney failure?
To be eligible, you’ll need a written diagnosis of kidney failure from a medical professional. You’ll need to be on regular dialysis or have had a kidney transplant. Medicare is only available for U.S. citizens or permanent residents who have lived here for at least 5 continuous years.
When does Medicare coverage end after a kidney transplant?
For example, if you get a kidney transplant that continues to work for 36 months, your Medicare coverage will end (unless you have Medicare based on your age or disability). If after 36 months you enroll in Medicare again because you start dialysis or get another transplant, your Medicare coverage will start right away.

Can a person with end-stage renal disease enroll in a Medicare Advantage Plan?
Beginning in 2021, people with End-Stage Renal Disease (ESRD) can enroll in Medicare Advantage Plans. Medicare Advantage Plans must cover the same services as Original Medicare but may have different costs and restrictions.
Why are ESRD patients eligible for Medicare?
Am I eligible for Medicare? One of these applies to you: You've worked the required amount of time under Social Security, the Railroad Retirement Board (RRB), or as a government employee. You're already getting or are eligible for Social Security or Railroad Retirement benefits.
Is Medicare primary for end-stage renal disease?
Medicare will be secondary under the ESRD provisions for 30 months. If Medicare was already the primary payer under the Working Aged or Disability guidelines immediately before the individual became eligible to enroll in Medicare because of ESRD, Medicare will remain the primary payer of benefits.
When does Medicare coverage start for ESRD?
When you enroll in Medicare based on ESRD and you're on dialysis, Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. For example, if you start dialysis on July 1, your coverage will begin on October 1.
What part of Medicare covers ESRD?
Important: You need Medicare Part B (and must pay the Part B premium) to get full ESRD benefits under Medicare, including outpatient and home dialysis.
How much is ESRD Medicare?
In inflation-unadjusted terms, total expenditures in Medicare FFS beneficiaries with ESRD increased from $28.0B in 2009 to $36.6B in 2018, or 30.7% (Figure 9.8).
When does Medicare ESRD coverage end?
If the beneficiary has Medicare only because of ESRD, Medicare coverage will end when one of the following conditions is met: 12 months after the month the beneficiary stops dialysis treatments, or. 36 months after the month the beneficiary had a kidney transplant.
When does ESRD Medicare end?
When will my Medicare coverage end? If you have Medicare only because of permanent kidney failure, Medicare coverage will end: 12 months after the month you stop dialysis treatments. 36 months after the month you have a kidney transplant.
Are dialysis patients eligible for Medicare?
People who need dialysis are not eligible to sign up for Medicare (Parts A and B) until the day they begin dialysis. Once they sign up, Medicare will be effective at the beginning of their fourth month of dialysis and will start paying for their treatment if they choose in-center hemodialysis.
What is a network provider?
A network is a group of doctors, hospitals, and medical facilities that work with a plan to provide services. Your costs are typically lowest when you use in-network providers and facilities. Before enrolling in a Medicare Advantage Plan, make sure your providers, including your dialysis facility, are in network.
Does Medicare Advantage cover dialysis?
Medicare Advantage Plans must cover the same services as Original Medicare but may have different costs and restrictions. However, Medicare Advantage Plans cannot set cost-sharing for either outpatient dialysis or immunosuppressant drugs higher than would be the beneficiary responsibility under Original Medicare.
When will ESRD be available for Medicare?
If you want to switch from original Medicare to a Medicare Advantage plan, you will be able to do so during the annual open enrollment period, which takes place from October 15 through December 7.
How long do you have to be on dialysis to qualify for Medicare?
citizens or permanent residents who have lived here for at least 5 continuous years. Your eligibility for Medicare will begin 3 months after the date you start regular dialysis or receive a kidney transplant.
How long does ESRD last?
If you only have Medicare because you have ESRD, your coverage will end 12 months after you stop dialysis treatment or 36 months after you have a kidney transplant.
What is ESRD in Medicare?
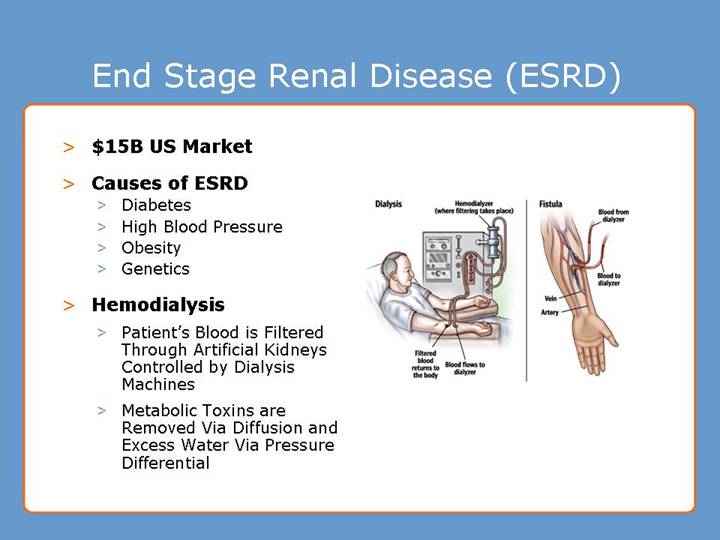
End stage renal disease (ESRD) is also known as permanent kidney failure. With this condition, your kidneys can no longer function on their own and you need regular dialysis or a kidney transplant. Medicare provides medical coverage for eligible people of all ages with ESRD.
How to prevent kidney failure?
Strategies include eating a heart-healthy diet, staying well hydrated, and limiting your salt intake. Kidney failure (ESRD) is the final stage of kidney disease. At this point, you will need dialysis or a kidney transplant.
How old do you have to be to qualify for Medicare?
If you’re younger than 65 years old. If you are an adult who has ESRD and are under 65 years old, you must meet one of the following criteria to be eligible for Medicare: you’ve worked the required amount of time (at least 40 quarters or 10 years)
Does Medicare cover all medications?
Some medications not covered under original Medicare are covered by Medicare Part D. Part D is an optional prescription drug plan you can purchase from an insurance company. Not all Part D plans cover the same medications, although every plan is required to provide a standard level of coverage established by Medicare.
How long does it take for Medicare to become primary payer for ESRD?
For ESRD patients who have an employer-sponsored health insurance policy in place in addition to Medicare, the private insurance will be the primary payer for the first 30 months, after which Medicare will become primary.
How long does it take for Medicare to cover ESRD?
The requirements for Medicare eligibility for people with ESRD and ALS are: ESRD – Generally 3 months after a course of regular dialysis begins (ie, on the first day of the fourth months of dialysis), but coverage can be available as early as the first month of dialysis for people who opt for at-home dialysis.
What is the Steve Gleason Act?
And in 2018, the Steve Gleason Act was approved as part of a budget bill, providing permanent Medicare funding of communication devices — including eye-tracking technology and speech generating devices — and the required accessories.
How long do you have to wait to get Medicare if you have ALS?
As with ESDR, if your disability is amyotrophic lateral sclerosis (ALS, or Lou Gehrig’s disease), you don’t have to wait 24 months for Medicare coverage. You can get Medicare as soon as you become entitled to SSDI.
When did Medicare start ESRD?
In 1972 the United States Congress passed legislation authorizing eligibility for persons diagnosed with ESRD under Medicare. The extension of coverage provided Medicare for patients with stage five chronic kidney disease (CKD), as long as they qualified under Medicare’s work history requirements. The ESRD Medicare program took effect on July 1, ...
Does Medicare cover kidney transplants?
Patients receiving a kidney transplant may also be qualified for Medicare coverage as soon as they become hospitalized for the transplant. For most enrollees, Medicare Part A has no premium, but Medicare Part B does have a premium ($148.50/month for most enrollees in 2021).
Is Medicare available for ESRD patients?
Medicare Advantage is newly available to ESRD patients as of 2021. ALS: You’re eligible for Medicare as soon as your SSDI benefits begin (and there’s no longer a waiting period for SSDI as of 2021). For people under 65 who have ALS or ESRD, access to Medigap plans varies from one state to another. Eligibility for Medicare includes persons ...
Can You Enroll in Medicare Advantage With ESRD?
As of January 2021, you can enroll in Medicare Advantage with ESRD. Here’s how it works.
Get started now
Interested in learning more about Medicare, Medigap, and Medicare Advantage plans? WebMD Connect to Care Advisors may be able to help.
When does Medicare pay first?
If you had ESRD Medicare first before becoming eligible for age or disability Medicare, any group health plan (GHP) coverage you have – meaning job-based, retiree, or COBRA coverage – pays first during the 30-month coordination period. After the 30-month coordination period, Medicare pays first.
What happens if you decline Part B?
If you declined Part B during your Initial Enrollment Period (IEP), you may have an LEP. Enrolling in ESRD Medicare waives your Part B LEP. You want to shorten the 24-month waiting period for Medicare due to disability. In general, you must collect Social Security Disability Insurance (SSDI) for 24 months before you are eligible for Medicare.
Does Medicare pay first after 30 months?
After the 30-month coordination period, Medicare pays first. If you enroll in ESRD Medicare after already having Medicare due to age or disability, you will still have a 30-month coordination period. However, Medicare and your GHP coverage are primary or secondary following standard coordination of benefits rules.
When does Medicare start covering kidney transplants?
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
When does Medicare start ESRD?
When you enroll in Medicare based on ESRD and you’re on dialysis, Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. For example, if you start dialysis on July 1, your coverage will begin on October 1.
How to replace blood?
You can replace the blood by donating it yourself or getting another person or organization to donate the blood for you. The blood that’s donated doesn’t have to match your blood type. If you decide to donate the blood yourself, check with your doctor first.
What is assignment in Medicare?
Assignment—An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare cover home dialysis?
Medicare Part B covers training for home dialysis, but only by a facility certifed for dialysis training. You may qualify for training if you think you would benefit from home dialysis treatments, and your doctor approves. Training sessions occur at the same time you get dialysis treatment and are limited to a maximum number of sessions.
Does Medicare cover dialysis for children?
Your child can also be covered if you, your spouse, or your child gets Social Security or RRB benefits, or is eligible to get those benefits.Medicare can help cover your child’s medical costs if your child needs regular dialysis because their kidneys no longer work, or if they had a kidney transplant.Use the information in this booklet to help answer your questions, or visit Medicare.gov/manage-your-health/i-have-end-stage-renal-disease-esrd/children-end-stage-renal-disease-esrd. To enroll your child in Medicare, or to get more information about eligibility, call or visit your local Social Security oce. You can call Social Security at 1-800-772-1213 to make an appointment. TTY users can call 1-800-325-0778.
Does Medicare cover pancreas transplant?
If you have End-Stage Renal Disease (ESRD) and need a pancreas transplant, Medicare covers the transplant if it’s done at the same time you get a kidney transplant or it’s done after a kidney transplant.