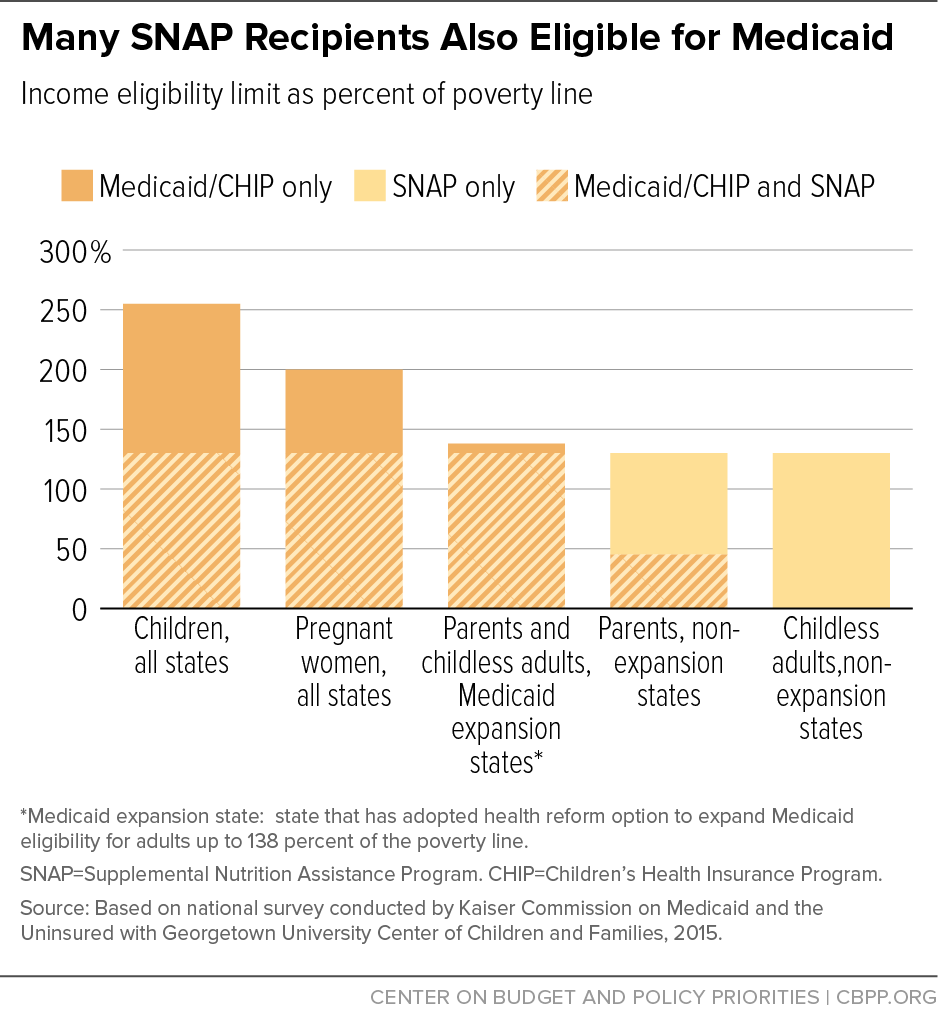
A study published in Annals of Internal Medicine led by UNC School of Medicine’s Seth A. Berkowitz, MD, MPH, shows that participation in the Supplemental Nutrition Assistance Program (SNAP) by older adults dually enrolled in Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
Will the Supplemental Nutrition Assistance Program (SNAP) increase in 2021?
The American Rescue Plan Act of 2021 signed by President Joseph R. Biden on March 11, 2021, extends increases to the Supplemental Nutrition Assistance Program (SNAP) maximum allotments from July 1, 2021, through Sept. 30, 2021.
How much money do you need for SNAP benefits?
Resources Households may have $2,250 in countable resources (such as cash or money in a bank account) or $3,500 in countable resources if at least one member of the household is age 60 or older, or is disabled. However, certain resources are NOT counted when determining eligibility for SNAP: A home and lot;
Are you eligible for SNAP benefits if you receive meals?
