How to enroll in a Medicare Advantage (Part C) plan
- Enroll in Medicare Part A and Part B first.
- Find insurance providers who offer Medicare Advantage plans in your area.
- Learn more about the plans available in your area by exploring them online or calling the provider directly.
- Find the plan that has the health care benefits you want and enroll with the plan provider—via...
Full Answer
Who qualifies for a Medicare Advantage plan?
- All-Dual
- Full-Benefit
- Medicare Zero Cost Sharing
- Dual Eligible Subset
- Dual Eligible Subset Medicare Zero Cost Sharing Who is eligible for a DSNP? ...
- You must be a United States citizen or have been a legal resident for at least five years.
- You must be 65 years old or have a qualifying disability if younger than 65.
How do I choose the best Medicare Advantage plan?
- Do your important physicians participate in any Medicare Advantage plans or do they only accept Original Medicare?
- What insurance is accepted by your preferred hospitals?
- Do you travel out of the area frequently? ...
- What is your risk tolerance? ...
- How about peace of mind? ...
Can anyone join a Medicare Advantage plan?
Usually, anyone who has Medicare Part A and Medicare Part B coverage can join a Medicare Advantage plan ( MA or MAPD) if the person lives within the plan's service area (Zip Code area).
How to sign up for a Medicare Advantage plan?
- Your job-based insurance pays first, and Medicare pays second.
- If you don’t have to pay a premium for Part A, you can choose to sign up when you turn 65 (or anytime later).
- You can wait until you stop working (or lose your health insurance, if that happens first) to sign up for Part B, and you won’t pay a late enrollment penalty.

How do I add a new provider to Medicare?
Enrollment ApplicationsEnroll as a Medicare provider or supplier.Review information currently on file.Upload your supporting documents.Electronically sign and submit your information online.
Which of the following are steps to becoming a Medicare provider?
Applying to become a Medicare providerStep 1: Obtain an NPI. Psychologists seeking to become Medicare providers must obtain a National Provider Identifier (NPI) before attempting to enroll in Medicare. ... Step 2: Complete the Medicare Enrollment Application. ... Step 3: Select a Specialty Designation.
How do I add a provider to Pecos?
0:146:13Medicare Provider Enrollment Through PECOS - YouTubeYouTubeStart of suggested clipEnd of suggested clipNumber if you do not already have an active NPI number you can register for one through the nationalMoreNumber if you do not already have an active NPI number you can register for one through the national plan and provider enumeration system or n Pez.
When can you enroll in a Medicare Advantage plan?
Sign up for a Medicare Advantage Plan (with or without drug coverage) or a Medicare drug plan. During the 7‑month period that starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65.
Does Medicare backdate provider enrollment?
When providers and suppliers enroll in Medicare, they are permitted to bill for services performed before the date of their enrollment approval—up to a point, Marting says. In other words, they're able to retroactively bill for their services if their 855 enrollment application is accepted.
Can providers and other health care professionals may enroll in the Medicare program and also be selected as a provider in a Medicare Advantage MA plan?
A. Beneficiaries must be entitled to Medicare Part A, enrolled in Part B, and live in the plan service area to be eligible to enroll in an MA Plan. Providers and other health care professionals may enroll in the Medicare Program and also be selected as a provider in a Medicare Advantage (MA) Plan.
What is Pecos enrolled mean?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.
How do I check if a provider is enrolled in Pecos?
To determine if you have a current enrollment record in the PECOS, you can do the following:Utilize the national file of Medicare physicians and non-physician practitioners who are eligible to order / refer and have current enrollment records in the PECOS. ... Utilize Internet-based PECOS.More items...•
How do I apply for a NPI number online?
Visit the NPPES website In the national plan and provider enumeration system website, navigate to the NPI webpage, and look under how to apply for an NPI for individual providers. Create a login through the identity and access management system.
How do I enroll in Medicare plan?
Once you understand the plan's rules and costs, here's how to join:Use Medicare's Plan Finder.Visit the plan's website to see if you can join online.Fill out a paper enrollment form. ... Call the plan you want to join. ... Call us at 1-800-MEDICARE (1-800-633-4227).
Who is the largest Medicare Advantage provider?
United HealthcareUnited Healthcare Nearly three-quarters (74%) of UHC's HMOs have no monthly premiums. All offer vision and hearing benefits and 95% offer dental coverage. UHC is the nation's largest health insurer, with nearly 49.5 million members, including more than six million Medicare Advantage members.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
What is Medicare Advantage?
Medicare Advantage is private insurance's counterpart to Original Medicare. It's a great alternative for receiving your Medicare coverage. Rather than purchasing individual components through Original Medicare, Medicare Advantage bundles benefits from Part A and Part B and can even include drug coverage, vision, dental, hearing, ...
When is the open enrollment period for Medicare?
There’s also a Fall Open Enrollment Period (October 15 through December 7) during which you may sign up. Learn about enrollment periods and when they apply to you.
How long does Medicare Advantage last?
If you’re new to Medicare, you’ll want to enroll in an MA Plan during your Initial Enrollment Period (IEP). This period lasts for seven months— three months before the month when you turn 65, and three months after.
How to add medication to a label?
Enter your medications one at a time. Be sure you type the name, dosage, and frequency exactly as they appear on the label. Then click “Done Adding Drugs."