Normally you are not eligible for SNAP benefits if an institution gives you most of your meals. However, there is one exception for elderly persons and one for disabled persons: Residents of federally subsidized housing for the elderly may be eligible for SNAP benefits, even if they receive their meals at the facility.
Are there any exceptions to the SNAP benefits for the elderly?
However, there is one exception for elderly persons and one for disabled persons: Residents of federally subsidized housing for the elderly may be eligible for SNAP benefits, even if they receive their meals at the facility.
What is the highest income for food stamps?
SNAP/Food Stamps Gross Income and Maximum Benefits for Individuals and Families*Gross Monthly Income Limit If not Elderly or Disabled*Max Monthly F.S. Benefit for Everyone1 person: $2,265$2502 people: $3,052$4593 people: $3,839$6584 people: $4,625$8355 more rows
Are we getting extra food stamps this month in California 2022?
Extra Food Stamps for California – April 2022 Summary Each eligible household will only receive one emergency allotment per benefit month that emergency allotments are approved. Extra CalFresh benefits for April 2022 will be paid on May 14 or 21, 2022.
Are we getting extra food stamps this month in Delaware 2022?
Delaware will issue emergency food benefits to all SNAP households as outlined below. SNAP households will receive the next emergency food benefit on May 26, 2022. Households receiving the maximum base SNAP benefit for their household size will receive $95 in emergency food benefits.
How long will the increase in food stamps last in Washington state?
In June 2021, USDA Food and Nutrition Service approved Washington state's plans to extend P-EBT benefits through the summer months of July and August 2021 and include children under age 6.
How long will the increase in food stamps last in California 2021?
How long will the increase in food stamps last in California for 2021? Unlike the 15% increase in food stamps that was approved from January – September 2021, the 25% increase in food stamps for 2021 is permanent. This means that you will receive this benefit increase indefinitely if you qualify.
Will pandemic EBT be extended in California 2022?
Overview. Pandemic EBT (P-EBT) was a brand-new program implemented in 2020 in response to school closures caused by the COVID-19 pandemic. P-EBT has been extended through the 2021-2022 school year, the summer of 2022, and as long as the current public health emergency continues.
Will Delaware get extra food stamps this month of April 2022?
NEW CASTLE (April 26, 2022) – The Delaware Division of Social Services will issue emergency benefits for April to eligible households as part of the State's ongoing response to the COVID-19 public health emergency.
How long will the increase in food stamps last in Maryland 2022?
In April 2022 the Biden administration extended the federal emergency declaration due to the pandemic for an additional 90 days; therefore, the SNAP emergency allotment payments will continue through August - due to an automatic extra month provided by the program rules.
How long will the increase in food stamps last in Iowa 2022?
The program remains in effect for the summer of 2022, but will expire following the end of the COVID-19 public health emergency.
Will pandemic EBT be extended in Washington state?
Yes! Additional benefits may be issued to the card for as long as the COVID-19 public health emergency continues and we receive federal approval to extend the program.
How long will the increase in food stamps last in Washington State 2022?
Household and Individual Allotments Have Gone Up for 2022. In 2021, the USDA announced a cost of living adjustment (COLA) for SNAP in 2022. Here's what you need to know: For the 48 contiguous states and Washington, D.C., the maximum allotment for a family of four has been raised to $835 per month.
Can Washington EBT be used in another state?
Q: Can you use your EBT card out of state? A: The Washington QUEST card is accepted nationwide at retailers participating in the EBT program. Look for the QUEST sign or check with the store before trying to use your QUEST card.
How much can you deduct from your SNAP?
The following deductions are allowed for SNAP: A 20-percent deduction from earned income. A standard deduction of $167 for household sizes of 1 to 3 people and $181 for a household size of 4 (higher for some larger households and for households in Alaska, Hawaii, and Guam).
When will the SNAP program be extended?
Biden on March 11, 2021, extends increases to the Supplemental Nutrition Assistance Program (SNAP) maximum allotments from July 1, 2021, through Sept. 30, 2021.
What is the net income test?
However, a household with an elderly or disabled person only has to meet the net income test. Net income means gross income minus allowable deductions. Gross income means a household's total, non-excluded income, before any deductions have been made.
What is dependent care deduction?
A dependent care deduction when needed for work, training, or education. Medical expenses for elderly or disabled members that are more than $35 for the month if they are not paid by insurance or someone else. The excess medical expenses deduction is described below. In some states, legally owed child support payments.
What are the rules for SNAP?
Home. Supplemental Nutrition Assistance Program (SNAP) To get SNAP benefits, you must apply in the state in which you currently live and you must meet certain requirements, including resource and income limits. Most SNAP eligibility rules apply to all households, ...
How to contact a state agency for snap?
You can contact your state agency by visiting your local SNAP office, visiting your state agency’s website, or calling your state’s toll-free SNAP Information hotline.
How much is shelter deduction?
Some states allow a set amount for utility costs instead of actual costs. The amount of the shelter deduction is capped at (or limited to) $586 unless one person in the household is elderly or disabled. The limit is higher in Alaska, Hawaii, and Guam.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How does Social Security determine IRMAA?
The Social Security Administration (SSA) determines your IRMAA based on the gross income on your tax return. Medicare uses your tax return from 2 years ago. For example, when you apply for Medicare coverage for 2021, the IRS will provide Medicare with your income from your 2019 tax return. You may pay more depending on your income.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
How much do you need to make to qualify for SLMB?
If you make less than $1,296 a month and have less than $7,860 in resources, you can qualify for SLMB. Married couples need to make less than $1,744 and have less than $11,800 in resources to qualify. This program covers your Part B premiums.
Does Medicare change if you make a higher income?
If you make a higher income, you’ll pay more for your premiums, even though your Medicare benefits won’t change.
How much do you pay for Medicare after you meet your deductible?
After you meet your deductible for the year, you typically pay 20% of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How much is Part B deductible in 2021?
Part B deductible & coinsurance. In 2021, you pay $203 for your Part B. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. . After you meet your deductible for the year, you typically pay 20% of the.
What is the standard Part B premium for 2021?
The standard Part B premium amount in 2021 is $148.50. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
What is Medicare Part B?
Some people automatically get. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , and some people need to sign up for Part B. Learn how and when you can sign up for Part B. If you don't sign up for Part B when you're first eligible, ...
Do you pay Medicare premiums if your income is above a certain amount?
If your modified adjusted gross income is above a certain amount, you may pay an Income Related Monthly Adjustment Amount (IRMAA). Medicare uses the modified adjusted gross income reported on your IRS tax return from 2 years ago.
How much is the 2021 Medicare Part B deductible?
The 2021 Part B deductible is $203 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
When will Medicare Part B and Part D be based on income?
If you have Part B and/or Part D benefits (which are optional), your premiums will be based in part on your reported income level from two years prior. This means that your Medicare Part B and Part D premiums in 2021 may be based on your reported income in 2019.
What is Medicare Part B based on?
Medicare Part B (medical insurance) premiums are based on your reported income from two years prior. The higher premiums based on income level are known as the Medicare Income-Related Monthly Adjustment Amount (IRMAA).
Does Medicare Part D cover copayments?
There are some assistance programs that can help qualified lower-income beneficiaries afford their Medicare Part D prescription drug coverage. Part D plans are sold by private insurance companies, so additional costs such as copayment amounts and deductibles can vary from plan to plan.
Does income affect Medicare Part A?
Medicare Part A costs are not affected by your income level. Your income level has no bearing on the amount you will pay for Medicare Part A (hospital insurance). Part A premiums (if you are required to pay them) are based on how long you worked and paid Medicare taxes.
Does Medicare Part B and D have to be higher?
Learn more about what you may pay for Medicare, depending on your income. Medicare Part B and Part D require higher income earners to pay higher premiums for their plan.
Does Medicare Advantage have a monthly premium?
Some of these additional benefits – such as prescription drug coverage or dental benefits – can help you save some costs on your health care, no matter what your income level may be. Some Medicare Advantage plans even feature $0 monthly premiums, though $0 premium plans may not be available in all locations.