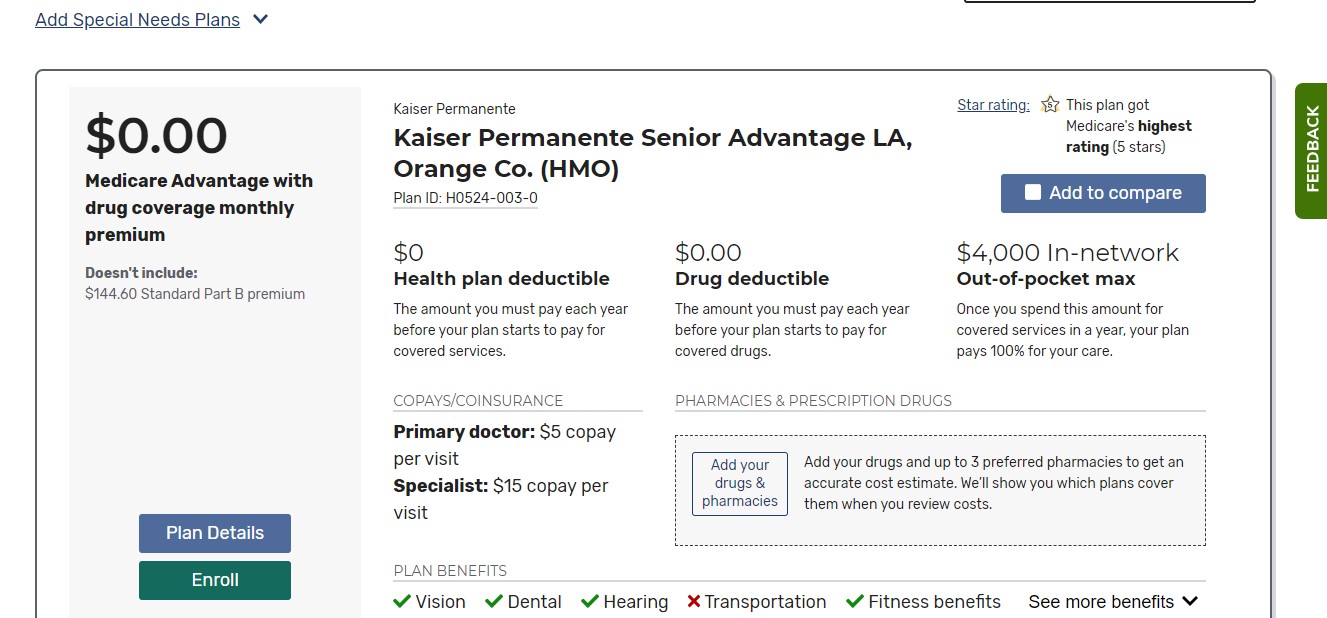
How to compare plans in a sandbox?
Select up to three plans you like best. Check the boxes next to"Add to compare" to select the plans you want to see head-to-head. Then click “Compare Plans” to see them side by side.
How to find my Medicare number?
Go to the Medicare Plan Finder. If you'd like to save your search results, choose the "Log in or Create Account" option and enter your Medicare number, email address, and other information. If you just want to do a quick search, select "Continue without logging in."
How many stars are there in Medicare?
Reference the Medicare Star Rating, from one to five. Avoid plans with a red warning icon—they’ve received poor quality ratings for three years in a row.
Medicare Advantage Enrollment Period
Whether you’re enrolling in Medicare Part C for the first time or want to make changes to an existing Medicare Advantage plan, there are many things to keep in mind. You’ll need to know if you qualify for an enrollment period, when your benefits will start, and what happens if you don’t meet the deadlines.
Can I enroll in a Medicare Advantage Plan anytime?
You can only enroll in a Medicare Advantage Plan during specific enrollment periods. If you are new to Medicare, we also have information about how to enroll in your Medicare Part A and B benefits and offer a comparison of Medicare Advantage vs. Original Medicare.
Do I have to enroll in Medicare Advantage every year?
You will be automatically re-enrolled in your Medicare Advantage plan annually – unless your insurer no longer provides the plan or you choose to switch plans. Then you can shop for a different plan during the Annual Enrollment Period.
How do I enroll in a Medicare Advantage plan?
We can help you find the right Medicare Advantage plan for your lifestyle and budget. We have tools to help you search for plans based on what’s important to you. Answer a few quick questions and we’ll provide a recommendation on the Medicare plan that matches you best.
How long does it take to get Medicare Advantage?
This is the period that begins three months before your birth month and ends three months after it. While there is no cost penalty for signing up at any time during this period, it is highly desirable to sign up as early in the period as possible. This is because any plan with a Part D component takes approximately three months to kick in, which means you could see a temporary gap in your drug coverage if you sign up any time after your birthday. This gap could last as long as three months after the time you lose the coverage you had before switching to Medicare, so it’s helpful to start your research before the ICEP and get the forms submitted prior to the first day of the month you turn 65.
What is Medicare Part A?
Medicare Part A is the basic coverage Medicare provides for its beneficiaries. This is a no-cost plan that covers the cost of inpatient hospitalization for eligible seniors. All U.S. citizens are automatically enrolled in Part A when they become eligible, since there is no out-of-pocket cost or monthly premium for this coverage. Services covered under Part A generally revolve around admissions to the hospital and treatments provided as part of regular inpatient care. Providers bill the Original Medicare program directly, which then pays for services according to a fixed or negotiated schedule. All Medicare-qualified providers are part of the Part A network, and they are required to bill only Medicare for covered services, unless the patient has a Medicare Advantage plan that provides the same coverage.
Can you enroll in Medicare Advantage outside of the normal enrollment period?
Sometimes circumstances force beneficiaries to enroll in Medicare Advantage outside of the normal enrollment periods. This can be tricky to do without incurring a penalty rate, but there are special circumstances you can invoke to justify an out-of-period enrollment. Examples of special circumstances include:
